![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
1.) What is a CVA? 2.) What are the two types? |
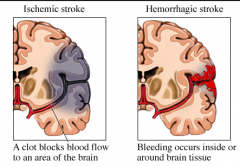
1.) Cerebrovascular Accident (Stroke): acute neurologic dysfunction of vascular origin, w/ symptom & signs corresponding to the focal area of the brain affected 2.) Ischemic (80%-result of embolism traveling to brian)) and Hemmorrhagic (20%- brain bleed) |
|
|
What causes a Ischemic CVA?
|
- Severe stenosis (typically from atherosclerosis) of crotid and basilar arteries or microstenosis of small deep arteries of the brain create blockage - Embolism travels and blocks vasculature in brain causing tissue death |
|
|
- What are risk factors for ischemic CVA?
|
- Hypertension, cardiac disease (a-fib, mitral stenosis, structural abnormalities), diabetes, cigarette smoking, alcohol, drugs, obesity
|
|
|
- What causes a hemorrhagic CVA? - How does the fatality rate compare to ischemic? |
- Cranial blood vessel breaks - > blood leaks into brain - Higher fatality rate with Hemorrhagic CVA |
|
|
- What are risk factors for Hemorrhagic CVA? |
- Same as ischemic but also genetic vascular malformations
|
|
|
How is a Transient Ischemic Attack (TIA or mini-stroke) different from a CVA
|
- Silimar symptoms to CVA but resolve within 24 hours. - TIA could bve a sign of impending CVA |
|
|
CVA Related Syndroms 1.) Cerebral Anoxia 2.) Ruptured Anyeurysm |
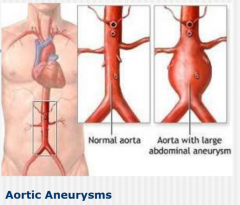
1.) Lack of oxygen to brain - can result in hemiplegia 2.) Enlargement of arterial wall related to atherosclerosis; bursting can result in death or hemiplegia |
|
|
- What characteristics of CVA symptoms
|
- Differ for every CVA - Symptoms depend on location - Can relate to any area: cognition, vision, movement, emotion, breathing, sensation, swallowing, speech, etc. |
|
|
- What are general symptoms of a CVA - How can you test for CVA (and area affected) |
- loss of consciousness, inability to speak, sudden/severe headache, voimiting, sudden numbness or weakness of face, arm, leg, especially on one side - Computerized Tomography (CT), Magnetic Resonance Imaging (MRI), Positon emission tomography (PET) scans |
|
|
What is part of the medical management of CVA (acute)
|
- Maintaining open airway, treating hypertension (medication), administer t-PA if appropriate, administer intravenous fluids, prevent deep vein thrombosis (DVT) (using blood thinners -which would stop pulmonary emboli, prevent respiratory problems
|
|
|
What is part of the medical management of CVA (long term)
|
- Blood thinners, filter placement if embolism/DVT occured (to catch clots), Botox injections is muscle spasticity/joint contractures
|
|
|
What is the main effect of CVA? - how does recovery normally occur - Overtime what occurs as a result? |
- Hemiplegia: paralysis/incoordination of entire contralateral side (to area of brain with CVA). - Recovery normally occures proximal to distal - Shoulder subluxation (joint separation) |
|
|
1.) Main concept of Brunnstrom Stages of Stroke Recovery 2.) What are the stages |
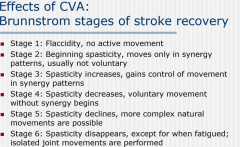
- After a stroke brain reverts to more primitive patterns of movement, you must progress through stages of abnormal movement in recovery. Also patients may stop recovery at any stage
|
|
|
Effects of CVA: What are motor synergies - WHat type are exhibited in UE and LE |
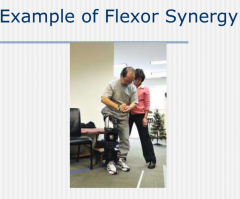
- Patterned movement characterized by co-contraction of flexors and extensors = UE: Flexor synergy, LE: Extensor synergy |
|
|
Effects of CVA: Why do muscle tone issues occur after CVA Define 1.) Hypotonus 2)Hypertonus |
- UWM dysfunction/brain cell death 1.) Lack of muscle tone (flaccidity) 2.) Abundance of tone (spasticity) |
|
|
Effects of CVA: What is muscle spasticity? - What can excite it? - What is "Clasp-Knife" phenomenon |
- Hyperactivity of muscle spindles stretch reflex (hyperactive firing) - Examiner's rapid passive stretch - Quick passive stretch casues resistance and then release |
|
|
Effects of CVA: What are some motor effects of CVA
|
- QUadriparesis (bilateral asymmetric weakness), clumsiness (hypotonia of ipsilateral limbs), weakness of upper/lower extremities, agraphia (inability to write)
|
|
|
Effects of CVA: Why might one loose sexual ability after a CVA?
|
- emotional problems, loss of sensation, loss of voluntary muscle control, imbalance of hormones, difficulty with cognition and communication, side effects of medications
|
|
|
- Effects of CVA: What is Dysphagia/why does it occur - Describe dysphagia diets/ what is OTs role? |
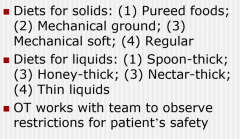
- swallowing dysfunction/poor movement and coordination in muscles of the throat
|
|
|
Effects of CVA: What are some cognitive deficits associated with CVA (7)
|
- Unilateral neglect (usually left), memory/attention deficits, problems w/ executive function, Alexia (inability to read), agnosia (inability to recognize), apraxia (deficits in motor planning), impaired behavior (impusivity)
|
|
|
Effects of CVA: What are some sensory deficits
|
- Numbness, contralateral hemi-sensory loss, difficulty w/ motor initiation due to sensory loss
|
|
|
Effects of CVA: What are some visual-perceptual deficits:
|
- Visual field impairment, poor contralateral conjugate gaze, field dependency, left/right unilateral visual neglect, visuospatial impairment, hemianopsia, visual agnosia (can't recognize objects)
|
|
|
Effects of CVA: What is the most common Psychological/Behavioral effect? - What are other effects? |
- Depression (35%) - Lability (rapid changing emotions), apathy (lack of initative), behavior abnormailities, agitation/restlessness |

