![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
|
What is the hallmark sign of myasthenia gravis?
|
Fatiguability on exertion
|
|
|
What happens at the neuromuscular junction with MG?
|
1. Antibodies to the nACHR impair the ability of ACH to bind to receptors
2. Antibodies are directed toward the nACHR at the NMJ of the skeletal mm 3. Results in: a. decreased number of functioning nACHR at the motor end-plate (blocks ACH transmission) b. reduced postsynaptic membrane folds (immune response) c. widened synaptic cleft |
|
|
What is the most sensitive test for MG?
|
Single Fiber EMG (SFEMG)
|
|
|
What are the classifications for MG?
|

|
|
|
What is the virus that carries the acute paralytic polio?
|
From one of 3 strains of enterovirus
|
|
|
How does one contract acute paralytic polio?
|
Contaminated food or water
|
|
|
How does acute paralytic polio initially present?
|
Fluelike infection
|
|
|
With acute paralytic polio, where is the damage and how much?
|
<1% developed paralysis - anterior horn cell damage
|
|
|
PPS is a combination of primary and secondary impairments, which are what?
|
Functional Limitations
Disability |
|
|
After how many years of neurological and functional stability will PPS occur?
|
30-40
|
|
|
What are current theories of how PPS ocurs?
|
Reactivation of the previous polio virus
Age-related changes superimposed with the already limited motor neuron pool Increased metabolic demand on giant motor units, with loss of individual motor units overuse and fatigue of the already weakened muscles Instability or failure of nerve impulse transmission at the NMJ |
|
|
What do macrophages have to do with GBS?
|
Macrophages attack and strip the myelin sheaths
In milder forms of GBS, the axons are left intact and the nerves are remyelinated in some cases, the axons also degenerate in AMAN (acute motor axonal neuropathy), macrophages invade the axon directly, leaving the myelin intact axonal loss is related to long-lasting or permanent muscle weakness seen in some patient’s |
|
|
What are key characteristics of AIDP?
|
Most common form of GBS
Often used synonymously with GBS Caused by an autoimmune responses directed against Schwann cell membranes Primarily demyelination Distribution of inflammation corresponds to clinical deficit |
|
|
What are key characteristics of AMAN?
|
most preceded by Campylobacter jejuni
DTR preserved, sensory nerves are not affected Also called Chinese paralytic syndrome (China and Mexico) - acute paralysis and respiratory failure Motor axonal loss and conduction block at nodes of Ranvier Auto-immune response directed against the axoplasm of peripheral nerves Seasonal and recovery can be rapid, or may be slow |
|
|
What are the differences between AIDP and AMAN?
|
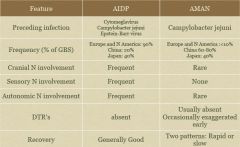
|
|
|
What are key characteristics of Miller Fisher Syndrome (MFS)?
|
Variant of GBS (rare compared to GBS but most common variant)
Descending paralysis, proceeding in the reverse order of the more common form of GBS Usually affects eye muscles first and presents with: opthalmoplegia ataxia areflexia |
|
|
What is the pathogenesis of GBS?
|
Significant associations with autoimmune reactions such as autoantibodies against myelin constituents
Because of damage to myelin sheath, saltatory propagation of action potential is disturbed slowed conduction velocity dyssynchrony of conduction disturbed conduction of higher frequency impulses complete conduction block |
|
|
What are the prominent differences between AIDP and CIDP?
|
CIDP is much less common
CIDP is slower, lowest point can be 4-8+weeks CIDP responds better to corticosteroids and IVIg and plasmapheresis Assymetry of symptoms are common in CIDP Proximal mm as much as distal mm Motor symptoms dominate in AIDP |
|
|
What are red flags for dizziness?
|
Dizziness with:
Exercise Orthostatic Position Change Loss of Consciousness Other Vertebral Basilar Signs and Symptoms (5 Ds) Sudden onset dizziness with: Severe lateropulsion Other central neurological sign and symptoms Headache (new and severe) |
|
|
What are the 7 D's?
