![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
Lining of a normal bronchus
|
Pseudostratified columnar epithelium
|
|
|
Abnormalities of alveoli
|
1. Visible endothelial cells
2. More than one layer of RBCs 3. Expansion of walls 4. Loss of room architecture 5. Visible alveolar cells 6. Anything in the lumens |
|
|
Defense mechanisms of the lung
|
1. Brain
2. Free flowing body fluids 3. Mucociliary elevator 4. Phagocytosis (activation of neutrophils and macrophages, is of course, by itself a problem) 5. Immune system 6. Neurologic |
|
|
Effect of a tracheoesophageal fistula and esophageal origin of bronchus
|
Cyanosis when feeding
|
|
|
Bronchopulmonary sequestration
|
Lobes/segments lacking normal communication with bronchial tree (abnormal vasculature is common).
2 types - extralobar and intralobar. |
|
|
Extralobar bronchopulmonary sequestration (has its own pleura because it is external to the lung)
|
Congenital anomaly-diaphragmatic defect, pectus excavatum, and vascular malformations. Presents at less than 6 mos, M:F is 4:1.
|
|
|
Intralobar bronchopulmonary sequestration)
|
Acquired by repeated pneumonias, anyone can get it, 50% are over the ag of 20. Usually fed by systemic arterial system but dump into the pulmonary veins. 10% can have associated anomalies.
|
|
|
Problems with bronchopulmonary sequestration
|
1. Pneumonia/cough
2. Hypoplasia of other lung 3. Compression of normal lung 4. Abnormal x-ray 5. Cyanosis, feeding difficulty. |
|
|
Bronchogenic cysts
|
Extra buds of the foregut during development.
|
|
|
Problem with bronchogenic cysts
|
1. Infxn
2. Rupture 3. Compression of normal lung |
|
|
Bronchial atresia
|
Abnormal closure or absence of a bronchus. Causes overinflation of adjacent area. Can cause recurrent pneumonia, common in left upper lobe.
|
|
|
Effects of vascular pulmonary malformations
|
Dilated blood vessels due to abnormal communication. Causes cyanosis, dyspnea, failure of normal lung development, hemoptysis, hemothorax.
|
|
|
Osler-Weber-Rendu syndrome
|
Hereditary hemorrhagic telangiectasia. AD, many mucosal abnormal vascular connections
|
|
|
Septal deviation
|
Nasal blockage that can lead to infection. Congenital or acquired.
|
|
|
Uncomplicated obstructive lung disease: definition
|
Lung is enlarged and rate of airflow is reduced.
|
|
|
Histology of emphysema
|
Expanded alveoli, loss of rooms, thickened pink (hyaline) walls, and decreased vasculature.
|
|
|
2 patterns of obstructive disease
|
1. Hyperinflation
2. Focal alectasis with adjacent compensatory hyperinflation. |
|
|
Emphysema
|
Abnormal, permanent enlargement of airspaces (alveoli) where the alveolar walls are destroyed but not fibrotic.
|
|
|
Normal behavior of alveoli and bronchioles in relation to air flow
|
1. Elastic network and chest pressure collapse alveoli uniformly on beginning of exhalation.
2. Due to shared walls the collapse opens bronchioles, allowing all air to escape. |
|
|
Abnormal (emphysema) behavior of alveoli and bronchioles in relation to air flow
|
1. Lack of alveolar elasticity means they do not close uniformly.
2. Open alveoli crush the bronchioles closed as the chest compresses 3. Air does not escape from either the damaged portion or adjacent normal alveoli |
|
|
Is the amount of air in the lungs after expiration increased or decreased in uncomplicated emphysema?
|
Increased.
|
|
|
Five types of emphysema
|
1. Centracinar: upper lobes, heavy smokers, chronic bronchitis
2. Panacinar: alpha-1-antitrypsin deficiency 3. Paraseptal (bullous): near pleura, causing fibrosis and pneumothorax 4. Irregular: caused by scarring 5. Interstitial: trauma, obstruction, ventilation |
|
|
How does smoking contribute to emphysema?
