![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
What is the simplest function of the respiratory system?
|
To provide oxygen and remove carbon dioxide.
|
|
|
What are the 5 steps of respiration?
|
1) ventilation - exchange of air between the atmosphere and the alveoli. (movement of air into and out of the lungs) 2) exchange of oxygen and carbon dioxide between alveolar air and blood in lung capillaries by diffusion. 3) Transport of oxygen and carbon dioxide through the pulmonary and systemic circulation by bulk flow. 4) exchange of oxygen and carbon dioxide between the blood in the tissue capillaries and cells in tissues by diffusion, 5) cellular utilization of oxygen and production of carbon dioxide. |
|
|
What is the difference between diffusion and bulk flow?
|
-diffusion is when a gas moves through a substance or across a membrane. -bulk flow is when substrate (ie blood) is flowing through a tube. |
|
|
The human respiratory tract can be divided into the upper and lower respiratory tract. which parts are in what? |
upper respiratory tract = nasal cavity, nostril, mouth and larynx lower respiratory tract = (everything below the larynx) i.e trachea, bronchi, lungs and diaphragm (note- the right lung has 3 lobes and the left lung has 2 lobes, each can function independently) |
|
|
What are the functions of the upper respiratory tract? (nasal cavity, mouth, pharynx and larynx)
|
1) Filtration - an important defence mechanism against infection, inhaled particles are trapped by hair and mucus in nasal passages, particles activate irritant receptors which trigger a sneezing reflex. Excess mucus also passes back to pharynx to be removed by swallowing, or is expulsed through the nose. 2) conditioning of air - air passing through the nasal cavity is warmed and humidified (100% saturation with water vapour) which is necessary for optimal gas exchange in the alveoli. Nasal passages have a rich blood supply for this purpose. 3) speech - larynx contains vocal cords: two folds of elastic tissue stretched across its lumen. These vibrate as air flows across them, producing sound. |
|
|
The lower respiratory tract is divided into two zones. What are these two zones? |
1) conducting zone (trachea, bronchi and bronchioles) 2) respiratory zone (respiratory bronchioles, alveolar ducts and alveoli) |
|
|
List some features of the conducting zone? (particularly the trachea and bronchi) |
- low resistance pathway for air flow - C-shaped bands of rigid cartilage to keep airways open - the trachealis muscle spans gaps between ends of cartilage bands. It contracts to aid expulsion of blockages e.g coughing reflex |
|
|
So what is the function of the trachealis muscle and where is it located?
|
in the trachea, it spans the gaps between the ends of the cartilage bands contraction of the trachealis muscle aids expulsion of blockages. |
|
|
List some features of the conducting zone, specifically the bronchioles...
|
- no cartilage - smooth muscle bundles. Normally relaxed, allowing air to reach the alveoli - contraction prevents irritants and particles from entering the alveoli |
|
|
In the conducting zone is there any gaseous exchange?
|
no gaseous exchange in the conducting zone (trachea, bronchi and bronchioles)
|
|
|
What is a function of the conducting zone region of the lower respiratory tract?
|
1) defence against microbes, chemicals and other foreign matter. (by mucociliary transport, foreign particles are trapped in mucus, continuously beating cilia moves mucus gel phase from the bronchioles up to the pharynx for ejection by coughing or swallowing) |
|
|
bronchioles have fewer cilia and less mucus than the upper airways. true or false? |
true
|
|
|
What constitutes the respiratory zone?
|
respiratory bronchioles, alveolar ducts and alveoli. (small amounts of gaseous exchange occur in the bronchioles, however most gaseous exchange occurs in alveolar ducts and alveolar sacs) |
|
|
The respiratory bronchioles branch into individual alveoli or alveolar ducts. Alveolar ducts and alveolar sacs (40-50 alveoli in each sac). List 3 features of alveolar ducts and sacs... |
- site of gaseous exchange - extensive blood supply - surrounded by capillaries - each alveoli is wrapped in a network of capillaries which is surrounded by the pulmonary artery - carries deoxygenated blood from the heart to the lungs - gets oxygenated at the alveoli - then pulmonary vein carries oxygenated blood to the systemic circuit |
|
|
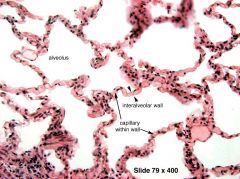
Lungs contain around 300x10`6 alveoli, each with a diameter of 0.2mm. Very high surface area of 85m2 and very thin walls of 0.2 micro meters, which maximises gaseous exchange. Two types of alveolar cells or pneumocytes, what are they? |
1) type 1 pneumocytes: flattened epithelium (for gaseous exchange) 2) type 2: thicker, secrete surfactant |
|
|
What are alveoli pores?