|
Drop
Dizziness Diplopia Dysarthria Dysphagia Diseuphoric Decreased sensation |
|
|
When would you refer out a vestibular patient who has dizziness?
|
Dizziness associated with loss of consciousness with exercise
Need to rule out cardiovascular system |
|
|
Which testing would indicate a central vestibular dysfunction?
|
Extraocular Eye Movements
Smooth Pursuit Saccade VOR Cancellation |
|
|
What are the differences between peripheral and central vestibular dysfunction?
|
Peripheral Vestibular Disorders (PVD) include pathology of inner ear vestibular structures as well as the vestibular portion of the eighth cranial nerve.1 Such pathology diminishes available sensory information regarding head position and movement. These disorders include neuritis, labyrinthitis, bilateral vestibular loss, Meniere’s, BPPV, and vestibulopathy following surgical procedures (e.g. labyrinthectomy and acoustic neuroma).
Central Vestibular Disorders (CVD) primarily involve the vestibular nuclear complex and the cerebellum, as well as structures of the reticular activating system, midbrain, and higher centers of cortical function. Pathology of the central vestibular structures affects integration and processing of sensory input from the vestibular, visual, and somatosensory systems. The most common CVD include brainstem strokes, head trauma, migraine-related vestibulopathy, multiple sclerosis, and cerebellar degeneration |
|
|
What percent of patients who suffer a whiplash associated disorder (WAD) experience vestibular disorder?
|
50% incidence of vestibular dysfunction (30% BPPV & 20% canal paresis)
|
|
|
What is BPPV?
|
Motion evoked dizziness
|
|
|
What is the classic sign of BPPV?
|
Characterized by transient vertigo of seconds to minutes that is provoked by head/body position changes
Often diagnosed in beauty parlor or dentist office |
|
|
What is the diagnostic test for BPPV?
|
Dix-Hallpike
|
|
|
What is the treatment for BPPV? What is that treatment's success rate?
|
Treatment: Canalith Repositioning Maneuver (Eply)
Success rate: 80% with 1-3 treatments |
|
|
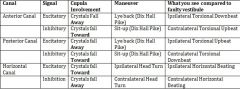
In BPPV, what eye motions will you see when going back to Dix hallpike, what is the eye motion you will see when you return to sit (both posterior, anterior and horizontal canal)?
|
Going to supine: nystagmus to the affeected side (the way the head is turned)
Returning to sit: nystagmus reverses |
|
|
What are clinical findings that would indicate BPPV?
|
Abnormal Dix-Hallpike w/ all other ocular/VOR findings normal (exception: can accompany other disorders of the labyrinth)
Abnormal CTSIB: often can persist after clearing |
|
|
What is Meniere's Disease?
|
"Plumbling problem of the inner ear"
Recurrent, spontaneous spells of intense vertigo lasting usually minutes to hoursvaccompanied by roaring tinnitus/aural fullness hearing loss (Meniere's Triad) Pathology: abnormal inner ear fluid dynamics (endolymphatic hydrops) Due to a low salt diet |
|
|
What are signs and symptoms of Meniere's Disease?
|
Transient acute shut down of vestibular function
|
|
|
What is involved in history taking on the dizzy patient?
|
Quality/intensity
Onset Associated Symptoms Temporal Pattern Contributing Factors |
|
|
VOR (vestibular ocular reflex) is what and what does it do?
|
The vestibulo-ocular reflex (VOR) is a reflex eye movement that stabilizes images on the retina during head movement by producing an eye movement in the direction opposite to head movement, thus preserving the image on the center of the visual field. For example, when the head moves to the right, the eyes move to the left, and vice versa. Since slight head movement is present all the time, the VOR is very important for stabilizing vision: patients whose VOR is impaired find it difficult to read using print, because they cannot stabilize the eyes during small head tremors. The VOR does not depend on visual input and works even in total darkness or when the eyes are closed. However, in the presence of light, the fixation reflex is also added to the movemen
|
|
|
Which tests are used to identify unilateral vestibular loss?
