![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Skeletal muscles |
Voluntary movement is dictated by shortening of S-muscles. Flexion: moves bones closer together Extension: moves bones away from each other. *note: muscles often have opposing pairs. AKA antagonists |
|
|
|
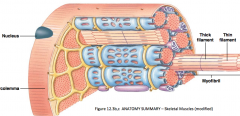
Muscle to muscle fibers (hpic) |
From out to in. 1Muscle Tendon (a bundle of fascicles) *nerve and blood vessels between 2) muscle fascicle (a bundle of fibers) 3) muscle fiber (a bundle of tissue) 4) nucleus |

|
|
|
Muscle terminology (hnotes) |
Muscle Cell : muscle fiber Cell membrane: Sarcolemma Cytoplasm: sarcoplasm modified endoplasmic reticulum: sarcoplasmic reticulum. |
sarcoplasm composed of Sarcoplasmic reticulum, myofibrils, mitochondria, glycogen granules. |
|
|
Visible features of muscles |

|
|
|
|
Visible features of muscle fibers (hpic myofibrils) |
|
|
|
|
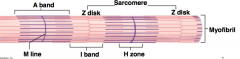
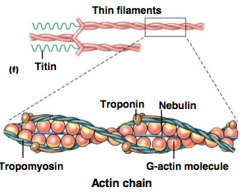
myofibril terminology (hpic notes) |
sarcomere = the distance between 2 z-disks A Band = collection of thick filaments (length of thick filament.) M-line = circumference of fiber |
composed of: troponin, actin, tropomyosin, myosin, titin, nebulin |
|
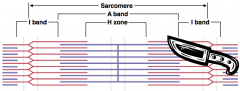
Sarcomeres (a close up) (hpic) |

thick filaments are composed of myosin. Thin filaments are composed of actin. |

|
|
|
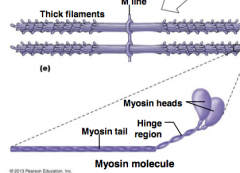
Myosin (hpic) |
Myosin tail: coiled and covalently bonded Myosin heads: globular, have ATPase and is what connects to actin and causes sarcomere contraction |
|
|
|
Actin (hpic) |
regulates skeletal muscle. resembles a string of pearls. 1 actin fiber can interact with 3 myosin thick filaments at once. |
|
|
|
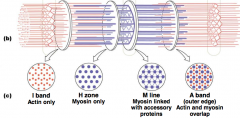
Sarcomere organization (inside) (hnotes) |
|
I band: Actin only H zone:myosin only M line: myosin linked with accessory proteins A band: actin myosin overlap |
|
|
I band vs A band |
I band changes (the distance between two thick filaments that shrinks as muscles contract) A band, length of thick filament, doesnt change with contraction |
|
|
|
Myofibril properties (hnotes) |
1)Linear contractile component of striated muscles. 2) Organized within muscle cells into a parallel array. 3) Composed of a serial array of sarcomeres. 4) Terminates in a myotendonus junction.
|
5)Fill most of the cytoplasmic space of striated muscles. 6) Muscle strength is proportional to the number of myofibrils in a muscle cell. 7) Surrounded by membrane structures. *note: you dont get more muscle cells, just more myofibrils within muscle fiber |
|
|
T-tubules (transverse tubules) |
T-tubule brings action potentials into interior of muscle fiber voltage gated channels along t-tubules sarcoplasmic reticulum stores Ca2+ ions.
|
|
|
|
motor units (h notes) |
A motor unit consists of one motor neuron and all the muscle fibers it innervates. A muscle may have many motor units of different types. |
A single motor neuron plus the muscle fibers (cells) it synapses on (innervates). Each muscle fiber is innervated by only one motor neuron. All of the muscle fibers in a motor unit are of the same fiber type. |
|
|
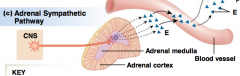
Autonomic pathways |
Autonomic targets: • Smooth and cardiac muscles • Some endocrine and exocrine glands • Some adipose tissue 3 types:parasympathetic, sympathetic, adrenal sympathetic |
|
|
|
parasympathetic (hpic) |
later |

|
|
|
Sympathetic (hpic) |
later |

|
|
|
Adrenal sympathetic pathway (hpic) |
later |
|
|
|
Neuromuscular junction |
? |

|
|
|
muscle action potential |
-voltage gated channels in cell membrane that will trigger muscle action potential -happens on both sides
|