|
gaps between the alveoli Allow entry of air even if the duct is blocked. |
|

|
|
|
|
To summarise List the 3 primary functions of the lungs... |
1) provides oxygen and removes carbon dioxide 2) form speech sounds (phonation) 3) protection from microbes and other foreign matter |
|
|
List 4 additional functions of the lungs...
|
1) regulates blood hydrogen ion concentration (pH) as pH is linked to the concentration of dissolved carbon dioxide. 2) removal of micro-thrombi arising in systemic veins 3) removal or deactivation of circulating vasoactive hormones eg Bradykinin 4) Activation of angiotensin II |
|
|
Describe the activation of angiotensin II...
|
Angiotensin converting enzyme (ACE) on the surface of pulmonary endothelium converts angiotensin I into angiotensin II. |
|
|
what does angiotensin II do?
|
- vasoconstrictor. - triggers release of aldosterone from the adrenal cortex. |
|
|
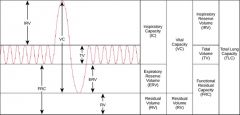
Define tidal volume (VT)...
|
In normal steady quiet breathing, the volume of air inspired is equal to the volume expired. = 500ml |
|
|
Define inspiratory reserve volume (IRV)...
|
The maximum amount that lung volume can be increased above the tidal volume (extra volume breathing in above the tidal volume) = 3000ml |
|
|
Define expiratory reserve volume (ERV)...
|
After expiring tidal volume, a further maximal exertion of the expiratory muscles a further volume can be expired. = 1200ml |
|
|
What is the residual volume (RV)...
|
Even after a maximal expiratory effort, the lungs cannot be completely emptied, a sizeable volume always remains. (air left in the lungs even after a big exhale) = 1200ml |
|
|
what are the lung volumes for an average young male?
|
tidal volume = 500ml inspiratory reserve volume= 3000ml expiratory reserve volume= 1200ml residual volume= 1200ml |
|
|
Lung volumes vary between individuals. What are lung volumes influenced by? |
age gender height |
|
|
Lung capacities are different to lung volumes. what are lung capacities? |
the sum of two or more 'volumes' are known as 'capacities'
|
|
|
the sum of the tidal volume and inspiratory reserve volume is the...
|
inspiratory capacity = 3500ml |
|
|
the sum of the tidal volume, inspiratory reserve volume and expiratory reserve volume is the...
|
vital capacity (breathe in as much as you can and then breathe out as much as you can) =4700ml |
|
|
the sum of the expiratory reserve volume and the residual volume is the...
|
functional residual capacity (FRC) (the volume of air in the lungs after a normal expiration) = 2400ml |
|
|
the sum of all four volumes (VT + IRV + ERV + RV) is known as the total lung capacity. It is... |
5900 ml
|
|
|
some lung volumes and capacities can be measured directly using a...
|
water spirometer (on inspiration the pen moves up, on expiration the pen moves down) |
|
|
To summarise... list the capacities of the lungs and their values... |
Inspiratory capacity (VT+IRV) = 3500ml Vital capacity (VT+IRV+ERV) = 4700ml Functional residual capacity (ERV + RV) = 2400ml total lung capacity = 5900 ml (IRV + VT + ERV + RV) |
|
|
Spirometer recordings of lung volumes and capacities...
|
|
|

|
|
|
|
Can RV (residual volume) and all of the capacities that include RV (FRC and TLC) be measured using a spirometer?
|
no because that lungs can't be completely emptied which means there is no 'baseline'
|
|
|
Define ventilation
|
the exchange of air between the atmosphere and the alveoli
|
|
|
define minute ventilation (VE)...
|
total ventilation per minute
|
|
|
define alveolar ventilation (VA)...
|
volume of fresh air reaching the alveoli per minute
|
|
|
how can minute ventilation be calculated?
|
minute ventilation = Respiratory rate x tidal volume e.g if the respiratory rate is 12 breaths/min an the tidal volume is 500ml then... VE = 500 x 12 = 6000ml/min or 6.0 L/min |
|
|
Is the alveolar ventilation; VA (volume of fresh air reaching the alveoli per minute) different from minute ventilation; VE (total ventilation per minute) ?
|
Yes- because gaseous exchange occurs primarily in the alveoli and minimally in respiratory bronchioles, while pharynx and the conducting zone of the lower respiratory tract do not contribute to this. (so gaseous exchange only occurs in the respiratory zone which is alveolar ventilation but minute ventilation involves both the conducting zone and respiratory zone- hence the terms are different) |
|
|
What is Anatomical dead space?
|
the volume from the top of the pharynx down to the terminal bronchioles is known as anatomical dead space. (ie the volume of air trapped in the conducting zone that is not involved in gaseous exchange) |
|
|
In adults the anatomical dead space is fixed, what is it?
