![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back

What is the chemical composition of urine? |
Human urine consists primarily of water, with organic solutes including urea, creatinine, uric acid, and trace amounts of enzymes, carbohydrates, hormones, fatty acid, pigments such as urochrome, uroerythrin, and urobilin. Mucins, and inorganic ions such as sodium (Na+), potassium (K+), chloride (Cl-), magnesium (Mg2+), calcium (Ca2+), ammonium (NH4+), sulfates (SO42-), and phosphates (e.g., PO43-). |
|
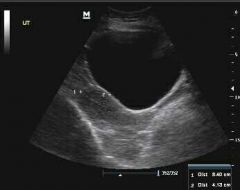
How much urine can the bladder hold? |
A healthy bladder can hold one and a half to two cups (300-400mls) of urine during the day and about four cups (800mls) at night. Photo shows a full bladder on ultrasound. |
|
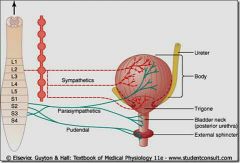
What nerves supply the bladder? |
• Parasympathetic nerves from the S2, S3 and S4 levels of your spinal cord cause the upper part of your bladder to contract and your bladder neck to relax, assisting in the process of micturition (urination). • Sympathetic nerves from the T11-L2 levels of your spinal cord do the opposite, causing the upper section of the bladder to relax and the bladder neck to contract, ensuring you can store urine. The nerves that control your urethral sphincter can be described as follows: • Parasympathetic nerves from the S2, S3 and S4 levels of the spinal cord control the internal sphincter, causing it to relax to allow urine to pass out of the bladder. • Sympathetic nerves from the T11-L2 levels of the spinal cord cause the internal urethral sphincter to tighten, helping to hold stored urine in the bladder. |
|
|
What do calcium oxalate crystals look like under the microscope? |
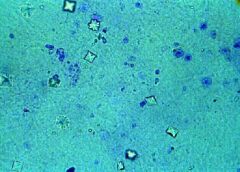
They look like the back of an envelope or an X in the box. |
|
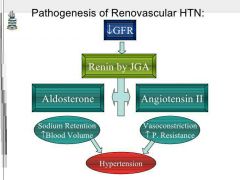
What is the most common cause of secondary hypertension? |
Renovascular hypertension. |
|
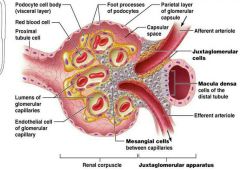
What do the juxtaglomerular cells of the afferent arteriole do when a decrease in blood pressure or sodium is detected? |
The juxtaglomerular cells react by releasing the enzyme renin and the enzyme renin activates angiotensinogen from the liver, when renin reacts with angiotensinogen it produces a peptide called angiotensin 1 and when it circulates through the lungs it is then changed to angiotensin 2 by the angiotensin converting enzyme(ACE) and finally aldosterone is secreted to increase sodium absorption. This whole process increases blood pressure. |
|
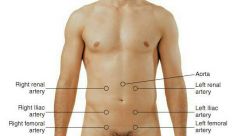
What is the most common clinical finding in renovascular hypertension? |
Abdominal bruit. Bruits are "swishing" sounds heard over major arteries during systole or, less commonly, systole and diastole. The area over the aorta, both renal arteries. and the iliac arteries should be examined carefully for bruits. |
|
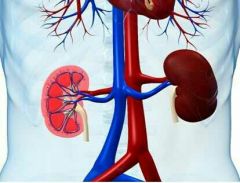
Why is the left kidney higher than the right? |
The left kidney is located slightly more superior than the right kidney due to the larger size of the liver on the right side of the body. Unlike the other abdominal organs, the kidneys lie behind the peritoneum that lines the abdominal cavity and are thus considered to be retroperitoneal organs. |
|
What are the functions of the urinary system? Where are the kidneys located? |
The urinary system gets rid of toxins, controls the levels of ions in the body, controls the amount of water in the body, controls the pH of the blood, plays a role in blood pressure regulation, and controls red blood cell production.
