![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
170 Cards in this Set
- Front
- Back
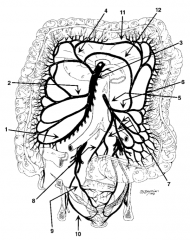
What is structure 1? |
Ileocolic artery (1) |
|
What is structure 2? |
Right colic artery (2) |
|
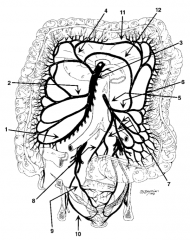
What is structure 3? |
Superior Mesenteric Artery (3) |
|
What is structure 4? |
Middle colic artery (4) |
|
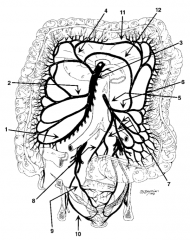
What is structure 5? |
Inferior Mesenteric Artery (IMA) (5) |
|
What is structure 6? |
Left Colic Artery (6) |
|
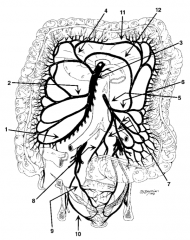
What is structure 7? |

Sigmoidal Artery (7) |
|
What is structure 8? |
Superior Hemorrhoidal Artery / Superior Rectal (8) |
|
What is structure 9? |
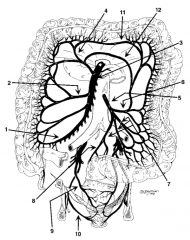
Middle Hemorrhoidal Artery (9) |
|
What is structure 10? |
Inferior Hemorrhoidal Artery (10) |
|
What is structure 11? |
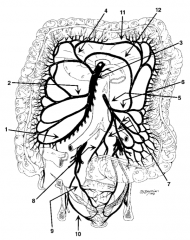
Marginal artery of Drummond (11) |
|
What is structure 12? |
Meandering artery of Gonzalez |
|
|
What are the white lines of Toldt? |
Lateral peritoneal reflections of the ascending and descending colon |
|
|
What parts of the GI tract do not have a serosa? |
- Esophagus - Middle and distal rectum |
|
|
What are the major anatomic differences between the colon and small intestine? |
- Colon has taeniae coli, haustra, and appendices epiploicae (fat appendages) - Small intestine is smooth |
|
|
What is the blood supply to the proximal rectum? |
Superior hemorrhoidal (or superior rectal) from the IMA |
|
|
What is the blood supply to the middle rectum? |
Middle hemorrhoidal (or middle rectal) from the hypogastric (internal iliac) |
|
|
What is the blood supply to the distal rectum? |
Inferior hemorrhoidal (or inferior rectal) from the pudendal artery (a branch of the hypogastric artery) |
|
|
What is the venous drainage of the proximal rectum? |
Via the IMV to the splenic vein, then to the portal vein |
|
|
What is the venous drainage of the middle rectum? |
Via the iliac vein to the IVC |
|
|
What is the venous drainage of the distal rectum? |
Via the iliac vein to the IVC |
|
|
What is colorectal carcinoma? |
Adenocarcinoma of the colon or rectum |
|
|
What is the incidence of colorectal carcinoma? |
- Most common GI cancer - Second most common cancer in the US - Incidence increases with age starting at 40 and peaks at 70-80 years |
|
|
How common is colorectal carcinoma as a cause of cancer deaths? |
Second most common cause of cancer deaths |
|
|
What is the lifetime risk of colorectal cancer? |
6% |
|
|
What is the male to female ratio for colorectal carcinoma? |
~1:1 |
|
|
What are the risk factors for colorectal carcinoma? |
- Dietary: low-fiber, high-fat diets correlate with increased rates - Genetic: family history is important; FAP, Lynch's syndrome - IBD: ulcerative colitis > Crohn's disease, age, previous colon cancer |
|
|
What is Lynch's syndrome? |
HNPCC = Hereditary NonPolyposis Colon Cancer - Autosomal dominant inheritance of high risk for development of colon cancer |
|
|
What are current ACS recommendations for polyp / colorectal screening in asymptomatic patients without family (first-degree) history of colorectal cancer? |
Starting at age 50, at least one of the following test regimens is recommended: - Colonoscopy q10 years - Double contrast barium enema (DCBE) q5 years - Flex sigmoidoscopy q5 years - CT colonography q5 years |
|
|
What are the current recommendations for colorectal carcinoma screening if there is a history of colorectal carcinoma in a first-degree relative <60 years old? |
