![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
what is a a skin graft? how is it different from a flap?
|
segment of dermis and epidermis that is completely removed from one site and transferred to another. whereas flaps are living and have blood supply, grafts are essentially dead, and rely on neovascularization to survive
|
|
|
classification of skin graft according to their source
|
autograft: same animal
allograft: (homograft) different animal, same species xenograft: (heterograft) different species isograft: between identical twins or F1 hybrids |
|
|
cassification of grafts according to thickness
|
full thickness: epidermis and dermis
partial thickness: epidermis and split thickness dermis further classified as: thin, intermediate,or thick, according to how thick dermal layer is. |
|
|
what are island grafts
|
small pieces of skin implanted in large field
-process of coverage differs from sheet grafts in that islands rely mainly on migration of keratinocytes from the edges of islands also called seed grafts they include: pich, punch, strip, and stamp grafts |
|
|
primary indication for grafts i small animals
|
distal limbs where skin tight so no primary closure or local flaps
|
|
|
most common donor site in small animals:
|
cranial lower lateral thoracic area
|
|
|
3 most common causes of graft failure?
|
1. separation of graft from bed
2.infection: bacterial enzymes and fluid production 3.movement --disrupts fibrin bond that attaches bed to recip site |
|
|
particular bacteria that damage graft survival? how?
|
B hemolytic strept and Pseudomonas produce large amounts of plasmin and proteolytic enzymes which disrupt fibrin attachments
pseudomonas also has elastase which degrades elastin |
|
|
regarding bandaging, how often should bandages be changed?
|
every 12-24hrs to every 2-4days
immediate post op bandage should be left in place for 1-2days in order to facilitate adherence. some surgeons leave this inital bandage on for 3-5d--tobias authors DO NOT recommend this bandage changes at least 2-3 weeks post-op, after that light bandage for another 2 weeks--because process of rennervation of the graft can take several weeks |
|
|
how long does it take for reenervation of graft? what is significance of this?
|
in rate study sensation started to reurn 14 days post op, not complete until day 40. can have parasthesia so prone to self trauma so must be protected.
|
|
|
when do you see hairgrowth, what type of graft has best hair regrowth?
|
2-3 weeks, best with full thickness and unexpanded mesh grafts
|
|
|
what are power driven dermatomes?
|
instruments for graft harvest that control depth and can rapidly create uniform split thickness graft
available in electri and nitrogen driven |
|
|
how can grafts be meshed
|
with a blade or a meshing block.
an aluminum block with staggerred parallel rows of cutting blades |
|
|
how are seed grafts obtained?
|
suture needle, skin hook, or forceps to elevate skin, then cut with blade, or skin punch
|
|
|
where should grafts be placed
which is better? |
either healthy granulation tissue bed
OR acute wound with good blood supply studies report faster vascularization of grafts on fresh tissue than GT |
|
|
where will graft not take?
|
relatively avascular areas:
-stratified squamous epithelial tissues -heavily irritated tissues -avascular fat -poorly vascularized or hypertrophic GT -bone -cartilage -tendon -nerve -excessice/chronic inflammatory process in bed |
|
|
when should graft regeneration surpass degeneration?
|
seventh or eighth day
|
|
|
what are the 4 major steps of graft take?
|
adherence
plasmatic imbibition inosculation revascularization |
|
|
describe adherence
describe 2 phases |
soon after placement fibrin strands develop that contract and pull graft to bed
phase 1: attachment depends on fubrn stands which link collagen and elastin. fibrin polymerization results in increased strength. Greatest gain 8 hours post grafting. phase 2: begins at 72hrs. fibrinous network invaded by fibroblasts, WBCs, conversion to fibrous adhesion starts. continues until complete fibrous union by day 10. maturation results in contraction of graft |
|
|
is contraction more in thin or thick grafts?
|
thin split thickness
|
|
|
what is plasmatic imbibition, timeframe?
|
graft vessels spasm and constrict when harvested. fluid builds up between graft and bed as bed vessels leak. soon after placement in bed, graft vessels dilate, pulling fibrinogen-free serum and cells into graft via capillary action. this continues until graft is revascularized.
accumulation of Hb and breakdown products gives graft a cyanotic apearance absorbed fluid diffuses into interstitium of graft, produces edema. this peaks 48-72 hours post grafting vascular connection is established about this time, but venous drainage lags behind, so edema may increase graft returns to normal weight by 8th day post-op as lymphatics and veins improve. |
|
|
what is inosculation
|
the anastomosis of the cut ends of graft vessels with recient bed vessels of about same diameter.
can begin around 24 hours post, more commonly noted between 48-72 hours capillary buds for along fibrin network many make anastamoses but few survive connections can be initiated either way (graft to bed, bed to graft) anastamoses inhibits new capillary bud formation in bed. if separation of graft from bed occurs, this inhibition does not occur, and GT formation in bed continues initally flow is slow when blood begins to flow into the graft on day 3 or 4 post grafting, but resumes normal velocity by day 6 |
|
|
diagram of engrafting
|