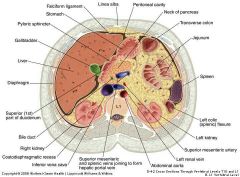
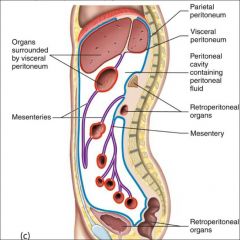
When looking at cross section of an abdomen, the first thing you should notice is the large organ-filled cavity anterior to the kidneys. That is the peritoneal cavity. Its outer membranous boundary, the parietal peritoneum, lies over the kidneys. It is composed of a serous membrane which secretes a small amount of fluid into the cavity. Most of the abdominal organs (liver, spleen, pancreas, stomach, for example) are housed in the peritoneal cavity. Notice, however, that the kidneys are not. As a result, they are called retroperitoneal organs. |
|
What is the visceral peritoneum? |
The organs that are housed within the peritoneal cavity are each encased in another serous membrane called the visceral peritoneum. These serous membranes ( the parietal and visceral peritoneum), together with the serous fluid lubricate, the organs so that they experience very little friction as they move against the body wall and each other. |
|
Why aren't the kidneys surrounded by a serous membrane? |
Unlike the abdominal organs which are housed within the peritoneal membranes, the kidneys are not allowed to move when the body moves. Instead, the kidneys are held firmly in place by a layer of adipose tissue called perirenal fat. Even thin people have perirenal fat. However, if a person gets really emaciated, he or she can loose perirenal fat, and the kidneys can slip as a result. While it is natural for many organs to move as your body moves, it can be devastating if it happens to the kidneys, because the dropping kidney's ureter might get pinched, blocking urine flow to the bladder. |
|

How big are the kidneys? Kidney anatomy parts? |
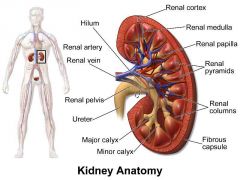
The kidneys are 11-14 cm in length and 6 cm wide. They are surrounded by a renal capsule, which is composed of fibrous connective tissue. The interior is split into 2 regions: the outer part called the renal cortex and the inner part called the renal medulla. The medulla is composed of roughly cone-shaped structures called renal pyramids. The base of these pyramids form the boundary between the medulla and cortex. The tips of the pyramids are called renal papillae, and they point towards funnel-shaped structures called minor calyces. Urine formed in the renal pyramids enters into these minor calyces. The minor calyces converge to form major calyces, and the major calyces converge to form the renal pelvis. The renal pelvis then narrows to form the ureter, which ultimately removes urine from the kidneys. The renal pyramids are separated by renal columns, which are essentially extensions of the cortex that project into the medulla. |
|
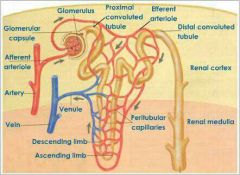
What is a nephron? |
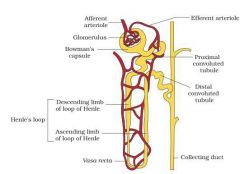
The functional unit of the kidney is the nephron. The nephron spans both the cortex and medulla. The blood enters the nephron at the renal corpuscle, which is in the cortex of the kidney. The nephron then extends into the medulla, leaves the medulla and goes back into the cortex, and then it enters the medulla once more. There, it dumps into the collecting duct, which leads to 1 of the minor calyces. |
|
What is the renal corpuscle? What is the percentage of nephron's that don't have a loop of Henle? |
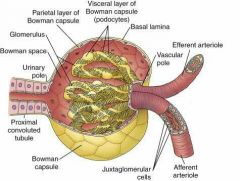
The renal corpuscle is, essentially, the beginning of the nephron. It consists of a capsule, called Bowman's corpuscle, and a network of capillaries called the glomerulus. The proximal tubule runs from the renal corpuscle to a long tube called the loop of Henle. The loop of Henle dips into the medulla and then comes back into the cortex. In the cortex, the loop of Henle meets up with the distal tubule, which leads to the collecting duct. It turns out that only about 10% of the nephron's actually have a loop of Henle. This means 90% of nephron's don't have one. |
|

How many nephrons are there in each kidney? |
There are about 1.3 million nephrons in each kidney. At the bare minimum, at least 1/3 of them must be functional. If fewer than 1/3 are functional, you simply can't survive. This should tell you something about the kidneys. They are obviously super-efficient! This is why you can donate a kidney. Even if 1 of your kidneys is removed, you still have roughly half of your nephrons. That's plenty to do the job. |
|
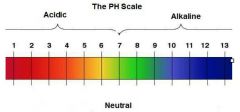