Colonoscopy at age 40 or 10 years before the age at diagnosis of the youngest first-degree relative, and every 5 years thereafter |
|
|
What percentage of adults will have a guaiac positive stool test? |
~2% |
|
|
What percentage of patients with a guaiac positive stool test will have colon cancer? |
~10% |
|
|
What signs / symptoms are associated with RIGHT-sided colorectal carcinoma? |
- Right side of bowel has a large luminal diameter, so tumor may attain a large side before causing problems - Microcytic anemia - Occult / melena more than hematochezia PR - Post-prandial discomfort - Fatigue |
|
|
What signs / symptoms are associated with LEFT-sided colorectal carcinoma? |
- Left side of bowel has smaller lumen and semisolid contents - Changes in bowel habits (small-caliber stools) - Colicky pain - Signs of obstruction - Abdominal mass - Heme (+) or gross red blood - Nausea, vomiting - Constipation |
|
|
From which site is melena from colon cancer more common? |
Right-sided colon cancer? |
|
|
From which site is hematochezia from colon cancer more common? |
Left-sided colon cancer |
|
|
What is the incidence of rectal cancer? |
Comprises 20-30% of all colorectal cancer |
|
|
What are the signs/symptoms of rectal cancer? |
Most common symptom is hematochezia (passage of red blood +/- stool) or mucus; also tenesmus, feeling of incomplete evacuation of stool (because of the mass), and rectal mass |
|
|
What is the differential diagnosis of a colon tumor / mass? |
- Adenocarcinoma - Carcinoid tumor - Lipoma - Liposarcoma - Leiomyoma - Leiomyosarcoma - Lymphoma - Diverticular disease - Ulcerative colitis - Crohn's disease - Polyps |
|
|
Which diagnostic tests are helpful for colon cancer? |
- H&P (note ~10% of cancers are palpable on rectal exam) - Heme occult - CBC - Barium enema - Colonoscopy |
|
|
What disease does microcytic anemia signify until proven otherwise in a man or post-menopausal woman? |
Colon cancer |
|
|
What tests help find metastases from colon cancer? |
- CXR (lung metastases) - LFTs (liver metastases) - Abdominal CT (liver metastases) - Other tests based on H&P (eg, head CT for left arm weakness looking for brain metastasis) |
|
|
What is the pre-op workup for colorectal cancer? |
- History - Physical exam - LFTs - CEA - CBC - Chemistry - PT / PTT - Type and cross, 2 U PRBC - CXR - U/A - Abdominopelvic CT |
|
|
What are the means by which colon cancer spreads? |
- Direct extension: circumferentially and then through bowel wall to later invade other abdominoperineal organs - Hematogenous: portal circulation to liver; lumbar/vertebral veins to lungs - Lymphagenous: regional lymph nodes - Transperitoneal - Intraluminal |
|
|
Is CEA useful in colon cancer? |
Not for screening but for baseline and recurrence surveillance (but offers no proven survival benefit) |
|
|
What unique diagnostic test is helpful in patients with rectal cancer? |
Endorectal U/S (probe is placed transanally and depth of invasion and nodes are evaluated) |
|
|
How are colorectal tumors staged? |
TMN staging system |
|
|
What are the characteristics of a Stage I colorectal tumor? |
Invades submucosa or muscularis propria (T1-2 N0 M0) |
|
|
What are the characteristics of a Stage II colorectal tumor? |
Invades through muscularis propria or surrounding structures but with negative nodes (T3-4, N0, M0) |
|
|
What are the characteristics of a Stage III colorectal tumor? |
Positive nodes, no distant metastasis (any T, N1-3, M0) |
|
|
What are the characteristics of a Stage IV colorectal tumor? |
Positive distant metastasis (any T, any N, M1) |
|
|
What is the approximate 5-year survival of colorectal cancer that is stage I? |
90% |