|
|
|
MAP (muscle action potential) hnotes |
activates the DHP channel. in skeletal muscle, comes from cellular ER, (sarcoplasmic reticulum) all internal calcium mechanically operated |
|
|
|
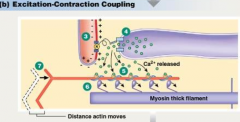
Timing of E-C coupling (hpic) |
action potentials in the axon terminal (top) and muscle fiber (middle) followed by a muscle twitch (bottom) |

|
|
|
what occurs in the latent period? |
there has to be a calcium signal, so calcium concentration rises during the latent period. twitch, (single response to a single action potential) |
|
|
|
E-C coupling (excitation contraction coupling) |
-Depolarization of the muscle fiber membrane creates an endplate potential (EPP) which spreads passively unitl it encounters nearby voltage gated Na channel. - Opening of the muscle’s voltage-gated sodium and potassium channels trigger the muscle’s action potential |
A muscle twitch is a single contraction-relaxation cycle A latent period is the short delay between the muscle action potential and beginning of muscle tension development |
|
|
Thin filaments |
later |
|
|
|
troponin and tropomyosin |
later |
|
|
|
initiation of contraction |
later |
|
|
|
contraction cycle |
later |
|
|
|
initiation of MAP (hpic) |

|

|
|
|
contraction cycles process hpic |
3)Action potential in t-tubule alters conformation of DHP receptor. 4)DHP receptor opens RyR Ca2+ release channels in sarco- plasmic reticulum, and Ca2+ enters cytoplasm. 5)Ca2+ binds to troponin, allowing actin-myosin binding. 6)Myosin heads execute power stroke. 7) actin filaments slide toward center of sacromere |
|
|
|
concentraction cycle relaxation phase hpic |
8)Sarcoplasmic Ca2-ATPase pumps Ca2 back into SR. 9) decrease in free cytosolic Ca2+ causes Ca2+ to unbind from troposin 10) tropomyosin re-covers binding site, when myosin heads release elastic elements pull filaments back to their relaxed positions |

|
|
|
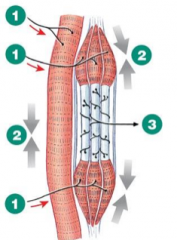
Muscle spindle hpic |
-capsule with specialized muscle fibers -nerve fiber (axon) wraps around these fibers -signal muscle stretch -action potentials when muscle is lengthened, silent when muscle contracts (shortens) |

|
|
|
Muscle spindle communication hpic |
1)Extrafusal muscle fibers at resting length 2)Sensory neuron is tonically active. 3)Spinal cord integrates function. 4)Alpha motor neurons to extrafusal fibers receive tonic input from muscle spindles. 5)Extrafusal fibers maintain a certain level of tension even at rest. |

|
|
|
Alpha gamma coactivation hpic |
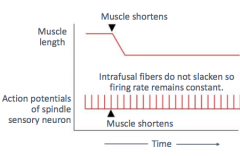
1) alpha motor neuron fires and gamma motor neuron fires 2) muscle and intrafusal fibers both contract 3) stretch on centers of interfusal fibers unchanged, firing rate of afferent neuron remains constant |
|
|
|
Alpha gamma coactivation cont |
The muscle spindle is actively modulated so it can provide information about muscle length even if the muscle shortens. Gamma motoneurons stimulate intrafusal fibers to contract and “reset” their sensory signals so the system continues to report muscle length changes. |
|
|
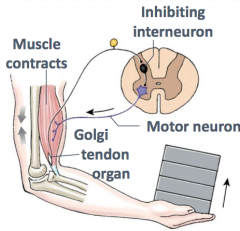
Golgi tendon muscle contraction hpic |
when load is on the joint, sends signal to CNS and inhibiting neuron sending to arm. |
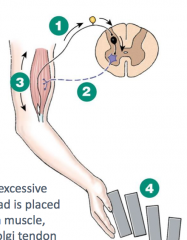
1) Neuron from Golgi tendon organ fires. 2)Motor neuron is inhibited. 3)Muscle relaxes. 4)Load is dropped. |
|
|
knee jerk reflex |
start with) stimulus, receptor, affluent path, integrating center
efferent path 1) effector 1(quads), response(kick) efferent path 2) effector 2(hams), response(retract)
|

