![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
nervous system review
|
|
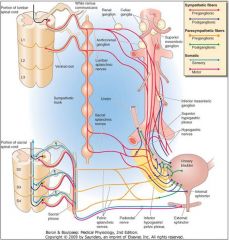
innervation to the urinary system
|
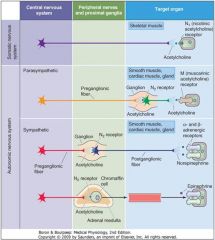
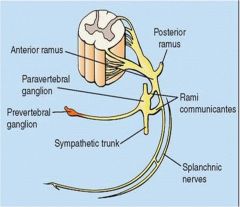
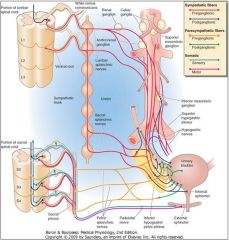
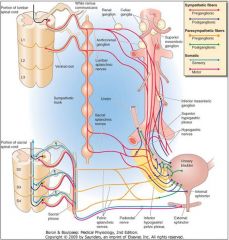
Axons of neurons in
the intermediolateral cell column pass through the ventral root through the ventral ramus into the mixed spinal nerve. They then pass through the white ramus communicans into a paravertebral sympathetic ganglion, where they do NOT synapse. They continue into the abdomino-pelvic splanchnic nerves to synapse in a prevertebral ganglion by means of a N2 (N G) synapse. Acetylcholine is the neurotransmitter for the first-order (primary) neuron, whereas norepi- nephrine is the neurotransmitter for the second-order (secondary) neuron. The only exception is the sympathetic supply to the sweat glands, where acetylcholine is the neurotransmitter for both neurons. |
|

loin and groin pain
|
characteristic of ureitic pain; ureteric stone produces colicky pain
|
|
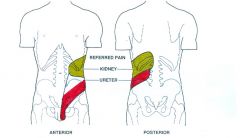
Referred renal pain
|
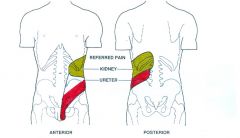
Primarily to the back and flank
|
|

|
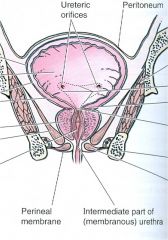
When empty, the urinary bladder Is located in the lesser pelvis,
posterior to the pubic symphysis. It rises higher when full. Its body has an apex, a superior surface, two inferolateral surfaces, and a base. The base is located posteriorly, and contains the trigone. |
|
|
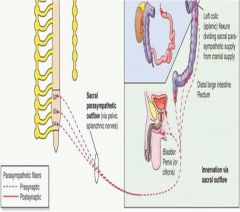
PNS -> pelvic plexus (synapse) -> supply destusor and sphincter muscles of bladder
sensory fibers follow this path backwards |
|
|
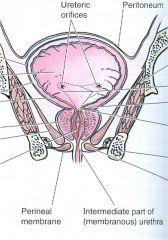
Coronal section through bladder;
Note bladder is infraperitoneal, note ureteric orifices, trigone located in fundus of bladder, note neck of bladder passes through prostate gland |
|
|
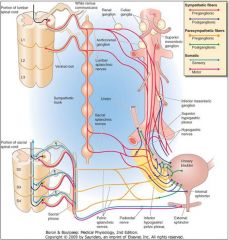
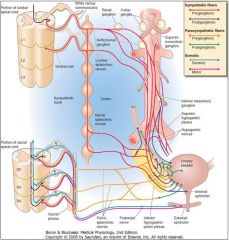
IML T10 to L2 -> ventral root -> ventral ramus -> white ramus communicans -> paravertebral ganglion (no synapse) -> lesser, least, lumbar splanchnic nerves -> aortic and hypogastric plexuses -> postganglionic fibers pass w vesical arteries to supply the bladder
|
|
|
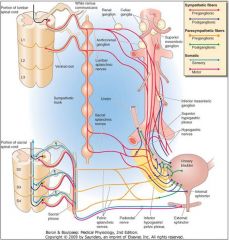
The first neuronal cell bodies lie within the sacral parasympathetic nucleus of the spinal cord at S2-S4. Axons pass out the
ventral rami to join the pelvic splanchnic nerves which feed the pelvic plexus. Synapse occurs on second-order neurons via a N2 nicotinic cholinergic receptor. Postganglionic neurons then send their processes through the plexus to innervate the bladder. Red = preganglionic sympathetics and somatic motor fibers. Purple = postganglionic sympathetic fibers. Orange = preganglionic parasympathetic fibers. Green = postganglionic sympathetic fibers. Blue = somatic sensory fibers. |
|
motor supply to the sphincter urethrae (external)
|
This
sphincter lies within the urogenital diaphragm. It is composed of striated muscle. Its motor supply arises from the nucleus of Onuf in the sacral spinal cord from S2-S4. The axons of these neurons pass via the ventral roots to the ventral rami to enter the pudendal nerve. They pass with the pudendal nerve to innervate the sphincter urethrae (external urethral sphincter). Note that this system is under voluntary control, unlike the sphincter vesicae (internal urethral sphincter). |
|
|
At the lower tip of the bladder trigone, the
bladder neck opens into the prostatic urethra (dark blue arrow). At this point the smooth muscle fibers are interspersed with elastic tissue to form the sphincter vesicae*, also termed the internal urethral sphincter or Involuntary urethral sphincter (red arrow). The parasympathetic fibers innervate the smooth muscle cells via M3 muscarinic cholinergic Receptors. Thus, drugs that inhibit muscarinic cholinergic receptors (such as tolterodine, trospium, darifenacin, and solifenacin) can be used to treat urinary incontinence due to bladder hyperactivity. |
|

