![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
This lecture goes over the pathophysiology of viral infections in which locations?
|
-nose and throat
-larynx and trachea -large bronchi -bronchioles |
|
|
What are the four major viral respiratory pathogens discussed in this lecture?
|
1.) rhinovirus
2.) parainfluenza virus 3.) influenza virus 4.) respiratory syncytial virus |
|
|
Go over the epidemiology of respiratory tract infections: -adults infected / year vs. children infected per year
-amount of restricted activity days/ year -percent of infections caused by viruses |
adults: 1-4 infections per year
children: 6-8 infections per year influenza-like illnesses result in 400 million days of restricted activity/ year 65-75% caused by viruses (more than 200 viruses from 10 distinct genera) |
|
|
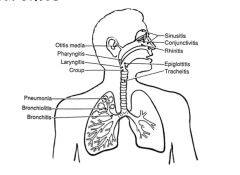
What is a major determinant of clinical manifestations?
|
anatomical location
|
|
|
There are overall twelve different clinical manifestations linked to specific areas in the body. can you list them?
|
|
|
|
Depending on causative agent, different clinical manifestations of respiratory infection can occur. list problems caused by viruses, bacteria, and fungi:
|
viruses: upper respiratory tract
bacteria: (OSEP): otitis media, sinusitis, epiglottitis, pneumonia fungi and protozoa: important cause of pneumonia in the immunocompromised |
|
|
There are 5 anatomic locations of infection and each is associated with common pathogens. Give the list of infection location to pathogen:
|
Nasopharynx: rhinovirus, coronavirus, other respiratory viruses
Oropharynx: Group A streptococcus, EBV, adenovirus, HSV, enterovirus Middle Ear and sinuses: Strep pneumonia, H. influenzae, moraxella catarrhalis Bronchi: strep pneumonia, H. influenza, mycoplasma pneumoniae and influenza Bronchioles: RSV |
|
|
Give a list of the most common illnesses associated with respiratory viruses:
|
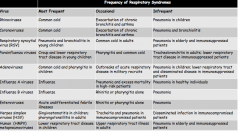
|
|
|
Infections of the nose and the throat: five aspects of pharyngitis:
|
1.) infection of the oropharynx
2.) discomfort in throat, especially during swallowing 3.) nasal symptoms may also be present 4.) viruses more common than bacteria 5.) viral pharyngitis can NOT be distinguished from bacterial pharyngitis on clinical grounds (culture for Group A Streptococcus); |
|
|
Infections of the nasopharynx: 3 important aspects:
|
1.) most are viral
2.) lead to signs and symptoms associated with the common cold 3.) primary etiology is the rhinovirus |
|
|
Draw a table listing the etiological pathogens associated with the common cold: 9 pathogens total/ with established % of cases and peak season
|
pathogens:
rhinovirus: (30-50%); all seasons coronavirus (10-15%); winter influenza (5-15%); winter the 5 5% ers'! RSV (5%; winter) parainfluenza: autumn/ spring enterovirus: summer adenovirus: all seasons HMPV: winter |
|
|
What are important points concerning the epidemiology of the common cold?
|
-very common infections (adults = 1 infection/ year; children and parents: 3-5 infections / year)
-occurs during the fall and the spring -multiple serotypes of rhinovirus circulate (102 serotypes exist) infected humans are the only reservoir TRANSMISSION: contamination of hands and direct contact with mucus membranes; cold temperatures and fatigue = not associated |
|
|
Give a sample flowchart for the transmission of a rhinovirus:
|
1.) nasal secretions of infected person --> hand of infection person --> direct or fomite such as telephone --> hand of susceptible person --> nose or eyes of susceptible person --> viral replication in nasal mucosa
|
|
|
Describe four important points in the pathogenesis of the common cold:
|
1.) small innoculum is sufficient to initiate an infection
2.) virus binds to specific receptors on respiratory cells: a.) 91 serotypes use ICAM-1 b.) 10 serotypes use LDL-R c.) 1 serotype uses Decay-accelerating factor NOTE: there is spread to the respiratory epithelium by local extension AND the posterior pharynx is the site of the most intense infection viremia/ infection of sites OUTSIDE the respiratory tract does not occur |
|
|
WHAT IS THE MECHANISM of symptom production in the common cold? (leads to sneezing/sore throat; rhinorrhea; cough, nasal obstruction)
|
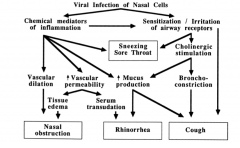
viral infection of nasal cells:
a.) chemical mediators of inflammation: b.) sensitization and irritation of airway receptors: |
|
|
How do you prevent the common cold?