|
|
|
Change and receptors |
Length change:muscle spindles Force change:Golgi tendon organs Pain : pain receptors
|
|
|
|
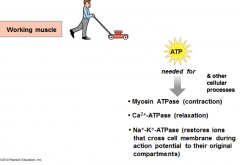
muscle metabolism hpic |
Muscle cells can form ATP via 3 different biochemical pathways: 1 - phosphorylation of ADP by creatine phosphate in muscle (rapid) 2 - oxidative phosphorylation of ADP in mitochondria (requires O2) 3 - phosphorylation of ADP by glycolysis in the cytoplasm (slow) |
|
|
|
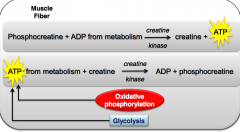
phosphocreatine hpic/notes |

|

|
|
|
1 - Phosphorylation of ADP by creatine phosphate stored in muscle (hpic) |
creatine phosphate (CP) is a “storehouse” of high energy phosphate which is accumulated during rest in muscle cells provides ATP during first few seconds of a contraction ATP production is rapid, but limited by the amount of CP stored in cell |
|
|
|
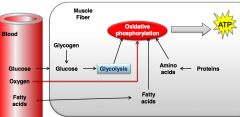
2 - Oxidative phosphorylation of ADP in mitochondria |
-multi-enzyme pathway that requires O2 -slower, so kicks in a little later than creatine phosphate -initially (first 5-10 min. of activity), glycogen provides major fuel -next 30 min, blood borne glucose and fatty acids contribute fuel, eventually giving way to mostly fatty acids |
|
|
|
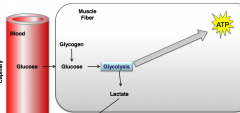
3 - Phosphorylation of ADP by glycolysis in the cytoplasm |
-kicks in during high intensity exercise -can produce ATP from glucose in the absence of O2 -produces small quantities of ATP from one molecule of glucose -in presence of large amounts of glucose, can produce large quantities of ATP -glucose can come from blood or from breakdown of muscle glycogen |
|
|
|
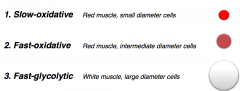
Muscle Fiber Types (hpic) |
Classified according to: -maximal velocity of shortening (i.e. how quickly myosin can hydrolyze ATP) -major pathway they use to form ATP |
|
|
|
Muscle fiber types part 2 (hpic) |

|

|
|
|
What factors could affect how much tension a whole muscle can produce? |
???? fill in later |
|
|
|
Peripheral fatigue |

|

|
|
|
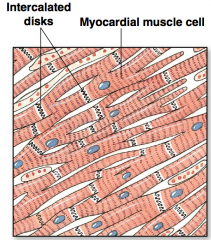
Cardiac muscle |
Composed of contractile cells - striated fibers organized into sarcomeres Autorhythmic cells, AKA pacemakers - signal for contraction -smaller and fewer contractile fibers compared to ontractile cells -do not have organized sarcomeres |
|
|
|
Cardiac vs skeletal muscles |
Cardiac muscles are.... -smaller and have single nucleus per fiber -branch and join neighboring cells through intercalated disks (desmosomes allow force to be transferred, gap junctions provide electrical connection) -T-tubles are larger and branch -Sarcoplasmic reticulum is smaller -mitochondria occupy 1/3 of the cell |
|
|
|
myocardial muscle cells (hpic) |
Myocardial muscle cells are branched, have a single nucleus, and are attached to each other by specialized junctions known as intercalated disks |
|
|
|
Questions: what is a myocyte? |
is the type of cell found in muscle tissue. Myocytes are long, tubular cells that develop from myoblasts to form muscles in a process known as myogenesis. |
|
|
|
Cardiac muscle desmosomes hpic |
Desmosomes are like rivets holding the cells together; Gap junctions are large cell to cell channels to permit local current flow |

|
|
|
Skeletal muscle movement process |
1) starts with action potential 2) down the sarcolema 3) to the t-tubules 4) DHP (dihydropyradines) is depolarized to tell another channel to open up (RYR receptor is opened) |
|
|
|
Cardiac muscle movement process |
1) action potential enters cell 2) voltage gated Ca2+ channels open so Ca2+ enters cell 3) Ca2+ induces Ca2+ release due to RyR 4) Local release causes Ca2+ spark 5) summed Ca2+ starts Ca2+ signal 6)Ca2+ ions bind to troponin to initiate contraction 7) relaxation occurs when Ca2+ unbinds from troponin 8) Ca2+ is pumped back into sarcoplasmic reticulum 9) Ca2+ replaced by Na+ |