|
Head Thrust
Nystagmus Testing Head Shake CTSIB Gait Abnormal: corrective saccade, nystagmus, postural instability |
|
|
Which tests are used to identify bilateral vestibular dysfunction?
|
Slow VOR testing
CTSIB Gait Abnormal: Hx consistent with severe infection w/antibiotics Positive bilateral corrective saccades with head thrust testing at even slow speeds Often fall on Fukada or profound rotation Free falls on CTSIB 5/6 (vestibular conditions) Severely impaired gait, profound with eyes closed |
|
|
Which type of exercises are for habituation?
|
from the sitting position, lying sideways on 1 ear and waiting for 30 s; sitting up then lying down on the opposite ear
|
|
|
What would you see with an acoustic neuroma?
|
Pathology
Progressive to different degrees of vestibular loss then sudden complete permanent loss when tumor is removed Response to surgical removal varies depending on degree of loss prior to surgery and compensatory pathway integrity Prognosis Excellent with appropriate movement/challenge Long term commitment to exercise Vulnerable to decompensation even years later |
|

Name these orthotics
|

|
|
|
Which LE orthotics controls rear foot and midfoot?
|
SMO
|
|
|
Which LE orthotic blocks movement of ankle in all planes?
|
AFO-Solid Ankle
|
|
|
Which LE orthotic has good swing phase control, clears toe, and prepositions for stance?
|
AFO-PLS
|
|
|
Which LE orthotic has controlled ankle motion, can block PF, and may smooth out 2nd half of stance?
|
AFO-Articulated Ankle
|
|
|
Which LE orthotic applies an external extension moment to the knee to assist a weak quad?
|
AFO-Ground Reaction
|
|
|
How many points is the POMA (Tinnetti)? At which point level is a person high, moderate, or low risk?
|
Total Points: 28
High Risk: <19 Moderate Risk: 19-23 Low Risk: >23 |
|
|
How many points is the Berg Balance?
At which point level is a person considered fall risk, low fall risk, moderate fall risk, or high fall risk? |
Total Points: 56
Fall Risk: <45 Low Fall Risk: 41-56 Moderate Fall Risk: 21-40 High Fall Risk: 0-20 |
|
|
What is the epidemiology for ALS?
|
Overall incident is 0.4 to 2.4 cases per 100,000
The incidence increasing with each decade of life Average age at onset is mid-to-late 50s Men slightly more than women at 1.7:1 5-10% of pt’s with ALS, inherited as an autosomal dominant trait (familial ALS [fALS]) Rare cases of juvenile onset ALS are inherited in an autosomal recessive pattern The large majority of adult individuals with ALs have no family history of the disease (sporadic ALS) 70-80% of individuals develop limb-onset ALS, with initial involvement in the extremities 20-30% develop bulbar-onset ALS, with initial involvement in the bulbar muscles |
|
|
What is the cardinal sign of ALS?
|
Muscle Weakness
|
|
|
Is ALS caused by UMN or LMN?
|
Either
|
|
|
How is the UMN involved with ALS?
|
Muscle weakness
-Characterized by spasticity, hyperreflexia, clonus, pathological reflex (Babinski or Hoffmann sign) -Spasticity can eventually lead to contracture and deformities -Spasticity causes dyssynergic mvmt patterns, abnormal timing, loss of dexterity and fatigue -As the disease progresses, UMN signs may decrease |
|
|
How is the LMN involved with ALS?
|
-Focal, asymmetrical weakness in LE, UE or bulbar mm
-The weakness assoc with LMN loss causes more significant dysfunction than UMN loss weakness -Initially occurs in isolated mm, distally, followed by progressive weakness and functional limitations -Mm weakness leads to decreased ROM: joint subluxations, tendon shortening, contracture, adhesive capsulitis -The pattern and progression of LE weakness is characterized by greater losses of mm force in distal muscles compared to proximal mm |
|
|
What are clinical manifestations of ALS?
|
Muscle weakness
Fall (46% of ALS patients fall) Fatigue Fasciculations Hypreflexia Muscle Cramping Atrophy Pain |
|
|
What is the disease course for ALS?
|
Progressive and deteriorating
From pathology to impairments to functional limitations is inevitable Time from onset to death ranges from several months to 20+ years In most patients, death occurs 3-5 years Death usually occurs from respiratory failure |
|
|
What loss will you see in a spinal cord injury of the posterior cord?
|
Bilateral vibration and proprioception.