How do kidneys control the pH of the blood? |
The kidneys can adjust the amount of H+ ions in the blood, which determines the pH. The more H+ in the blood, the lower the pH. If the blood pH goes up, the blood needs more H+. Thus, the secretion of H+ into the nephron is reduced. This results in fewer H+ ions getting into the urine, and more H+ ions staying in the blood. This then lowers the pH of the blood, and it raises the pH of urine. At the same time, an increase in blood pH will reduce the HCO3- (bicarbonate ion) reabsorption which takes place in the nephron. The bicarbonate is a base. If less base is reabsorbed back into the blood, what would happen to the pH of the blood? It will go down. After all, more base means higher pH, so less base means lower pH. Once again, this will increase the pH of the urine, because if bicarbonate is not being reabsorbed into the blood, it is staying in the urine, and that raises the pH of urine. If the distal tubules sense a decrease in blood pH, exactly the opposite occurs. |
|
What is erythropoiesis? And how do the kidneys stimulate erythropoiesis? |
Erythropoiesis is the production of red blood cells. The kidneys stimulate erythropoiesis. Cells in the kidneys detect low oxygen, and in response, they produce erythropoietin, which signals the bone marrow to increase red blood cell production. |
|

How do the kidneys regulate blood pressure? |
Surprisingly enough, the kidneys play a role in blood pressure regulation. This is so because ultimately, the volume of blood determines the blood pressure. Since the kidneys determine the amount of water in the blood, they therefore affect the blood pressure. A drop in blood pressure or a decrease in blood sodium levels can be detected in the afferent arteriole by the juxtaglomerular cells. When these cells detect either of those changes, they respond by releasing renin. Renin is an enzyme, not a hormone. It activates an inactive protein of the blood that is made in the liver. This inactive protein is called angiotensinogen. It is a precursor and it is not the chemical that actually affects blood pressure; it is a chemical which leads to the chemical that affects blood pressure. |
|
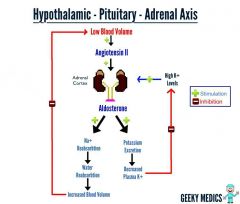
What happens when renin reacts with angiotensinogen? |
When renin interacts with angiotensinogen, it produces a peptide called angiotensin I. This peptide is not quite the 1 that affects blood pressure either, but it is close. When it circulates through the lungs, it encounters another enzyme called the angiotensin converting enzyme (ACE) which activates angiotensin, creating angiotensin II. This is the active substance, and it does 4 things. First, it increases vasoconstriction quiet powerfully. When vasoconstriction increases, blood pressure increases. Second, it makes a person thirsty. This is another way of increasing blood pressure, because more water makes a larger volume of blood, which leads to a higher blood pressure. Third, it increases salt appetite. After all, 1 of the things that the juxtaglomerular cells respond to is a decrease in sodium levels. Increasing the appetite for salt will hopefully alleviate the problem of low sodium. Finally, it causes the release of aldosterone, a hormone that increases sodium reabsorption in the kidneys. |
|
How do the third and fourth effects of angiotensin II help raise blood pressure? What is the hormone that produces opposite effect? |
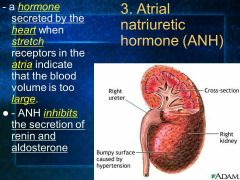
Believe it or not, the 3rd and 4th effects of angiotensin II also aid in raising blood pressure. Both of these effects will increase the amount of sodium in the blood. With more sodium, the blood will absorb more water, because the water will be attracted to the increased concentration of solute. If water absorption is increased, blood volume will go up, which will once again lead to a higher blood pressure.
There's 1 hormone that produces the opposite effect. The atrial natriuretic hormone comes from the atria of the heart. When blood volume is high, it actually stretches the 2 atria. This triggers the release of the atrial natriuretic hormone, which inhibits the nephron's from reabsorbing sodium. This lowers the amount of water reabsorbed, because water follows solutes and solutes follow water. Thus, if the amount of solute is reduced, the amount of water reabsorbed is reduced. This lowers blood volume, which lowers blood pressure.