|
|
What is the approximate 5-year survival of colorectal cancer that is stage II? |
70% |
|
|
What is the approximate 5-year survival of colorectal cancer that is stage III? |
50% |
|
|
What is the approximate 5-year survival of colorectal cancer that is stage IV? |
10% |
|
|
What percentage of patients with colorectal cancer have liver metastases on diagnosis? |
~20% |
|
|
What is a "bowel prep"? |
Pre-operative prep for colon/rectal resection: 1. Golytely colonic lavage or Fleets Phospho-Soda until clear effluent per rectum 2. PO antibiotics (1 gm neomycin and 1 gm erythromycin x 3 doses)
Note: pt should also receive pre-op and 24-hr IV antibiotics |
|
|
What are the common pre-op IV antibiotics prior to colon/rectal resection? |
- Cefoxitin - Unasyn |
|
|
If the patient requiring colon/rectal surgery is allergic to penicillins (hives, swelling), what antibiotics should be prescribed |
IV Cipro and Flagyl |
|
|
What are the treatment options for colorectal cancer? |
Resection: wide surgical resection of lesion and its regional lymphatic drainage |
|
|
What decides low anterior resection (LAR) vs abdominal perineal resection (APR)? |
Distance from the anal verge, pelvis size |
|
|
What do all rectal cancer operations include? |
Total mesorectal excision - remove the rectal mesentery, including the lymph nodes (LNs) |
|
|
What is the lowest low anterior resection (LAR) possible? |
Coloanal anastomosis (anastomosis normal colon directly to anus) |
|
|
What do some surgeons do with any anastomosis less than 5 cm from the anus? |
Temporary ileostomy to "protect" the anastomosis |
|
|
What surgical margins are needed for colon cancer? |
Traditionally >5 cm; margins must be at least 2 cm |
|
|
What is the minimal surgical margin for rectal cancer? |
2 cm |
|
|
How many lymph nodes should be resected with a colon cancer mass? Why? |
12 LNs minimum = for staging, and may improve prognosis |
|
|
What is the adjuvant treatment of stage III colon cancer? |
5-FU and leucovorin (or levamisole) chemotherapy (if there is nodal metastasis post-op) |
|
|
What is the adjuvant treatment for T3-T4 rectal cancer? |
Pre-op radiation therapy and 5-FU chemo as a "radiosensitizer" |
|
|
What is the most common site of distant (hematogenous) metastasis from colorectal cancer? |
Liver |
|
|
What is the treatment of liver metastases from colorectal cancer? |
Resect with ≥1 cm margins and administer chemotherapy if feasible? |
|
|
What is the surveillance regimen for colorectal cancer? |
- Physical exam - Stool guaiac - CBC - CEA - LFTs (every 3 months for 3 years, then every 6 months for 2 years) - CXR every 6 months for 2 years and then yearly - Colonoscopy at years 1 and 3 post-op - CT scans directed by exam |
|
|
Why is follow-up so important for colorectal cancer in the first 3 years post-op? |
~90% of colorectal recurrences are within 3 years of surgery |
|
|
What are the most common causes of colonic obstruction in the adult population? |
- Colon cancer - Diverticular disease - Colonic volvulus |
|
|
What is the 5-year survival rate after liver resection with clean margins for colon cancer liver metastasis? |
~33% (28-50%) |
|
|
What is the 5-year survival rate ofter diagnosis of unresectable colon cancer liver metastasis? |
0% |
|
|
What are colonic and rectal polyps? |
Tissue growth into bowel lumen, usually consisting of mucosa, submucosa, or both |
|
|
How are colonic and rectal polyps anatomically classified? |
- Sessile (flat) - Pedunculated (on a stalk) |
|
|
What are the characteristics of "inflammatory (pseudopolyp)" colonic and rectal polyps? |
As in Crohn's disease or ulcerative colitis |