|
|
|
EC coupling comparison (hnotes) |
In skeletal muscle, the DHPR is a voltage sensor that mechanically gates the calcium release from the ryanodine receptor on the SR. (in smooth muscle, most Ca2+ comes from ECF) |
In cardiac muscle, the DHPR is a L type voltage gated calcium channel. Calcium, that enters cytoplasm via the DHPR, binds to the ryanodine receptor to open it (ligand gated). –About 80% of the calcium needed for contraction comes from the SR –About 20% comes from the ECF via the Ltype Ca2+ channel in the T tubule |
|
|
Cardiac Muscle Contraction Can Be Graded (hnotes) |
Force generated is proportional to number of active crossbridges –Determined by how much Ca2+ is bound to troponin –This is the cellular basis of contractility • Sarcomere length affects force of contraction –This is the cellular basis of preload –Frank Starling Law of the Heart |
amount of Ca2+ determines size of contraction |
|
|
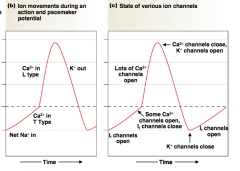
ACTION POTENTIAL OF A CARDIAC CONTRACTILE CELL (hpic) note, there is no summation |

|

|
|
|
Cardiac muscle action potential hnotes |

|
Cardiac muscle fiber: The refractory period lasts almost as long as the entire muscle twitch (means, muscle and relaxes, which is SUPER important in the heart) must pump, then refill. if no relax, youre dead. NOTE the hear does not TETANIZE |
|
|
Skeletal muscle action potential hnotes |

|
Skeletal muscle fast -twitch fiber: The refractory period (yellow) is very short compared with the amount of time required for the development of tension |
|
|
ACTION POTENTIALS IN CARDIAC AUTORHYTHMIC CELLS (*pacemaker potential, meaning no fast voltage gated channel) hpic |

|
|
|
|
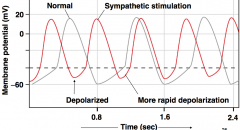
huge fact mindbomb (hnotes) |
nearly all our channels opened with depolarization, but for the heart ventricle, the channel opens for re-polarization activate action potentials spontaneously the longer it takes to go to threshold, the slower your contractions and slower the heartrate |
the action potential is brought out by a slow Ca2+ channel. as the Ca2+ closes and K+ opens, the cell repolarizes and the "funny" channels open |
|
|
Heart diagram (hnotes) |

|
blood starts superior/inferior VC go into right atrium. goes through tricuspid valve, into ventricle, then up through pulmonary semilunar valve. Oxygenated blood goes through pulmonary vein into left atrium, through bicuspid valve into left ventricle, up into the aorta and into the body. |
|
|
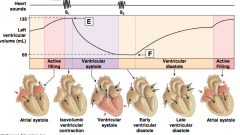
Order of events in action |
electrical event -> mechanical -> Pressure change -> valve/volume event |
|
|
|
Heart Valves Ensure One Way Flow in the Heart |
Two sets of heart valves ensure one -way flow –Atrioventricular valves –Between atria and ventricles –Tricuspid valve on the right side –Bicuspid valve, or mitral valve, on the left side –Semilunar valves –Between ventricles and arteries –Aortic valve –Pulmonary valve |
|
|
|
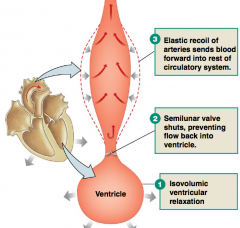
ventricular relaxation/contraction (2pics) note, semilunars do not have chordae tendinae |

|

|
|
|
Diastole vs Systole (meaning the ventricles) |
Diastole: is relaxation of the ventricle Systole: is the contraction of the ventricle IN THIS COURSE diastole/systole only refers to ventricles Atrial contraction will be known as active filling or atrial kick |
|
|

|

|

|
|
|
Filling of the atrium |
passive filling fills the atrium with more blood than active filling (atrial kick). Passive filling occurs due to pressure gradients isovolumentric state (when all (AV and semilunar valves) are closed due to pressure. |
|
|
|
Heart sounds hnotes |
First heart sound (happens when mitral and bicuspid close) –Vibrations following closure of the AV valves –“Lub” •Second heart sound –Vibrations created by closing of semilunar valve –“Dup” •Auscultation is listening to the heart through the chest wall through a stethoscope |
heart sound one-->going to heart sound two, is systole heart sound two --->going to heart sound one is diastole |
|
|
Wiggers diagram |
|