|
a.) immunity against only the serotype affecting
-antibody blocks attachment to cellular receptor b.) vaccine is not feasible: -serologic diversity in rhinoviruses -rhinoviruses account for only 50% of colds |
|
|
How do you treat the common cold once you have it?
|
NOTHING really: no approved antivirals; medications for symptomatic treatment do not alter course of illness
-other therapies (zinc, echinacea, vitamin C = no benefit) |
|
|
INFECTIONS OF THE LARYNX AND THE TRACHEA: CROUP list five important characteristics of croup:
|
1.) obstruction of upper airway with sudden onset of a barking cough, difficulty breathing, and stridor
2.) almost all cases = PARAINFLUENZA VIRUSES ---> croup = parainfluenza 3.) usually preceded by 1-3 days of nasal discharge and dry cough 4.) self-limited: resolves in 3-7 days 5.) In adults: manifestation is usually hoarseness |
|
|
Differentiate between croup and epiglottitis:
|
croup: viral, effects airway below the vocal cords; inspiratory stridor
epiglottitis: bacterial (primarily Hib); effects the epiglottitis; and muffled voice with drooling |
|
|
three important points for the pathogenesis of croup:
|
1.) virus spreads by direct extension
2.) no viremia or infection OUTSIDE the respiratory tract 3.) histamine and IgE antibodies to parainfluenza virus are found in nasopharyngeal secretions (therefore, immunologic mechanisms involving inflammatory mediators may be involved in pathogenesis) |
|
|
pathogenesis of upper airway obstruction in croup: 4 different points:
|
1.) edema of the tracheal mucus membrane
2.) tracheal wall has nonexpandable rings of cartilage 3.) mucus membrane swelling results in narrowing of tracheal lumen 4.) worsens during inspiration resulting in inspiratory stridor |
|
|
Therapy of croup:
|
1.) supportive care
2.) to reduce edema and relieve airway obstruction use oral corticosteroids and inhaled epinephrine |
|
|
INFECTION OF THE LARGE BRONCHI: etiology of bronchial infections: What is the most common agent and three other agents:
|
influenza is the most common viral agent
may be also caused by mycoplasma, other viruses, and bacteria (i.e. in patients with COPD) |
|
|
INFLUENZA: general features and demographics of influenza:
affects on adults vs. young and elderly -amount of money spent in the US: |
-a major epidemic disease in developed countries
-a relatively mild disease in normal adults but significant mortality in elderly and immunocompromised -toll of influenza in the US: -25 million physician visits -125,000 hospitalizations, 25,000 deaths ; 2.5 billion in medical costs |
|
|
Influenza virus features: the three types and what is the outer coat made of?
|
three serotypes A,B,C:
-neuraminidase and hemagglutinin proteins which determine virulence |
|
|
classification scheme: how are new strains named?
|
TYPE/ CITY or country of first isolation/ Recovery year/ subtypes
|
|
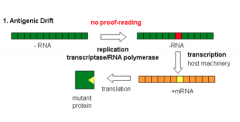
Antigenic drift: Describe some features of antigenic drift?
|
-influenza types A and B
-modest variations (point mutations) in hemagglutinin and neuraminidase genes -antigenic profile changes may compromsie vaccine and immune system efficacy -annual evaluation of circulating influenza and vaccine reformulation updates antigenic profile -responsible for annual epidemics |
|
|
Antigenic shift: describe some features of antigenic shift?
|
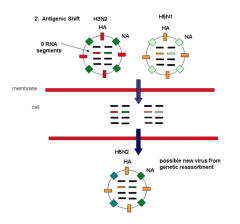
-only influenza type A;
-profound variation in hemagglutinin or neuraminidase structure -mixture of genes from diff. virus strains through genetic reassortment -animals are likely reservoirs for genes for new strains -new virus with novel antigenic profile -compromised vaccine and immune system efficacy -PANDEMIC consequences |
|
|
Transmission of influenza:
|
inhalation of large and small aerosols caused by coughs or sneezes
|
|
|
epidemiology of influenza (2 different slides); list some important features in the epidemiology
|
-occur in US on an annual basis
-late fall to late winter -most outbreaks are mild and sporadic -every few years there are severe epidemics -pandemics (frequent disease worldwide): occur rarely: 1918, 1957, 1968, 2009) |
|
|
Define endemic, epidemic, and pandemic
|
endemic: (sporadic): most of the population is immune
epidemic: antigenic drift has led to a large number of nonimmunes pandemic: antigenic shift leaves nearly all persons susceptible |
|
|
What parts of the respiratory tract does influenza infect and what happens when person has partial immunity to neuraminidase?