|
|
What are the characteristics of "hamartomatous" colonic and rectal polyps? |
Normal tissue in abnormal configuration |
|
|
What are the characteristics of "hyperplastic" colonic and rectal polyps? |
Benign - normal cells - no malignant potential |
|
|
What are the characteristics of "neoplastic" colonic and rectal polyps? |
Proliferation of undifferentiated cells; pre-malignant or malignant cells |
|
|
What are the subtypes of neoplastic polyps? |
- Tubular adenomas (usually pedunculated) - Tubulovillous adenomas - Villous adenomas (usually sessile and look like broccoli heads) |
|
|
What determines malignant potential of an adenomatous polyp? |
- Size - Histologic type - Atypia of cells |
|
|
What is the most common type of adenomatous polyps? |
Tubular 85% |
|
|
What is the correlation between size and malignancy of polyps? |
Polyps larger than 2 cm have a high risk of carcinoma (33%-55%) |
|
|
Which histologic types of adenomatous polyps have greater cancer potential? |
Villous > Tubovillous > Tubular
Think: VILLous = VILLain |
|
|
What is the approximate percentage of carcinomas found in the a tubular adenoma polyp? |
5% |
|
|
What is the approximate percentage of carcinomas found in the a tubulovillous adenoma polyp? |
20% |
|
|
What is the approximate percentage of carcinomas found in the a villous adenoma polyp? |
40% |
|
|
Where are most polyps found? |
Rectosigmoid (30%) |
|
|
What are the signs / symptoms of polyps? |
- Bleeding (red or dark blood) - Change in bowel habits - Mucus per rectum - Electrolyte loss - Totally asymptomatic |
|
|
What are the diagnostic tests for polyps? |
- Best = colonoscopy - Less sensitive for small polyps = barium enema and sigmoidoscopy |
|
|
What is the treatment for polyps? |
- Endoscopic resection (snared) if polyps - Large sessile villous adenomas should be removed with bowel resection and lymph node resection |
|
|
What is another name for familial polyposis? |
Familial Adenomatous Polyposis (FAP) |
|
|
What are the characteristics of Familial Adenomatous Polyposis (FAP)? |
- Hundreds of adenomatous polyps within the rectum and colon that begin developing at puberty - All undiagnosed, untreated patients develop cancer by ages 40-50 |
|
|
What is the inheritance pattern of Familial Adenomatous Polyposis (FAP)? |
Autosomal dominant (ie, 50% of offspring) |
|
|
What is the genetic defect associated with Familial Adenomatous Polyposis (FAP)? |
APC (Adenomatous Polyposis Coli) gene |
|
|
What is the treatment of Familial Adenomatous Polyposis (FAP)? |
- Total proctocolectomy and ileostomy - Total colectomy and rectal mucosal removal (mucosal proctectomy) and ileoanal anastomosis) |
|
|
What are the characteristics of Gardner's Syndrome? |
Neoplastic polyps of the small bowel and colon; cancer by age 40 in 100% of undiagnosed patients, as in FAP |
|
|
What are the other associated findings with Gardner's Syndrome? |
- Desmoid tumors (in abdominal wall or cavity) - Osteomas of skull (seen on x-ray) - Sebaceous cysts - Adrenal and thyroid tumors - Retroperitoneal fibrosis - Duodenal and periampullary tumors |
|
|
How can the findings associated with Gardner's Syndrome be remembered? |
Think of a gardener planting "SOD" - Sebaceous cysts - Osteomas - Desmoid tumors |
|
|
What is a desmoid tumor? |
- Tumor of the musculoaponeurotic sheath, usually of the abdominal wall - Benign, but grows locally - Treated by wide resection |
|
|
What medications may slow the growth of a desmoid tumor? |
- Tamoxifen - Sulindac - Steroids |
|
|
What is the inheritance pattern for Gardner's Syndrome? |