|
150ml
|
|
|
How does anatomical dead space influence alveolar ventilation?
|
-150 ml of air remains in the conducting zone from the previous breath. -this means that of the 500ml tidal volume, 350ml will reach the alveoli for gaseous exchange, while 150 ml will remain in the conducting zone and not be absorbed. so, tidal ventilation = dead space + alveolar ventilation |
|
|
so alveolar ventilation =
|
minute ventilation - anatomical dead space e.g (500x12) - (150x12) = 4200 ml/min |
|
|
So what value is alveolar ventilation (assuming tidal volume is 500ml and respiratory rate is 12 breaths per minute)?
|
4200 ml/min as (500x12) - (150x12) = 4200 ml/min |
|
|
Although anatomical dead space is fixed, physiological dead space is not. What does this mean? |
In healthy lungs: anatomical dead space = physiological dead space. However, if some alveoli are poorly perfused (with blood), then no gas exchange occurs in those areas ---> this is the alveolar dead space. Physiological dead space = anatomical dead space + alveolar dead space (note in healthy people, alveolar dead space is zero) |
|
|
standard units of pressure are...
|
kPa (kilopascals) 1kPa = 7.5mmHg |
|
|
atmospheric pressure is Patm, what is partial pressure?
|
PO2 and PCO2 (capital P and in italics for partial pressures) |
|
|
when you have a mixture of gases, such as in air, fractional concentration is used...
|
FO2 (or %) e.g the FO2 in air is 21%. |
|
|
List the nomenclature for inspired, alveolar and arterial pressures...
|
Inspired = PIO2, FIO2 Alveolar = PAO2, FAO2 (capital A for alveolar) Arterial = PaO2, FaO2 (small a for arterial) |
|
|
How does ventilation occur?
|
Air moves from a region of high pressure to a region of low pressure. this can be defined by the equation: Flow (F) = difference in pressure (P1-P2) / Resistance to flow; R |
|
|
In ventilation, what are the important pressures?
|
atmospheric pressure (Patm) and alveolar pressure (Palv) F = (Palv-Patm)/ R |
|
|
Movement of air into and out of the lungs occurs when alveolar pressure becomes larger or smaller than atmospheric pressure, respectively... |
so, in between breaths when alveolar pressure is the same as atmospheric pressure, there is no flow of air.
|
|
|
The changes in pressure inside the lungs can be explained by Boyles law, What is Boyles law? |
The pressure (P) of a fixed amount of a gas (at a constant temperature) is inversely proportional to the volume (V) of the container in which it is placed. so smaller volumes = greater pressures |
|
|
Describe how the plural membranes of the lungs are involved in movement of the lungs...
|
The lungs are enclosed in a fluid-filled pleural sac. Cohesive forces exerted by the fluid between the pleural membranes (intra plural) cause the lung to adhere to the thoracic cage and this when the thorax changes its shape the lungs move with it. |
|
|
At functional residual capacity (FRC; at the end of a normal breath out), all the respiratory muscles are relaxed and inward recoil of lungs is balanced by an outward recoil of the chest wall. This generates... |
a negative pressure between the pleural membranes. so at FRC = negative intra-pleural pressure; PIP = -0.5kPa |
|
|
If the chest wall was opened, intra-pleural pressure would be normalised with atmospheric pressure. what would happen to the lungs and chest? |
1) lungs would collapse due to inward recoil 2) chest wall would expand due to outward recoil |
|
|
what is the trans-pulmonary pressure? PTP
|
the difference between the alveolar and intrapleural pressure PTP = Palv - PIP |
|
|
At functional residual capacity (end of a normal breath out), what is the trans-pulmonary pressure?
|
0.5 kPa
|
|
|
As the chest wall expands (in inspiration), intra-pleural pressure becomes what?
|
-0.7 kPa and trans-pulmonary pressure increases this lowers alveolar pressure so as the chest expands = intra pleural pressure becomes more negative. (think about the gap between the pleural membranes reducing in size, hence increase in pressure) |
|
|
List the sequence of events in inspiration (in terms of intra pleural pressure and trans-pulmonary pressure)...
|
1) nerves stimulate the diaphragm and other inspiratory muscles to contract, expanding the chest wall. 2) intra pleural pressure falls (becomes more negative to -0.7kPa (from 0.5 at normal)) 3) alveoli are expanded (due to increased trans-pulmonary pressure) causing an increased pressure difference across the alveoli. 4) pressure in the alveoli falls as they are expanded; greater volume (Boyles Law) 5) Increased pressure gradient from the mouth to the alveoli - air flows into the lungs. |
|
|
List the sequence of events in expiration (in terms of intra pleural pressure and trans-pulmonary pressure)...