Parasympathetic effects on bladder
|

stimulates detrusor smooth muscle contraction
postganglionic symps also reelase ATP which can stimulate purinergic receptors |
|

NO on bladder
|

Relaxes smooth msucle cells in bladder
note that the preganglionic para- sympathetics in the pelvic splanchnic nerves cause the detrusor muscle to contract, and the sphincter vesicae (dark blue arrow) to relax, promoting emptying of the bladder in a coordin- ated manner. |
|
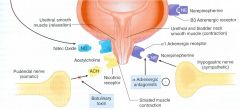
Sympatheic stimulus of bladder
|

Increased sphincter vesicae tone (NE) -> alpha 1 adrenergic receptors
NE can also relax detrusor muscle in the wall of bladdder by stimulating B3 adrenergic receptors |
|

|
peripheral innervation of the bladder
|
|
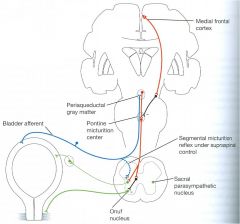
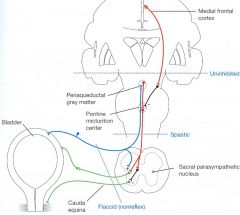
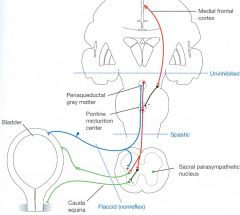
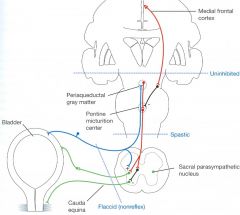
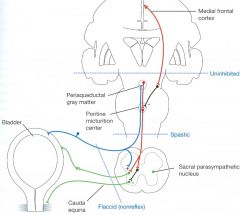
normal micturition reflex involves a supraspinal pathway
|
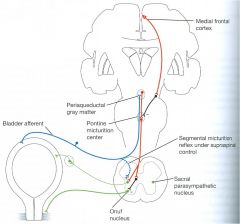
The reflex is
coordinated by the pontine micturition center. This region, activated by input from the bladder, contains neurons that stimulate sacral preganglionic parasympathetic neurons and inhibit a lateral pontine area that activates neurons In Onuf’s nucleus. Thus, activation of the pontine micturition center leads to coordinated contraction of the detrusor muscle of the bladder and relaxation of the external urethral sphincter muscle required for normal micturition. The excitability of the pontine micturitioncenter is controlled by inhibitory input from the medial frontal lobe, which is the basis for voluntary control of micturition. |
|
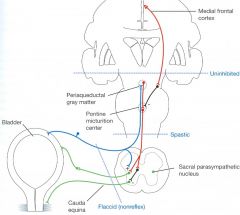
COMBINED AFFERENT AND EFFERENT LESIONS
|
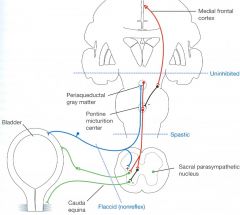
Severing both afferent and efferent
nerves initially causes the bladder to become distended and flaccid. In the chronic state of “decentralized bladder”, many small contractions of the progressively hypertrophied bladder muscles replace the coordinated events of micturition. Although small amounts of urine can be expelled, a residual volume of urine remains In the bladder after urination. |
|
afferent lesions
|
When only the sacral dorsal nerve roots containing the sensory
fibers are interrupted, reflex contractions of the bladder, in response to the stimulation of the stretch receptors are totally abolished. The bladder frequently becomes distended, the wall thins, and bladder tone decreases. However, some residual contractions remain because of the intrinsic contractile response of smooth muscle to stretch. As a rule, residual volume is present after urination. Incontinence is present, and urinary retention occurs. Perianal sensation, and the anal and bulbocavernous reflexes are abolished. Bladder volume is increased, but bladder pressure is decreased. The lesion is localized typically in the conus medullaris or cauda equina. |
|
Spinal cord lesions
|
The effects of spinal cord transection (e.g., in paraplegic patients)
include the initial state of spinal shock in which the bladder becomes overfilled and exhibits sporadic voiding (“overflow incontinence”). With time, the voiding reflex is re-established, but no voluntary control of urination is possible. Bladder volume is often reduced and reflex hyperactivity may lead to a state of spastic neurogenic bladder, in which the bladder fills to a set point, and then spontaneously empties whether it is convenient for the patient or not. Perianal sensation is preserved, and the anal and bulbo- cavernous reflexes are normal. Bladder intravesical pressure is increased but bladder