|
|
|
describe the process of vascular ingrowth. which direction? rate?
|
grow from bed to graft
new capillary ingrowth at rate of 0.5mm/day initaially tortuous, then become arterioles VEGF most elevated 5-7d, peak ingrowth new lymphatics start day 4-5 |
|
|
describe the color changes and timeframe as grafts take
|
initially pale
first 2-3 days: purple/red as inosculation begins light red by 72-96 by day 7-8 entire graft is pink or red if took |
|
|
what happens if ontly partial thickness survives
|
if partial thikness take, may be darkly discolored becuse of ischemic necrosis of epidermis ,but vascularization of dermis. after epidermis sloughs or is debrided, dermis will re-epithelialize.
final appearance is sparsely haired epithelialized skin |
|
|
is reenervation better in partial or full thickness grafts?
|
better in full thickness
|
|
|
can you use split thickness grafts in cats?
|
not really because skin is so thin
|
|
|
how do you prepare wound bed for grafting?
|
chronic GT completely excised, replaced by acute healthy GT bed (day 4-5)
epithelium at wound edge is removed top of healthy GT bed can be scraped OR 0.5-2mm off top can be sharply excised defect covered with chlorohex soaked gause while graft developed let natural hemostasis occur in bed |
|
|
weck knife
|

goulian type uses disposable blade and has guard that slides over blade to fix depth
humby and watson are other types of knives razor blade can be used. |
|
|
what is good depth for split thickness graft
|
0.35mm thick (same thickness as scalpel blade)
|
|
|
when harvesting graft, how can you prepare donor site?
|
SQ saline to tent skin
|
|
|
name 4 good donor sites for grafts
|
lateral thorax
thoracolumbar region proximolateral forelimb lateral thigh |
|
|
how is the graft placed?
|
1. so that direction of hairgrowth will be same as surrounding tissues
2.graft may be cut to exact fit, but many surgeons like it to overlap the edges of wound bed by 1-2 cm. the overlapped portion will necrose and can be excised later 3. edges should be secured with sutures through graft in underlying skin 4. additional sutures in center to assure good adherence |
|
|
what can you do about hematomas under the graft
|
can be removed with q-tip under graft
thrombin or saline soaked solt to irrigate underneath graft before putitng on bandage after surgery (days) hematoma can be reomved by making an incision in the graft and milking it out, or q tip |
|
|
brown dermatome
|

|
|
|
for how long are immobilization splints usually necessary in limbs?
|
2 weeks
|
|
|
negative pressure wound therapy?
|
studies of split thickness grafts in people have shown improved percent graft survival compared with tie overs
|
|
|
name 2 main advantages of split thickness grafts, describe why
|
1.better viability
-study noted 89% survival vs. 58% for full thickness grafts on dog forelimbs -greater capillary density -less distance for for capillaries to traverse -shorter distance for diffusion, better plasmatic imbibition 2.less wound contraction -may be better if contraction would be big problem -there is actually expansion of the graft |
|
|
what are some disadvantages of split thickness grafts?
|
1.less durable
2. sparse hair growth 3. scaly appearance, may lack sebaceous glands 4.may require more specialized equipment |
|
|
what are 4 advantages of full thickness mesh graft?
|
drainage
conformity flexibility expansion |
|
|
what are 3 indications for mesh grafts?
|
1.allow drainage from a wound with minor exudate/bleeding
2.cover large skin defects when insufficient donor skin 3.reconstruct irregular surfaces |
|
|
preparing the mesh graft
|
after harvesting the skin from donor site (using template for measurements)
place on cardboard sq side up, stretched with hypodermic needles sq tissue must be removed-"defatting" meshing done with #11 blade incisions 1-2cm long, 0.5-2cm apart |
|
|
mesh expansion unit
|

aluminum block with stainless steel blades, graft placed on block and rolled with teflon or nylon roller
expansion occurs in only one directon depending on orientation of blades. |
|
|
best expansion ratio
|
3:1 or 4:1 for dogs and cats
|
|
|
is hyperbaric O2 therapy good for mesh grafts?
|
horse study: trend towards less granulation tissue and less edema, but more inflammation and less viability-
dogs study: -13% viable at 10d post grafting with O2 -concurrent admin of deferoxamine (O2 radical scavenger) improved survival to 65% still way less than expected some conflicting results i rats and pigs currently hyperbaric O2 contraindicated as adjunct therapy for grafts |
|
|
what are some advantages of mesh grafts, diasadvantages?
|
-excellent viability: 90-100% take when well cared for
-improved drainage -conformability -full thickness associated benefits -disadvantage: excess gt can grow through the slips and up over the graft |
|
|
what are the indications for full thickness unmeshed craft
|
where postgraft contraction might result in contracture (like distal limbs, joint surfaces)
small to moderate sized wounds wounds with minimal expected drainage/exudate |
|
|
drainage with full thickness grafts?
|
yes--small closed suction drains
--use butterfly needle to create drain --can also do stab incisions, but they tend to clot |
|
|
what is the diff between pinch and punch grafts
|
pinch: small pieces of skin cut free
punch: small pieces of skin cut with a punch biopsy |
|
|
indications for pinch/punch grafts
|
small limb wounds
contamnated wounds low grade infected wounds areas that dont need major durability irregular contour |
|
|
technique for punches
|