|
1. Tobacco promotes formation of reactive oxygen species, which themselves damage tissue and recruit neutrophils via IL-8, LTB4, and TNF
2. The radicals inactivate alpha-1-antitrypsin, such that neutrophilic products are not broken down 3. The high levels of neutrophilic elastase damage tissue 4. Alveolar macrophages attempting to clear damaged tissue and foreign objects will make more elastase and metalloproteinases (remodeling proteins) that contribute to alveolar disfunction. |
|
|
What is the key ratio to consider when talking about emphysemal damage?
|
The protease (elastase)-antiprotease (alpha-1-antitrypsin) ratio. Not enough antiproteases allow inflammatory proteases to continually damage tissue.
|
|
|
What will the alveoli look like on gross examination of emphysema?
|
Dilated. The larger the dilation, the greater the loss of surface area for gas exchange (think of how many folds there are in a deflated balloon, and then the tension in an inflated one)
|
|
|
Microscopic hallmark of emphysema
|
Enlarged alveolar spaces lined by slightly thickened alveolar walls with thin fibrosis and relative avascularity. INFOLDING WILL BE LOST, AND SO WILL SURFACE AREA.
|
|
|
Hyperinflation
|
Dilated alveoli with thin walls and NO FIBROSIS due to loss of intrinsic elasticity.
|
|
|
Compensatory hyperinflation
|
Caused by focal atelectasis (collapse) so that other portions must hyperinflate to compensate.
|
|
|
Obstructive hyperinflation
|
When the gas cannot leave. It can be congenital, there can be a blockage in the lumen, etc.
|
|
|
How can you tell the difference between emphysema and hyperinflation?
|
Hyperinflation does not involve an inflammatory, fibrotic process. The walls just lose their stretch, not their basic structure.
|
|
|
Is there a pathologic definition for chronic bronchitis?
|
No, it is clinical.
|
|
|
Clinical definition of chronic bronchitis
|
Persistent productive cough for at least three months in at least two years.
|
|
|
How is chronic bronchitis different from emphysema?
|
For one, the lung involvement is widespread and almost immediate. Chronic bronchitis is also the compensatory response against irritation, IT IS NOT A CAUSE.
|
|
|
What is the disease process in chronic bronchitis?
|
Resistance to airflow due to clogged bronchial tree either by inflammatory corrosion or by mechanical obstruction. Work of breathing must increase to maintain normal rate.
|
|
|
Gross appearances of bronchitis
|
1. Change in mucosal color
2. Mucus plugs, mucus!! 3. Thickened, narrowed lumens. |
|
|
Microscopic appearance of bronchitis
|
1. Curschmann spiral: mucus shape cast in the shape of lumen .
2. Increase in size and number of mucous glands. 3. Increased goblet cells. 4. Decreased serous glands |
|
|
Etiology of bronchitis
|
1. Chronic irritation
2. Infection: does NOT CAUSE, but can aggravate. |
|
|
Sequelae of chronic bronchitis
|
1. COPD (when you add emphysema to the mix)
2. Cor pulmonale/cyanosis 3. Carcinoma (if smoking is a cause) 4. Bronchiectasis 5. COP 6. Fistulas 7. Chronic infection |
|
|
Bronchiestasis: definition
|
Permanent abnormal dilatation of the bronchial tree. You should not be able to see bronchi close to the pleural surface. If you can, then you have this condition.
|
|
|
3 types of bronchiectasis
|
1. Saccular
2. Varicose 3. Cylindrical |
|
|
Clinical appearance of bronchiectasis
|
Paroxysms of coughing, copious nasty pus-y sputum, hemoptysis, dyspnea.
|
|
|
Etiology of bronchiectasis
|
Bottom line: obstruction and infection.
|
|
|
Sequelae of bronchiectasis
|
1. Obstruction (bronchi are too wide!)
2. Fistulas/pleurisy 3. Cor pulmonale 4. Metastases 5. Amyloidosis 6. COPD 7. Chronic infection |
|
|
Types of asthma
|
1. Atopic: don't forget aspergillus
2. Nonatopic (asthmatic bronchitis) 3. Drug-induced 4. Occupational |
|
|
Pulmonary hypoplasia
|
defective development of both lungs (one may be more affected than the other) resulting in decreased weight, volume, and acini
|
|
|
Foregut cysts
|
abnormal detachment of primitive foregut and are most often located in the hilum or middle mediastinum
|
|
|
How do you repair foregut cysts?
