![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back

What are risk factors for urolithiasis in sheep and goats? |
High levels of concentrates- unbalanced ration with high phosphorus, high magnesium. Water deprivation. Bore water. Males. Show animals. Castrates. Pet small ruminants. |
|
|
What is the most common type of urolithiasis in sheep and goats? |
Struvite. Magnesium ammonium phosphate hexahydrate. |
|
|
Where are the pain sites that uroliths lodge in the male sheep/goat? |
In urethra Proximal to the sigmoid flexure. Vermiform appendage. |
|

Clinical signs of urolithiasis in sheep? |
1) Away from the group. 2) Frequent tail swishing and foot stomping. 3) Wide stance with pelvic limbs held back. 4) Frequent straining with bruxism and bleating. 5) MM congested, H.R. , Resp elevate. 6) Anuria or drops of blood tinged urine. 7) Dry preputial hairs with calculi. 8) Can palpate the gritty calculus in the vermiform appendage. |
|
|
Sequalae of urolithiasis in sheep? |
1) Uroperitoneum- rupture rare, bladder wall becomes permeable. 2) Hydronephrosis due to back pressure. 3) Rupture of the urethra and penis |
|

What are signs of urethral/penile rupture due to urolithiasis? |
If untreated in 48 hours. Get subcutaneous swelling from scrotum to prepuce. Very oedematous. Large well demarcated purple discolored skin along ventrum overlying the accumulating urine. Discoloured skin and muscle becomes cold and sloughs after 10-14 days. |
|
|
Ddx for urolithiasis in sheep? |
Abomasal/small intestinal volvulus- more marked toxaemia, marked abdominal distension and rapid deterioation.
Coccidiosis and intussuception- tensemus and abdominal pain. Pleurisy and peritonitis in rams. |
|
|
What laboratory parameters can we use to help diagnose urolithiasis? |
Urea will be 30-60 mmol/l normally 2.2-6.6 Creatinine >500 umol/l normally 40-150 Ultrasound. |
|
|
How can we treat urolithiasis? |
Cut verminform appendage. Perineal urethrostomy- make mini vagina Perineal penectomy- making a bum willy Salvage surgeries |
|
|
Can an animal breed after a perineal urethrostomy/penectomy is done? What procedure can be done on a breeding animal? |
No. Tube cystotomy. |
|
|
How do we perform a perineal urethrostomy? |
Restrain animal in a crush. Tie tail up. Place a bag in anus or glove. Clip and surgical prep site. Epidural/block Make a longitudinal incision along ventral aspect of urethra. Suture to the skin. |
|
|
Management and control measures for urolithiasis in cattle and sheep? |
Fresh clean water at all times. Provide roughage. Urine acidifiers such as ammonium chloride. Sodium chloride to increase water intake. |
|

What is the common agent involved in pyelonephritis in cattle? Which cows is it mainly seen? |
Actinomyces renale/cornyebacterium renale or e-coli. 2-3 months post calving in beef cows. |
|
|
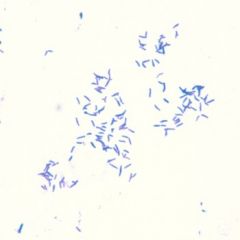
Characteristics of cornyebacterium renale? |
Gram + facultative anaerobe. Survives in environment for ages. |
|

Clinical signs of pyelonephritis in cows? |
Chronic weight loss, poor appetite and poor milk yield. Failure of cows calf to thrive. Elevated temperature (39-39.8) |
|
|
What are clinical signs of pyelonephritis in cows relating to the urinary tract? |
Pollakiuria. Stranguria. Dysuria Discoloured urine with fleck of pus and blood. Staining of the tail and perineum with pus. Swishing tail. Colic signs. Urine foams. |
|
|
On rectal exam what would you notice with a cow with pyelonephritis? |
Grossly thickened ureters, thickened bladder. The kidney is enlarged and painful. |
|
What are further tests we can do to diagnose pyelonephritis in a cow? |
Dipstick- blood and protein. Grams stain urine- gram positive rods. Blood sample- chronic inflammatory changes like elecated fibrinogen and serum globulins and low albumin. Blood urea, nitrogen and serum creatinine are elevated in agonal stages. |
|
|
Treatment plan for a cow with pyelonephritis?Prognosis? |
Long course of penicillin 3-6 weeks Poor in advanced disease |
|
|
Control measures for pyelonephritis in a herd of cattle? |
Attention to environmental hygiene. Isolate affected animals. Regular cleaning of obsteric equipment. Feed acidifying diet if a herd problem |
|
|
What are causes of haematuria in cattle? |
Cystitis, pyelonephritis, enzootic haematuria. |
|
|
Cause of haemaglobinuria in cattle? |
Babesiosis. Bacillary haemoglobinuria. Post parturient haemoglobinuria. Chronic copper poisoning. Theileriasis. Lepto. |
|

What is the causative agent of bacillary haemoglobinuria? Pathogenesis? |
Clostridium haemolyticum. Fluke migrating through the liver leave focal anaerobic regions for spores to germinate and release toxin. |
|
|
When is bacillary haemoglobinuria usually seen? |
Summer and autumn in endemic areas. |
|
|
Signs of bacillary haemoglobinuria? |
Animals isolated with an arched back, febrile (40-41), tachypnoea, rectal blleding and bloody faeces. |
|
|
How can we control bacillary haemoglobinuria in endemic areas? |
Vaccination and routine flukicide. |
|
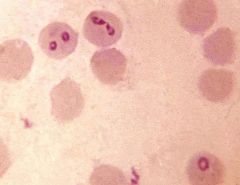
Causative agent of babesiosis? Vector? |
Protozoal red cell parasite -Babesia bigemina and babesia bovis Vector is the tick Ixodes ricinus. Seen in hill grazed cattle. |
|
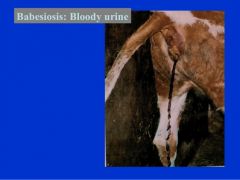
Clinical signs of babesiosis in cattle? |
Pyrexia- 40-41 Depressed and anorexic. Tachycardia and tachypnoea. Marked lymphadenopathy. Anaemia and haemoglobinuria after 1-3 weeks. MM- Red-> pale-> jaundice. Profuse diarrhoea. Death. |
|
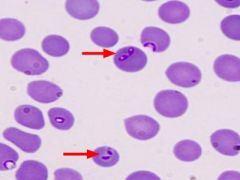
How can we diagnose babesiosis? |
Giemsa staining peripheral blood smear. Serology- PCR, ELISA,iFAT Haematology- severe anaemia. |
|
|
How do we treat a cow with babesiosis? |
Imidocarb dipropionate. ( Meat with-hold 213 days) (21 day milk) +/- a blood transfusion. |
|
|
How can we prevent babesiosis in cattle? |
Tick control.
Grazing management. Prophylactic use of imidocarb. Avoid bringing in naiive animals. |
|

What is the cause of enzootic haematuria? Onset? |
Bracken toxicity. Gradual over 7 weeks of ingestion. |
|
|
Signs of enzootic haematuria? |
Intermittent haematuria and anaemia. Ultimately weight loss, weakness, pyrexia, ptechia to haemorrhage. Fatal. |
|
|
What is post parturient haemoglobinburia related to? |
High yielding cows with hypophosphataemia. |
|
|
Signs of renal amyloidosis of cows? |
Older cow. Chronic weight loss Profuse diarrhoe- PLE- Protein losing enteropathy. Peripheral oedema. Enlarged kidneys. |