insert 5mm punch at angle of hair follicles
|
|
|
placement of pinch grafts--preparation of recipient bed
|
small slits are made in recipient bed, almost parallel to surface of the wound, openings upward
pockets are 2-4mm deep and 5-7mm apart apply direct digital pressure to keep it in its pocket |
|
|
placement of punch grafts
|
cylindrical holes 1-2cm apart
4mm punch used to make the holes. q-tip placed in holes for 5 minutes before graft placement for hemostasis |
|
|
outcome pinch grafts
|
thin epithelium, scaly, sparly haired, prone to injury
but take well |
|
|
what are strip grafts
|
5mm wide strips placed in parallel grooves cut in a GT bed. wounds that are parallel to long access on limb are good for these
|
|
|
what are stamp grafts?
|
chessboard grafs.
square patches-05-2cm per side no particular indication disadvantages are that may need to cut depressions into GT to keep the grafts from moving or being disturbed by the bandage, and these may bleed alot because of size of grafts. |
|
|
what are paw pad grafts?
|
small segements of full thickness pad tissue --placed into areas of GT that have formed in an absent metatarsal or metacarpal pad.
after grafter, healing via contraction, epithelialization, and hyperplasia forms a durable weight bearing tissue. indicated when phalangeal fillet wont work tough in large breed active dogs grafts are taken as rectangles from other paw pads, and secured into GT bed by 4-0 suture on the corners |
|
|
paw pad grafts, aftercare
|

donute to take pressure off pad, two mason metasplints incorporated over cast padding
|
|
|
what is the two stage technique for pad grafting?
|
-option when paw has sustained severe damage requiring amputation of digits at metacarpaophalangeal joint.
Step 1: pad grafts are harvested and implanted in the lateral thoracic area-each graft is sutured to cutaneous trunci mm. bandaged for 7 days, Step 2: bipedicle pouch flap containing grafts is elevated and animals paw is wrapped in flap the advantage of this technique is that SQ layer of graft can replace the fibroelastic pad tissue. |
|
|
what types of mucosal grafts have been described in small animal medicine
|
nicititans,
hypoplastic prepuce, conjunctival replacement nasal passage urethroplasty |
|
|
where can mucosal grafts be placed?
|
GT bed,
acute wound bed dermal side of freshly raised transposition flap? |
|
|
how would you prepare nasal passages for grafting?
|
place silicone stents to encourage tubular formation of GT
|
|
|
where are mucosal grafts harvested from?
|
buccal or sublingual mucosa
|
|
|
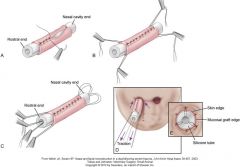
how do you do a conjunctival replacement
|
graft sutured to dermal side of transpoition flap that will be used to reconstruct eyelid. then flap returned to its original position for 4-7 days, then eslevated, transposed, and sutured into defect
|
|
|
how do you do a nasal mucosa replacement?
|
10 days after silicone tubes are placed, they are removed.
mucosal grafts are sutured with submucosal side out!! around the tubes, with traction sutures placed. tube is inserted, and graft and tube are sutured into place. sutures are placed through skin and graft to create new mucocutaneous junction at rostral end. tube acts as stent--removed at 7 days. |
|
|
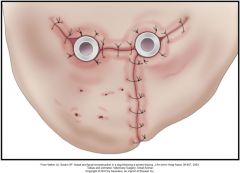
nasal mucosa reconstruction
|
|
|
|
conjuntival reconstruction
|

|
|
|
advantages and disadvantages of mucosal grafts
|
thin, easily vascularized, heal quickly
shrink alot, can shrivel, very delicates, difficult to handle |
|
|
preputial graft
|
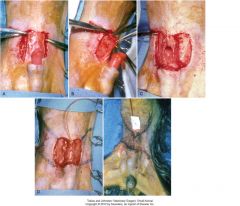
A mucosal graft was previously applied to a wound bed that was created by removing abdominal skin at the cranial aspect of a hypoplastic prepuce. The penis protrudes from the prepuce. After the graft has healed, the lateral and cranial edges of the mucosal graft are incised (A), and the graft is undermined to mobilize it (B). The dissection plane is kept deep to preserve the blood supply. C, The lateral edges of the graft are being sutured together around the penis to form a lining for the preputial extension. D, Completed suturing of the mucosal graft lining. Bilateral single-pedicle advancement skin flaps will be advanced to cover the mucosal graft lining. E, Skin flaps sutured together over the mucosal lining.
|