|
-infects upper and lower respiratory tract cells
-partial immunity to neuraminidase may confine infection to upper respiratory tract |
|
|
What does the destruction of ciliated bacteria provide a foothold for?
|
-for superinfecting bacteria;
-secondary bacterial pneumonia; usually lobar and pneumococci, staphylococci, and H. influenzae |
|
|
Draw a flowchart outlining the viral infection and lysis of respiratory epithelial cells:
|
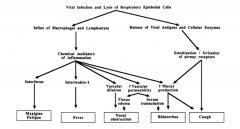
|
|
|
Comparison of common cold versus the flu in 9 different subpoints:
|
1.) fever: cold (rare in adults and common in children); flu (usually 1-2 but up to 104 and lasts 3-4 days)
2. headache: cold (rare) and flu (sudden onset and can be severe) 3.) muscle aches: cold (mild) and flu (usual and often severe) 4.) tiredness and weakness: cold (mild) and flu (last two or more weeks) 5.) extreme exhaustion: cold (never) and flu (sudden onset) 6,7,8: runny nose, sneezing, and sore throat features of common cold/ flu only sometimes 9.) COUGH: (common cold : mild hacking) and flu = usual and can become severe |
|
|
Diagnosis of influenza: 3 different ways:
|
1.) on epidemiologic grounds
2.) on viral culture 3.) rapid viral assays (EIAs and PCR) |
|
|
treatment of influenza:
|
supportive care
-antivirals: RAN: (zo) rimantidine and amantidine: prophylaxis and treatment ; influenza A only neuraminidase inhibitors: zanamivir (inhaled) and oseltamivir (oral) -treatment and prophylaxis: influenza A and B |
|
|
influenza vaccines approved in the US:
|
vaccines contain three viral strains (usually 2 type A and 1 type B); composition changed annually to reflect current strains; this year = h1n1 and H3n2 and a b strain
1.) trivalent inactivated vaccine (intramuscular injection) 2.) live attenuated vaccine (intranasal administration) |
|
|
INFECTIONS OF THE BRONCHIOLES: bronchiolitis:
|
-airway obstruction with wheezing and air trapping
-most commonly caused by respiratory syncytial virus |
|
|
6 different pathogens and associated relative importance of each: for bronchiolitis:
|
RSV: +++
parainfluenza 3: ++ parainfluenza 1: + parainfluenza 2: + adenovirus + influenza + |
|
|
epidemiology of RSV:
|
seasonal disease: epidemics every winter
-almost all children are infected but only 1% need hospitalization -humans = only reservoir -risk groups: congenital heart disease, immunodeficiency, chronic pulmonary disorders |
|
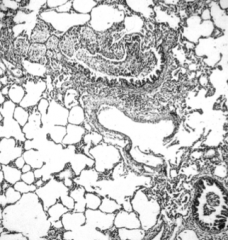
What is this a picture of and why does it happen?
|
-pathogenesis of RSV bronchiolitis
-necrosis of epithelial cells lining small bronchioles -increased mucus secretion, inflammation, and edema |
|
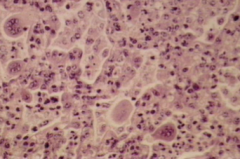
What is this a picture of?
|
-pulmonary infiltrates for RSV pneumonia
-alveolar involvement with swelling of alveolar lining cells and interstitial inflammation |
|
|
Other aspects of pathogenesis of RSV:
|
-transmission occurs by direct contact with infected secretions
-spread occurs cell-cell down the respiratory tract -no extra respiratory disease occurs -self limited and can cause bronchiolitis and pneumonia |
|
|
Draw a flowchart for the pathogenesis of bronchiolitis:
|

|
|
|
Treatment of RSV infections:
|
-
|
|
|
Treatment of RSV infections:
|
-usually a self-limited illness
-primarily supportive with oxygen and hydration -bronchodilaters are sometimes useful -steroids are NOT effective in randomized trials antiviral: ribavirin by inhalation (rarely given) |
|
|
Prevention of RSV infection: what prophylaxis is used and what vaccine is under development?
|
-prophylaxis with anti-RSV monoclonal antibody (palivizumab) in high risk infants
premature infants and infants < 2 with COPD and congenital heart disease also live attenuated cold-adapted vaccine is under way |