|
Surgical resection is curative.
|
|
|
Pulmonary sequestration
|
a discrete mass of lung tissue without any normal connection to the airway system
|
|
|
Atelectasis
|
incomplete expansion of the lungs (neonatal atelectasis) or to the collapse of previously inflated lung
3 types: resorption (or obstruction), compression, and contraction atelectasis |
|
|
Resorption atelectasis
|
1. consequence of complete obstruction of an airway,
2. mediastinum shifts toward the atelectatic lung 3. caused principally by excessive secretions |
|
|
Compression atelectasis
|
1. Something in the pleural cavity compresses the lung
2. Can be due to pneumothorax 3.most commonly encountered in patients with cardiac failure 4. Mediastinum shifts away from atelectic lung |
|
|
Contraction atelectasis
|
local or generalized fibrotic changes prevent full expansion of the lung
|
|
|
Is atelectasis reversible?
|
Yes. Bronchiectasis is not.
|
|
|
Cytokine mediators of acute lung injury
|
tumor necrosis factor (TNF), interleukin (IL)-1, IL-6, IL-10, and transforming growth factor (TGF)-β
|
|
|
Progression of acute lung injury
|
acute respiratory distress syndrome or acute interstitial pneumonia
|
|
|
Examples of hemodynamic edema
|
Left-sided heart failure, increased hydrostatic pressure, pulmonary vein obstruction
|
|
|
The major diffuse obstructive disorders
|
emphysema, chronic bronchitis, hyperinflation, bronchiectasis, and asthma
|
|
|
Two major causes of obstructive lung disorders and their related diseases
|
1. Narrowing of the airway (asthma)
2. Loss of alveolar elasticity (emphysema) |
|
|
COPD
|
Emphysema w/chronic bronchitis
|
|
|
Major difference between centroacinar and panacinar emphysemal changes.
|
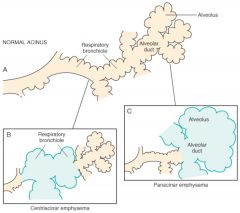
|
|
|
Associated causes of panacinar emphysema
|
Alpha-1-antitrypsin deficiency
|
|
|
Pathogenesis of emphysema (image)
|
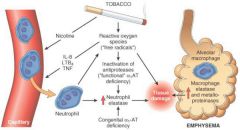
|
|
|
Classic presentation of emphysema
|
Classically, the patient is barrel-chested and dyspneic, with obviously prolonged expiration, sits forward in a hunched-over position, and breathes through pursed lips
|
|
|
How do you diagnose emphysema?
|
Expiratory airflow limitation, best measured through spirometry, is the key to diagnosis.
|
|
|
Blue bloaters vs. pink puffers
|
Chronic bronchitis vs. emphysema
|
|
|
Histologic study of the airways in chronic bronchitis reveals
|
(1) goblet cell metaplasia with mucus plugging of the lumen, (2) clustering of pigmented alveolar macrophages, (3) inflammatory infiltration, and (4) fibrosis of the bronchiolar wall
|
|
|
the ratio of the thickness of the mucous gland layer to the thickness of the wall between the epithelium and the cartilage
|
The Reid Index, increased in chronic bronchitis.
|
|
|
Proposed mechanistic malfunction in asthma
|
The inhibitory interferon-gamma from TH1 cells fails to stop overproduction of TH2, which in turn continue the asthmatic formation of reactive memory cells.
|
|
|
A busy pictorial representation of atopic asthma
|

|
|
|
Major chemokines implicated in causality of asthma
|
(1) leukotrienes C4, D4, and E4
(2) acetylcholine Minor: (1) histamine (2) prostaglandin D2 |
|
|
primary ciliary dyskinesia
|
poorly functioning cilia contribute to the retention of secretions and recurrent infections that in turn lead to bronchiectasis
|
|
|
Kartagener syndrome
|
bronchiectasis, sinusitis, and situs inversus or partial lateralizing abnormality
|
|
|
Usual flora cultured from bronchiectasis
|
Haemophilus influenzae and Pseudomonas aeruginosa specifically, and then a whole mix of everyone else.
|