Varying degrees of penetrance form an autosomal-dominant gene |
|
|
What is the treatment of colon polyps in patients with Gardner's Syndrome? |
- Total proctocolectomy and ileostomy - Total colectomy and rectal mucosal removal (mucosal proctectomy) and ileoanal anastomosis |
|
|
What are the characteristics of Peutz-Jeghers' Syndrome? |
Hamartomas throughout the GI tract (jejunum / ileum > colon > stomach) |
|
|
What is the associated cancer risk from polyps in patients with Peutz-Jeghers' Syndrome? |
Increased |
|
|
What is the associated cancer risk for women with Peutz-Jeghers' Syndrome? |
Ovarian cancer (granulosa cell tumor is most common) |
|
|
What is the inheritance pattern of Peutz-Jeghers' Syndrome? |
Autosomal dominant |
|
|
What are the other signs of Peutz-Jeghers' Syndrome? |
- Melanotic pigmentation (black/brown) of buccal mucosa (mouth), lips, digits, palms, feet (soles)
- Think: Peutz = Pigmented |
|
|
What is the treatment of Peutz-Jeghers' Syndrome? |
Removal of polyps if symptomatic (bleeding, intussusception, or obstruction) or large (>1.5 cm) |
|
|
What are juvenile polyps in Peutz-Jeghers' Syndrome? |
Benign hamartomas in the small bowel and colon; not pre-malignant; also known as "retention polyps" |
|
|
What is Cronkhite-Canada syndrome? |
- Diffuse GI hamartoma polyps (ie, no cancer potential) associated with malabsorption / weight loss, diarrhea, and loss of electrolytes / protein
- Signs include alopecia, nail atrophy, and skin pigmentation |
|
|
What is Turcot's syndrome? |
Colon polyps with malignant CNS tumors (glioblastoma multiforme) |
|
|
What is diverticulosis? |
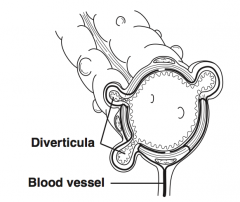
Condition in which diverticula can be found within the colon, especially the sigmoid; diverticula are actually false diverticula in that only mucosa and submucosa herniate through the bowel musculature
True diverticula involve all layers of the bowel wall and are rare in the colon |
|
|
What is the pathophysiology responsible for diverticulosis? |
Weakness in the bowel wall develops at points where nutrient blood vessels enter between antimesenteric and mesenteric taenia; increased intraluminal pressures then cause herniation through these areas |
|
|
What is the incidence of diverticulosis? |
~50-60% in US by age 60, with only 10-20% becoming symptomatic |
|
|
What is the most common site of diverticulosis? |
95% of people have sigmoid colon involvement |
|
|
Who is at risk for diverticulosis? |
People with low-fiber diets, chronic constipation, and a positive family history; incidence increases with age |
|
|
What are the symptoms / complications of diverticulosis? |
- Bleeding: may be massive - Diverticulitis - Asymptomatic (80% of cases) |
|
|
What is the approach to bleeding in patients with suspected diverticulosis? |
Without signs of inflammation: colonoscopy |
|
|
What is the approach to pain and signs of inflammation in patients with suspected diverticulosis? |
Abdominal / pelvic CT scan |
|
|
What is the treatment of diverticulosis? |
High-fiber diet is recommended |
|
|
What are the indications for operation with diverticulosis? |
- Complications of diverticulitis (eg, fistula, obstruction, stricture) - Recurrent episodes - Hemorrhage - Suspected carcinoma - Prolonged symptoms - Abscess not drainable by percutaneous approach |
|
|
When is it safe to get a colonoscopy or barium enema / sigmoidoscopy? |
Due to risk of perforation, this is performed 6 weeks after inflammation resolves to rule out colon cancer |
|
|
What is diverticulitis? |
Infection or perforation of a diverticulum |
|
|
What is the pathophysiology of diverticulitis? |