|
|
|
Stroke Volume and Cardiac Output hnotes |
Stroke volume -Amount of blood pumped by one ventricle during a contraction (EDV–ESV) = stroke volume –Average=70 mL •Cardiac output –Volume of blood pumped by one ventricle in a given period of time CO = HR ×SV –Average =5 L/min |
|
|
|
parasympathetic response |
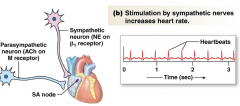
Parasympathetic stimulation hyperpolarizes the membrane potential of the autorhythmic cell and slows depolarization, slowing down the heart rate |

|
|
|
Sympathetic response |
Sympathetic stimulation and epinephrine depolarize the autorhythmic cell and speed up the pacemaker potential, increasing the heart rate |
|
|
|
Stroke volume(factors) hnotes |
Force of contraction is affected by – Length of muscle fiber – Determined by volume of blood at beginning of contraction – As stretch of the ventricular wall increases, so does stroke volume – Preload is the degree of myocardial stretch before contraction – Intracellular calcium concentration – More calcium binds more troponin – More crossbridges and more force production |
Stroke Volume • Frank - Starling law states – Stroke volume increases as EDV increases • EDV is determined by venous return • Venous return is affected by – Skeletal muscle pump – Respiratory pump – Sympathetic innervation of veins |
|
|
Frank starling law of heart |
Within limits, increase in venous return stretches the heart muscle and results in a larger stroke volume •Stretch adjusts sarcomeres to an optimal length •Benefit is that healthy heart keeps up with venous return so that there are no backups to increase stroke volume, increase venous return |
|
|
|
Contractility |
Any chemical that affects contractility is an inotropic agent –Epinephrine, norepineprine, and digitalis have positive inotropic effects –Positive inotropes increase contractility through the increase of intracellular calcium ions. |
|
|
|
Afterload (hnotes) |
Afterload is the combined load of EDV and arterial resistance during ventricular contraction (what we are pumping against) if blood pressure is too high, then ventricle contraction has to contract harder in order to keep valve open. bloodpressure is a measure of afterload.
|
to summarize: increasing afterload, decreases stroke volume. |
|
|
Blood pressure (pressure gradient) |

|
|
|
|
Hydrostatic pressure |
the pressure exerted on the walls of the container by the fluid within the containter. hydrostatic pressure is proportional to height of the column. |
once fluid begins to flow through the system, pressure falls with distance as energy is lost because of friction. this is the situation in the CV system. |
|
|
Ohms law |
Flow ∝∆P/R (change in mean arterial pressure / resistance in blood vessels) –Flow of blood in the cardiovascular system is –Directly proportional to the pressure gradient (∆P) (really mean arterial pressure) –Inversely proportional to the resistance (R) to flow |
|
|
|
Pressure change |
-if blood vessals dilate (R goes down) blood pressure decreases - if blood vessels constrick (R goes up), blood pressure increases. volume changes affect blood pressure in cardiovascular system such that an increase in volume increase blood pressure |
|
|
|
FLOW |
Flow ∝∆P/R (fluid will only flow in positive gradient) Flow ∝1/R (as R increases, flow decreases) |

|
|
|
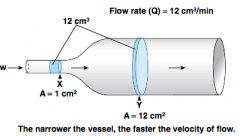
Poiseuille’s Law (hpic) |
R=8Lη/πr^4 or R∝Lη/r^4 •Resistance is proportional to length (L) of the tube (blood vessel) –Resistance increases as length increases •Resistance is proportional to viscosity (η), or thickness, of the fluid (blood) –Resistance increases as viscosity increases •Resistance is inversely proportional to tube radius to the fourth power –Resistance decreases as radius increases |

|
|
|
Resistance Opposes Flow |
Small change in radius has a large effect on resistance to blood flow –Vasoconstriction is a decrease in blood vessel diameter/radius and decreases blood flow (through an increase in resistance in a vessel) –Vasodilation is an increase in blood vessel diameter/radius and increases blood flow (through a decrease in resistance in a vessel) |
|
|
|
Flowrate is NOT the same as velocity of flow |
|
|
|
|
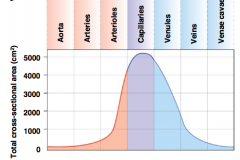
Types of vessels Hpic |
Arteries–high pressure, high velocity •Arterioles–high resistance, distribution, highly innervated by sympathetic nervous system •Capillaries–slow flow, thin walled •Venules–collection •Veins–lowest pressure, capacitance |