Preserved motor function Bladder dysfunction |
|
|
What loss will you see in a spinal cord injury of the anterior cord?
|
Motor function (corticospinal tract)
Pain and temperature (spinothalamic) |
|
|
What loss will you see in a spinal cord injury of the central cord?
|
Bilateral motor weakness
Arms > Legs Intact sensation above and below |
|
|
What are the signs of autonomic dysreflexia?
|
Elevation of BP
Headache Vasodilation Nasal Congestion |
|
|
What are the clinical subgroups of parkinson's?
|
Idiopathic: most common form, affecting 78% of pts
Secondary: results of other identifiable causes (virus, toxins, drugs, tumors, etc.) Parkinsonism-plus syndrome: conditions that mimic PD in some respects, but the symptoms are caused by other neurodegenerative disorders |
|
|
What is the leading cause of death and disability in young adults in the US?
|
TBI
|
|
|
What percent of TBI's do the following acount for:
Falls MVA Struck by or against something Assault/violence Other |
Falls: 29%
MVA: 20% Struck by or against something: 19% Assault/violence:11% Other: 13% |
|
|
What percent of all TBI's are considered moderate? Severe?
|
Moderate: 10-30%
Severe: 5-25% |
|
|
If you sustain a TBI you are ___ times more likely to sustain a second
|
3
|
|
|
If you have a second TBI you are ___ times more likely to sustain a third.
|
8
|
|
|
What is the typical age at time of injury for TBI?
|
15-24
|
|
|
How many people each year incur a TBI? How many of them die from it? How many are hospitalized and survive?
|
1.5-2 million incur
50K people die 230K hospitalized and live |
|
|
What is normal ICP?
|
4-15 mmHg
|
|
|
What are the 3 location a hematoma can increase ICP?
|
Epidural
Subdural Intracerebral |
|
|
What is the difference betwwen decorticate and derebrate rigidity?
|
decorticate rigidity-UE flexed/LE ext
-indicative of a lesion at or above the upper brainstem )above superior colliculus) decerebrate rigidity-UE and LE ext -indicative of a lesion located in the brainstem between the vestibular nucleus and the superior colliculus |
|
|
What is the gold standard used to document level of consciousness post TBI and now in ICU as well?
|
GCS
|
|
|
What are the 3 item observed for the GSC?
|
Eye Opening
Best Motor Response Verbal Response |
|
|
What are levels of mild, moderate, and severe brain injury as per the GCS?
|
Mild: 13-15
Moderate: 9-12 Severe: <8 |
|
|
What is the Rancho Los Amigos Scale for TBI?
|
Level I: No Response- Pt appears to be in a deep sleep and is completely unresponsive to any stimuli.