Obstruction of diverticulum by a fecalith leading to inflammation and microperforation |
|
|
What are the signs / symptoms of diverticulitis? |
- LLQ pain (cramping or steady) - Change in bowel habits (diarrhea) - Fevers - Chills - Anorexia - LLQ mass - Nausea / vomiting - Dysuria |
|
|
What are the associated lab findings with diverticulitis? |
Increased WBCs |
|
|
What are the associated radiographic findings of diverticulitis? |
- On x-ray: ileus, partially obstructed colon, air-fluid levels, free air if perforated - On abdominal / pelvic CT scan: swollen edematous bowel wall, particularly helpful in diagnosing an abscess |
|
|
What are the associated barium enema findings of diverticulitis? |
Barium enema should be avoided in acute cases |
|
|
Is colonoscopy safe in an acute setting of diverticulitis? |
No, there is an increased risk of perforation |
|
|
What are the possible complications of diverticulitis? |
- Abscess - Diffuse peritonitis - Fistula - Obstruction - Perforation - Stricture |
|
|
What is the most common fistula with diverticulitis? |
Colovesical fistula (to bladder) |
|
|
What is the best test for diverticulitis? |
CT scan |
|
|
What is the initial therapy for diverticulitis? |
- IV fluids - NPO - Broad-spectrum antibiotics with anaerobic coverage - NG suction (as needed for emesis / ileus) |
|
|
When is surgery warranted for diverticulitis? |
- Obstruction - Fistula - Free perforation - Abscess not amenable to percutaneous drainage - Sepsis - Deterioration with initial conservative treatment |
|
|
What is the lifetime risk of recurrence of diverticulitis after the first episode? |
33% |
|
|
What is the lifetime risk of recurrence of diverticulitis after the second episode? |
50% |
|
|
What are the indications for elective resection for patients with diverticulitis? |
Two episodes of diverticulitis; should be considered after the first episode in a young, diabetic, or immunosuppressed patient |
|
|
What surgery is usually performed electively for recurrent bouts of diverticulitis? |
One-stage operation: resection of involved segment and primary anastomosis (with pre-op bowel prep) |
|
|
What type of surgery is usually performed for an acute case of diverticulitis with a complication (eg, perforation or obstruction)? |
Hartmann's procedure: - Resection of involved segment with an end colostomy and stapled rectal stump (will need subsequent re-anastomosis of colon usually after 2-3 post-op months) |
|
|
What is the treatment of diverticular abscess? |
Percutaneous drainage; if abscess is not amenable to percutaneous drainage, then surgical approach for drainage is necessary |
|
|
How common is massive lower GI bleeding with diverticulitis? |
Very rare! Massive lower GI bleeding is seen with diverticulosis not diverticulitis |
|
|
What are the most common causes of massive lower GI bleeding in adults? |
Diverticulosis (especially right sided), vascular ectasia |
|
|
What must you rule out in any patient with diverticulitis / diverticulosis? |
Colon cancer |
|
|
What is colonic volvulus? |
Twisting of colon on itself about its mesentery, resulting in obstruction and, if complete, vascular compromise with potential necrosis, perforation, or both |
|
|
What is the most common type of colonic volvulus? |
Sigmoid volvulus (makes sense because the sigmoid is a redundant / "floppy" structure!) |
|
|
What is sigmoid volvulus? |

Volvulus or "twist" in the sigmoid colon |
|
|
What is the incidence of sigmoid volvulus? |
~75% of colonic volvulus cases (think: Sigmoid = Superior) |
|
|
What are the etiologic factors for sigmoid volvulus? |