|
|

What are the 4 steps of cleaning out the blood that takes place in the nephrons? |
The 1st step is filtration which occurs in the glomerulus and the Bowman's capsule which surrounds the glomerulus is where filtrate is collected. Filtration doesn't really remove anything bad. It just keeps blood cells and proteins in the blood vessel. Both good and bad chemicals in the filtrate flow through the filtration barrier and into the proximal tubule of nephron. Although the filtrate is in now in the functional unit of the kidney, it is not considered urine. In fact, upon entry into the proximal tubule, the fluid is essentially the same as interstitial fluid. The next 3 steps turn this fluid into urine. The 2nd step is reabsorption. As blood passes through the blood vessels which run along the nephron, the valuable chemicals that the blood needs are reabsorbed across the wall of the nephron. This reabsorption is controlled by a series of complex transport processes which ensure that useful chemicals are reabsorbed and that they are reabsorbed to their proper levels. Thus, even though sodium is a necessary component in blood plasma, if there is too much sodium in the nephron, it will not all get reabsorbed into the blood. Instead, the reabsorption will occur only until the sodium levels in the blood plasma have reached their proper level. The 3rd step is secretion. In this step, certain chemicals which have passed into the blood from the nephron must be removed removed from the blood. We don't want those chemicals in blood plasma, so they must be secreted back into the nephron. Harmful or excess chemicals which get back into the blood during step 2 get removed in step 3. Compared to the amount of reabsorption that takes place in the kidneys, the amount of secretion that goes on is quiet minimal. Nevertheless, secretion is important, because kidneys can adjust the blood pH by secreting H+ ions. The 4th step is water reabsorption. This is a separate step because its so complex. The processes which occur in the nephron regulate the water volume in the body. The water enters the nephron, and then the blood reabsorbs exactly the amount of water it needs and leaves the rest. The remaining water is the principal component of urine. |
|
When is filtrate considered urine? How much blood do the kidneys process? |
Filtrate is properly considered urine after it passes from the collecting duct into the calyx. The average adult has about 5 liters of blood, and that entire volume passes through the heart every minute. The blood flow to the kidneys is about 20% of that. Thus, about 1 liter of blood flows through the kidneys every minute. This is called renal blood flow rate. Thus, the nephrons in the kidneys are performing this 4-step process on about 1 liter of blood each minute. That's about 1,400 liters of blood every day. |
|
What are the 2 factors that fight against the glomerular capillary pressure (GCP) ? |
The 2 factors are capsular pressure and osmosis. The Bowman's corpuscle pushes back against the glomerulus. This results in capsular pressure, which fights the GCP. The parietal layer of the Bowman's corpuscle acts as duct tape, it exerts pressure against the blood flowing out of the glomerular capillaries. It exerxts about 10mmHg of pressure. The other factor is osmosis. The filtrate leaves the glomerular capillaries, but the proteins don't. Thus, the concentration of proteins is much higher inside the capillaries than outside. Proteins are too big to diffuse through the capillaries. Thus, osmosis takes over. The water in the filtrate is attracted back to the higher concentration of proteins. As a result, some of it crosses the filtration membrane and goes back into the capillaries. This, of course, fights GCP, which is pushing water out of capillaries. Pressure caused by this osmosis is called colloid osmotic pressure, and it measures about 28mmHg. |
|
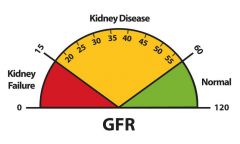
What is glomerular filtration rate (GFR)? How do kidneys filter so much fluid so fast? |
It is the rate at which filtration is produced in glomerular filtration (125 ml/minute). First reason is the filtration membrane is highly permeable. This allows filtrate to leave glomerular capillaries quickly. Second reason is the blood pressure in glomerular capillaries is higher than ordinary capillaries. Pressure in ordinary capillaries is on the order of 25mmHg and pressure in glomerular capillaries is about 45mmHg. This extra pressure helps push plasma through filtration membrane. Since pressure is higher than that of an ordinary capillary, filtrate flows out of glomerular capillaries more quickly than interstitial fluid flows out of ordinary capillaries. |
|

Why is the pressure in glomerular capillaries high? |
Its the result of an anatomical feature of arterioles that enter and leave the glomerulus. The afferent arteriole brings blood to Bowman's corpuscle and the efferent arteriole brings blood out of Bowman's corpuscle. This blood has a lot less plasma in it, since much of the plasma became filtrate while in glomerulus. This plasma-poor blood is sent in capillary networks down the length of the nephron, so that it can reabsorb useful chemicals from the nephron. The efferent arteriole is smaller than the afferent arteriole and this causes a backup of blood, increasing pressure behind it. Thus, blood in glomerulus is at higher pressure than blood in other parts of body because efferent arteriole is smaller than the afferent arteriole. |
|

Why is the GCP important? Where does reabsorption occur most? What is tubular maximum? |
Increased glomerular capillary pressure (GCP) allows glomerular filtration rate (GFR) to be high, because pressure is continually pushing filtrate out of glomeruluar capillaries. If the GCP goes down so will the GFR, if the GCP increases so will the GFR. Renal shutdown would happen if the GCP decreases too much because the GFR would drop to zero.