Level II: Generalized Response- Pt reacts inconsistently and nonpurposefully to stimuli in nonspecific manner. Responses are limited and often the same regardless of stimuli presented. Responses may be physiological changes, gross body mvmts, and/or vocalizations Level III: Localized Response- Pt reacts specifically but inconsistently to stimuli. Responses are directly related to the type of stimulus presented. May follow simple commands such as closing eyes or squeezing hand in an inconsistent, delayed manner. Level IV: Confused-agitated- Pt is in a heightened state of activity. Behavior is bizarre and nonpurposeful relative to immediate env. Does not discriminate among persons or objects; is unable to cooperate directly with tx efforts. Verbalizations frequently are incoherent and/or inappropriate to the environment; confabulation may be present. Gross attention to env is very brief; selective attention is often nonexistent. Pt lacks short- and long-term recall Level V: Confused-inappropriate- Pt is able to respond to simple commands fairly consistently. However, with increased complexity of commands or lack of any external structure, responses are nonpurposeful, random, or fragmented. Demonstrates gross attention to the env but is high distractible andlacks ability to focus attention on task. May converse on a social automatic level for short periods. Verbalization often inappropriate and confabulatory. Memory impaired, shows inappropriate use of objects, unable to learn new information Level VI: Confused-appropriate- Pt shows goal-directed behavior, dependent on external direction. Follows simple directions consistently and shows carryover for relearned tasks. Responses may be incorrect due to memory problems, but they are appropriate to the situation. Past memories show more depth and detail than recent memories. Level VII: Automatic-appropriate- Pt appears appropriate and oriented within the hospital and home; goes through daily routine automatically, but robotlike. Pt shows minimal to no confusion and has shallow recall of activities. Carryover for new learning but at a decreased rate. Able to initiate social or recreational activities; judgment remains impaired. Level VIII: Purposeful-appropriate- Recall and integrate past and recent events, is aware of and responsive to env. Carryover for new learning and needs no S once activities are learned. May continue to show decreased ability relative to premorbid abilities, abstract reasoning, tolerance for stress, and judgement in emergencies or unusual circumstances |
|
|
What is defined as the decreased level of awareness and intact eye opening and sleep-awake cycles but no ability to follow commands or speak?
|
A vegetative state
Persistent vegetative state:have no meaningful motor or cognitive function and complete absence of awareness of self or the environment • greater than 1 year for TBI or 3 mos for anoxic brain injury |
|
|
What are long-term behavior impairment typically seen with TBI?
|
sexual disinhibition
emotional disinhibition apathy aggressive disinhibition low frustration tolerance depression |
|
|
What factors help predict outcome after a TBI?
|
GCS
Duration of Coma Length of PTA |
|
|
What is the prognosis for TBI?
|
Duration of coma
> 2 weeks=moderate or severe injury <1 week=moderate disability or a good recovery Duration of PTA > 12 week=moderate to severe disability < 4 weeks=good recovery or moderate disability after one year GCS - mild: temporary or permanently altered mental or neuro sate - mod: some long term problems in one or more areas of life - severe: long term impairments in one or more areas of life |
|
|
What are the cranial nerves and how do you test them?
|

|
|
|
What are the dominant symptoms of parkinsons?
|
Tremor as main feature
Posture in stability and gait dynamics NOT bradykinesia |
|
|
How do you rate DTRs?
|
0: No response
1+: Present but depressed, low normal 2+: Average, Normal 3+: Increased, brisker than average; possibly but not necessarily abnormal 4+: Very brisk, hyperactive, with clonus; abnormal |
|
|
What is also know as a brain attack?
|
Stroke- The sudden loss of neurological function caused by an interruption of the blood flow to the brain
|
|
|
What is the etiology of an ischemic stroke?
|
Ischemic Stroke (75-87% ―Brain Infarct‖)
Occlusive: -Thrombosis -Embolism Low system perfusion pressures Deprives brain of needed oxygen and glucose, disrupts cellular metabolism, leads to injury and death of tissues. |
|
|
What is the difference between and MRI and CT in CVA?
|
MRI has greater resolution of the brain and its structural detail can be obtained as compared with a CT scan
MRI is more sensitive in the diagnosis of acute strokes |
|
|
What test would indicate a central vestibular dysfunction?
|
Tuning Fork
|
|
|
In BPPV, what eye motions will you see when going back to Dix hallpike, what is the eye motion you will see when you return to sit (both posterior, anterior and horizontal canal)?
|
|
|
|
How do you treat the posterior and horizontal canals for BPPV?