|
1) nerves decrease firing to the diaphragm and intercostals, muscles relax 2) expanded chest wall recoils inward 3) Intrapleural pressure (PIP) and transpulmonary pressure (PTP) goes back towards pre-inspiration level (0.5kPa) 4) expanded lungs which have a greater elastic recoil, reduce in size 5) air in the alveoli gets compressed (Boyles Law) 5) Air flows out of the lungs |
|
|
As a reminder, what is intrapleural pressure and what is trans-pulmonary pressure?
|
1) intrapleural pressure is the pressure between the pleural membranes (visceral and parietal membranes) - gets negative in inspiration 2) trans-pulmonary pressure is the difference between the alveolar pressure and intra pleural pressure. when intra pleural pressure is decreased = trans pulmonary pressure increases. |
|
|
When may intra-pleural pressure be positive?
|
In forced expiration or high ventilation (abdominal muscles increase recoil of the diaphragm and speed shrinkage of chest wall and lungs) |
|
|
Describe the volume/pressure relationships during inspiration...
|
1) In Mid-inspiration - expanding the chest wall lowers intra pleural pressure which makes trans pulmonary pressure more positive. This expands the lung, making alveolar pressure negative = inward flow of air 2) At the end of inspiration - the chest wall is no longer expanding, but has to passively recoil. (alveolar pressure = atmospheric pressure = no air flow) |
|
|
Describe the volume/pressure relationships during expiration...
|
In mid-expiration, the lung is collapsing, this compresses the alveolar gas. So alveolar pressure becomes more positive (pressure increases), alveolar pressure becomes greater than atmospheric pressure, causes an outward airflow. |
|
|
what is the composition of gases in air (primarily nitrogen and oxygen) ?
|
FN2 = 0.79 (79%) FO2 = 0.21 (21%) FCO2 = 0.0004 (0.04%) (note when air is humidified it slightly dilutes the oxygen) |
|
|
What is the pressure exerted by a gas directly proportional to?
|
1) temperature 2) the number of gas molecules in a given volume (concentration) |
|
|
What is Dalton's Law (regarding partial pressures)?
|
Individual pressure of a particular gas (e.g O2) in a mixture of chemically non-reactive gases is called the partial pressure. Total pressure (P) = sum of all the individual partial pressures e.g Pa + Pb + Pc... |
|
|
example, in dry air, if atmospheric pressure is 101.3 kPa and the fractional concentration of oxygen is 0.21, what is the PO2 ??
|
101.3 x 0.21 = 21.2 kPa (atmospheric pressure x fractional concentration of a given gas = partial pressure of that gas) |
|
|
so to calculate partial pressure...
|
atmospheric pressure x fractional concentration of a given gas = partial pressure of that gas
|
|
|
At rest, how much oxygen is consumed by the tissues per minute? At rest, how much oxygen is extracted from the blood per minute? |
250 ml of oxygen is consumed by the tissues per minute so 250 ml of oxygen is extracted from the blood per minute |
|
|
At rest, how much carbon dioxide is produced by the tissues per minute? At rest, how much carbon dioxide is expired in the lungs per minute? |
200 ml of carbon dioxide is produced by the tissues per minute 200ml of carbon dioxide is expired in the lungs per minute |
|
|
why are the volumes different (i.e volume of oxygen consumed by tissues is 250ml but volume of CO2 produced is 200ml) ?
|
because oxidation of organic fuel produces water as well as carbon dioxide (so there is more than one product of aerobic respiration and hence CO2 produced is less) |
|
|
how do you calculate the respiratory quotient?
|
ratio of CO2 produced / O2 consumed = 200/250 = 0.8 |
|
|
At rest, alveolar ventilation(VA) is what?
|
4.2 L/min
|
|
|
How do you calculate the volume of oxygen transported per minute?
|
21% of the 4.2 L (or 4200ml) = 882 ml of oxygen |
|
|
Of this 882ml, 250ml is absorbed by the tissues so...
|
250ml of oxygen is used by the cells per minute.
|
|
|
In atmospheric air, what is the partial pressures of oxygen, carbon dioxide and water?
|
PO2 = 21 PCO2 = 0 PH20 = variable (humidity dependent) |
|
|
In the upper airways, what is the partial pressures of oxygen, carbon dioxide and water?
|
PO2 = 20 PCO2= O PH20 = 6.3 |
|
|
In the alveoli (gaseous exchange), what is the partial pressures of oxygen, carbon dioxide and water?
|
PO2 = 13.3 PCO2 = 5.3 (alveoli have extracted CO2 from the blood) PH20 = 6.3 |
|
|
In mixed expired gas, (mixing of alveolar air with air in anatomical dead-space) what is the partial pressures of oxygen, carbon dioxide and water?
|
PO2 = 16 PCO2= 3.5 PH20 = variable |