Most of the reabsorption occurs in the proximal tubule of nephron. For example, about 65% of water needed by blood is reabsorbed in proximal tubule, as virtually 100% of the glucose that the blood needs.
Tubular maximum is the maximum rate of reabsorption by active transport through the nephron tubules. Active transport requires ATP and a carrier, all nutrients and vitamins and minerals body needs is absorbed this way, substances such as glucose, amino acids, vitamins, and minerals such as sodium, potassium, calcium. The materials actively transported need a carrier and that takes energy. Water is reabsorbed by passive reabsorption. |
|
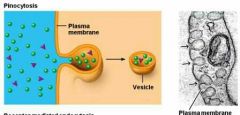
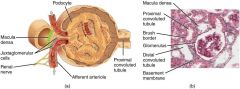
When is pinocytosis used in kidney? What are podocytes? |
Its used when some proteins leak through the filtration barrier and they must by reabsorbed, since proteins are too big for a carrier cells must take proteins back in by pinocytosis. Podocytes (or visceral epithelial cells) are cells in the Bowman's capsule in the kidneys that wrap around capillaries of the glomerulus. Podocytes cooperate with mesangial cells to support the structure and function of the glomerulus. Mesangial cells are found between the capillaries and help regulate the filtration process while providing support for the glomerular structure. They are also involved in the kidney's response to injury and disease. |
|
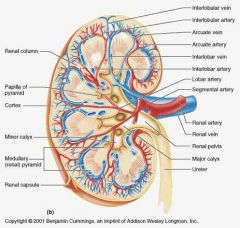
Name arteries in kidneys and where that are located. Where does osmosis occur in the nephron? |
Arcuate arteries are located at the border of the renal cortex and medulla. Interlobar arteries are in between renal pyramids and they branch over the base of the renal pyramids, little arteries and capillaries divide off the interlobar arteries and supply the pyramid and cortex with blood. Peritubular arteries are around nephron, they allow for reabsorption and secretion between the blood and the inner lumen of the nephron. In both the proximal convoluted tubule and the loop of Henle, osmosis of water occurs whereby the water moves from the more concentrated environment within the tubules to the less concentrated environment of the capillaries. This therefore creates a balanced concentration of water within and outside the tubules throughout the nephron network. |
|
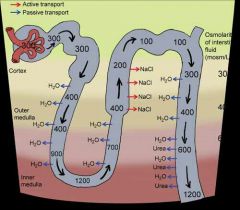
What happens in the parts of nephrons? |
1). Proximal convoluted tubule - reabsorb Na+ and K+(active transport), water(osmosis), organic solute reabsorb 100%.
2). Loop of Henle - reabsorption of water by osmosis, Na+ and K+(active transport) at the stage here there is no glucose and amino acids present(because it is reabsorb 100% at the Proximal convoluted tubule). The descending part is permeable to water and solutes but the ascending is not. When filtrate is in descending part, it has equal solute concentration to interstitial fluid but when filtrate enters the medulla, surrounding interstitial fluid increases in solute concentration which pulls water out of loop of Henle by osmosis and urea comes in loop of Henle by diffusion.
3). Distal convoluted tubule - reabsorption of water by osmosis, Na+ and K+(active transport). The ascending part of loop of Henle is not permeable to water or solutes. Thus, the only way anything can leave is active transport. The ascending portion is where only sodium, potassium, and chloride ions leave the nephron and go into the vasa recta. Solute concentration decreases due to electrolytes leaving. |
|
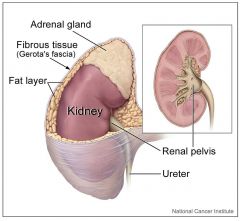
What are the 3 layers of the kidney? What are the 3 layers that surround the kidney? |
They are the cortex, medulla, and renal pelvis. The 3 parts surrounding the kidney are the renal fascia, perirenal fat, and the renal capsule. The renal fascia anchors the kidney to the peritoneum and this fibrous tissue surrounds both the kidney and adrenal gland. The renal capsule covers the kidney and is covered by perirenal fat. |
|
|
What part of tubule is permeable when adh is present? |
When adh is present the distal tubule is permeable and collecting tubule. |