|
Brandt-Daroff ExerciseAnt/Post Canal BPPV:
A. Turn head 45 degrees away from affected side then rapidly lie on affected side. Wait for symptoms to cease plus an additional 20 sec. Quickly sit up, rotate head 45 degrees the opposite way and lie on unaffected side until symptoms cease plus an additional 20 sec. B. This method can be used for canalith dispersion or habituation. Modified Brandt-Daroff for Horizontal Canal BPPV – Cupulolithiasis (debris attached to cupula): A. Pt. lies prone with head flexed 30 degrees. B. Head is passively rotated quickly to the affected side, affected ear toward the floor. C. Head is rotated quickly to the opposite side, affected ear pointing up. This process can be repeated to dislodge debris. D. If nystagmus persists, repeat 10 reps, 3 x daily until pt. is symptom free for 2 days |
|
|
What are excitatory and what are inhibitory movements of the fluid/crystals in relation to the kinocillium in the cupula in both the posterior/anterior and horizontal canals?
|
In Horizontal Canal: Kinocilium in closer to the utricle
In Vertical Canals: Kinocilium in closer to the canal |
|
|
What is involved with end organ vestibular pathology?
|
Nerve conduction interruption
Fluid pressure/membrane rupture Hair cell destruction in cupula/macula Abnormal pressure communication Mechanical disruption |
|
|
What are different equlibrium and nonequilibrium tests?
|
Nonequilibrium Coordination Tests
Alternate nose-to-finger Finger opposition Pronation/supination Rebound test Tapping (foot or hand) Heel on shin Fixation or position holding Equilibrium Coordination Tests Standing, comfortable posture with normal BOS Standing, feet together (narrow BOS) Standing in tandem Standing on one foot Perturbations Standing functional reach Standing eyes open (EO) to eyes closed (EC); LOB without visual input =positive Romberg |
|
|
What is the zone of partial preservation?
|
complete injury, intact sensory and motor above S5 and below level of injury
|
|
|
In Brown Sequard Syndrome, what is lost contralateral?
|
Pain
Temperature |
|
|
In Brown Sequard Syndrom, what is lost ipsilateral?
|
Reflexes
Proprioception Discriminitive Touch |
|
|
Which tract deals with pain and temperature?
|
Spinothalamic
|
|
|
Which tract deals with loss of reflexes and a positive babinski sign?
|
Corticospinal
|
|
|
What is not a symptom of autonomic dysreflexia?
|
Tachycardia
|
|
|
By which mechanism can a man with a complete spinal cord injury have an erection?
|
Reflexogenic
|
|
|
How high does the chest raise during inspiration?
|
2.5-3 inches at the xyphoid
|
|
|
What is described as reaching it's highest point of severity, which is 4 weeks for GBS?
|
Nadir
|
|
|
How frequent is optimal pressure relief?
|
10-15 seconds/10 minutes
|
|
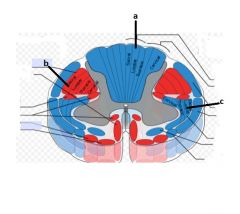
What is a, b, and c?
|
a- Medial Lemniscus
b- Lateral Corticospinal c- Lateral Spinothalamic |
|
|
T/F Increased respiratory rate is a sign of ICP
|
False
|
|
|
Following a stroke involving the middle cerebral artery, what is affected on the dominant side?
|
Aphasia
|
|
|
Following a stroke involving the middle cerebral artery, what is affected on the nondominant side?
|
Unilateral Neglect
Anosognosia Spatial Disorganization |
|
|
T/F Lateral Medullary Syndrome will not have severe weakness
|
True
|
|
|
What is function gait speed?
|
2.75 mph
|
|
|
What is the ideal height of a stair?
|
Less than 7 inches
|
|
|
What is the ADA height for handrails?
|
34-38 mph
|
|
|
What is ADA grade for a ramp?
|
1:12
|
|
|
What is ADA compliant ramp width?
|
36 inches
|
|
|
Which is ADA compliant door width?
|
32 inches
|
|
|
What is the most dangerous area of the house for a wheel chair bound person?
|
Bathroom
|
|
|
What percent of hysteria end up showing organic causes?
|
60%
|
|
|
What isn't a primary vital sign?
|
PO2
|
|
|
What controls thermoregulation?
|
Vascular
Metabolic Skeletal Muscle Sweating NOT respiratory |
|
|
What area is not affected by plaque from MS?
|
Brain Stem
|