volume is decreased. The bladder cannot empty completely, resulting in the presence of significant amounts of residual urine. Urinary tract infections (UTIs) are common, because the residual volume of urine in the bladder serves as an incubator for bacteria. In addition, during the period of overflow incontinence before the voiding reflex is re-established, these patients must be catheterized frequently, further predisposing them to urinary tract infections. The level of the lesion is between the lower brainstem or spinal cord above the level of the conus medullaris. |
|
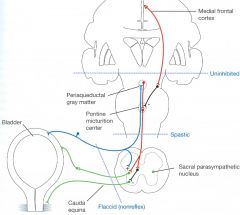
Uninhibited neurogenic bladder
|
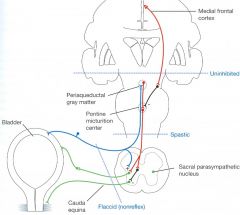
This condition is produced by a lesion between the medial frontal cortex and the pontine
micturition center. Incontinence occurs, but retention does not. Perianal sensation and the anal and bulbocavernous reflexes are preserved. Bladder volume and intravesical pressure are normal. The lesion is typically localized in the medial frontal lobes. CLINICAL EXAMPLES: HYDROCEPHALUS, MENINGIOMA, OTHER TUMORS OF THE BRAIN. |
|
|
bulbocaavernous reflex
|
tapping the dorsal portion of the penis causes the bulbocavernous portion to contract (measures integrity of S2,3 and 4)
|
|
|
Relative height of kidneys
|
Right kidney is lower than the left due to the large right lobe of the liver
|
|
|
Kidney location in abdomen
|
Retroperitoneal (posterior to the parietal peritoneum)
Thus they are retro-peritoneal in location, and are associated with the musculature of the posterior abdominal wall (psoas, quadratus lumborum). |
|
|
Where would a ruptured renal cyst drain to?
|
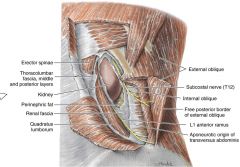
Due to the fascial capsule of Gerota (fascial sac which contains the kidney and perirenal fat) it would not cross the midline or mix with other contents of retroperitoneal space but pass with the ureter within the fascial capsule into the pelvis
|
|
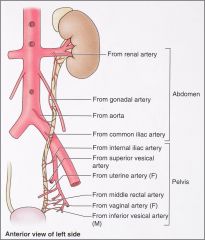
blood supply of kidney
|
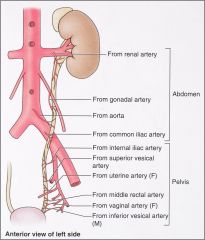
|
|
|
where does the gonal vein enter the IVC?
|
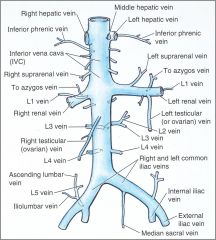
gonadal veins joins the left renal vein
|
|
|
Hallmark of renal pain
|
Pain elicited or increased by pressure on the costovertebral angle
|
|
|
Urter pain
|
T12 and L1; pain is felt in back, over lateral side of hip (loin) and L1 (groin); ureteric pain is colicky
|
|
|
Testicular pain
|
Can be a symptom of ureteric colic;
Paravertebral ganglia 0> least thoracic splanchnic nerve -> white ramus communicans of L1 |
|
|
Kidney pain dermatone
|
T8-L1, referred to back; T12 and L1 involve only when proximal ureter is involved (loin and groin)
|
|
|
Common sites of stones
|
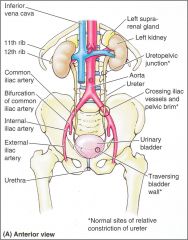
|
|
|
differential for upper lumbar pain
|
erector spinae contraction (herniation)
kidney pain (full blown dermatone) ureteric pain (more localized) |
|
|
supravenal vein
|
only one; receive blood from adrenal glands; the right goes straigh tinto the IVC while the left drains into the left renal vein
|
|
|
nutcracker renal pelvis
|
superior mesenteric artery compresses left renal vein
|
|
|
Where do the two ureters enter the bladder?
|
Trigone?
|
|
|
detrusor muscle
|
smooth muscle which surrounds the entire bladder
|
|
|
Parasympathetic innervation of the bladder
|
Terminate on ganglion cells located in wall of bladder -< short postganglionics innervate detrusor muscle
Also innervated bladder neck (posterior urethra) |
|
|
Sympathetic Innervation of Bladder
|
Sympathetic chain -> hypogastric nerves via L2
|
|
|
Voluntary innveration of bladder
|
Pudendal nerve to external bladder sphincter (S2-S3)
|