- High-residue diet resulting in bulky stools and tortuous, elongated colon - Chronic constipation - Laxative abuse - Pregnancy - Seen most commonly in bedridden elderly or institutionalized patients, many of whom have prior abdominal surgery or distal colonic obstruction |
|
|
What are the signs / symptoms of sigmoid volvulus? |
- Acute abdominal pain - Progressive abdominal distention - Anorexia - Constipation - Cramps - Nausea / vomiting |
|
|
What findings are evident on abdominal plain film? |
Distended loop of sigmoid colon, often in the classic "bent inner tube" or "omega" sign with the loop aiming toward the RUQ |
|
|
What are the signs of necrotic bowel in colonic volvulus? |
Free air, pneumostasis (air in bowel wall) |
|
|
How is the diagnosis of sigmoid volvulus made? |
Sigmoidoscopy or radiographic exam with gastrografin enema |
|
|
Under what conditions is gastrografin enema useful for sigmoid volvulus? |
If sigmoidoscopy and plain films fail to confirm the diagnosis; "birds beak" is pathognomonic seen on enema contrast study as the contrast comes to a sharp end |
|
|
What are the signs of strangulation of sigmoid volvulus? |
- Discolored or hemorrhagic mucosa on sigmoidoscopy - Bloody fluid in the rectum - Frank ulceration or necrosis at the point of the twist - Peritoneal signs - Fever - Hypotension - Increased WBCs |
|
|
What is the initial treatment of sigmoid volvulus? |
Non-operative: - If there is no strangulation, sigmoidoscopic reduction is successful in ~85% of cases - Enema study will occasionally reduce (5%) |
|
|
What is the percentage of recurrence after non-operative reduction of a sigmoid volvulus? |
~40% |
|
|
What are the indications for surgery with sigmoid vovlulus? |
- Emergently if strangulation is suspected or non-operative reduction unsuccessful (Hartmann's procedure) - Most patients should undergo resection during same hospitalization of redundant sigmoid after successful non-operative reduction because of high recurrence rate (40%) |
|
|
What is cecal volvulus? |
Twisting of the cecum upon itself and the mesentery |
|
|
What is a cecal "bascule" volvulus? |
Instead of the more common axial twist, the cecum folds upward (lies on the ascending colon) |
|
|
What is the incidence of cecal volvulus? |
~25% of colonic volvulus (ie, much less common than sigmoid volvulus) |
|
|
What is the etiology of cecal volvulus? |
- Idiopathic - Poor fixation of the right colon - Many patients have history of abdominal surgery |
|
|
What are the signs/symptoms of cecal volvulus? |
- Acute onset of abdominal or colicky pain beginning in the RLQ and progressing to a constant pain - Vomiting - Constipation - Abdominal distention - SBO - Many patients will have had previous similar episodes |
|
|
How is the diagnosis of cecal volvulus made? |
- Abdominal plain film - Dilated, ovoid colon with large air / fluid level in the RLQ often forming the classic "coffee bean" sign with the apex aiming toward the epigastrium or LUQ (must rule out gastric dilation with NG aspiration) |
|
|
What diagnostic studies should be performed to diagnose cecal volvulus? |
Water soluble contrast study (gastrografin), if diagnosis cannot bem ade by AXR |
|
|
What is the treatment for cecal volvulus? |
- Emergent surgery - Right colectomy with primary anastomosis or ileostomy and mucus fistula (primary anastomosis may be performed in stable patients) |
|
|
What are the major differences in the EMERGENT management of cecal volvulus vs sigmoid? |
Patients with cecal volvulus require surgical reduction, whereas the vast majority of patients with sigmoid volvulus undergo initial endoscopic reduction of the twist |