|
|
|
Arterial properties hpic note*elastic recoil maintains bloodflow even if there is no heart pump. |
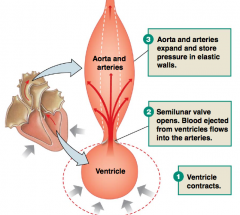
•Compliance –change in volume/change in Pressure –Compliance decreases with age –Veins more compliant than arteries •Elastic recoil –Ability of vessel to return to original shape after a stretch. –The elastic recoil of the arteries keeps the blood flowing during diastole. –Converts an on/off pump to a continuous, pulsatile blood flow |
|
|
|
Systemic circulation pressures hnotes |

|
Arterioles has pulse damping (pulse is no longer felt) capillaries and beyond, pulse is mostly gone Mean arterial pressure (diastolic pressure minus 1/3 pulse pressure) Pulse pressure = systolic minus diastolic pressure
|
|
|
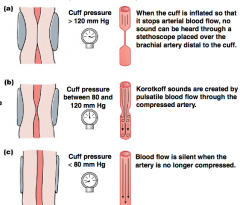
SPHYGMOMANOMETRY |
Arterial blood pressure is measured with a sphygmomanometer (an inflatable cuff plus a pressure gauge) and a stethoscope. The inflation pressure shown is for a person whose blood pressure is 120/80. |
|
|
|
Mean arterial pressure is determined by.... (2 pics) |

|
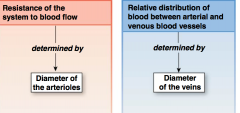
|
|
|
Arterial resistance(hpiC) |
Arteriolar resistance is influenced by both local and systemic control mechanisms –Local control –Sympathetic reflexes –Hormones, norepinephrine, serotonin, vascocontriction *epinephrine, only in skeletal muscles. |

|
|
|
Why is P wave so small and long |
the cells in the atria dont have purkinje fibers. purkinje fibers: line the inner ventricle, most efficient cardiac action potential conductors. |
|
|
|
Arteriolar Resistance |
•Myogenic autoregulation: a way we keep bloodflow constant even tho pressures changes, this exists in the brain, so we dont die. •Paracrines –Active hyperemia versus reactive hyperemia –Adenosine (depends on receptor for response) regulator of the coronary vessels •Hormones •Sympathetic control –SNS:norepinephrine –Adrenal medulla: epinephrine |
|
|
|
Active vs reactive hyperemia hpic |
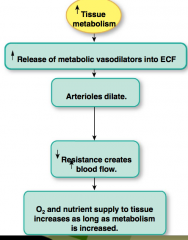
|

|
|
|
factors influencing peripheral blood flow hpic |

|

|
|
|
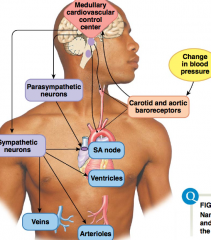
Regulation of Cardiovascular Function via the Baroreceptor reflex |
•Parameter regulated is the blood pressure. •Stimulus is a change in blood pressure. •Baroreceptor in the carotid arteries and aorta •Cardiovascular control center (CVCC) in the brain stem performs integration. •Sympathetic and parasympathetic motor pathways •Effects are SA node, ventricles and vascular smooth muscle |
|
|
Cardiovascular control |
|
|
|
|
INTEGRATION OF RESISTANCE CHANGES AND CARDIAC OUTPUT (hpic) |

|

|
|
|
RAAS |
•Low BP cause renin release from kidney •Angiotensinogen to angiotensin I •ACE •Angiotensin I to angiotensin II (vasoconstricter hormone) •Vasoconstriction and aldosterone release •Aldosterone increases plasma volume (increases stroke volume due to increase in pre-load) |
|
|
|
Takehome point |
•Angiotensin II is a vasoconstrictor and will increase vascular resistance and therefore will increase BP (and hydrostatic pressure) •Aldosterone is a hormone that works through the kidney to increase plasma volume and therefore to increase the blood pressure (and HS pressure) |
|
|
|
Arterioles |
-composed of smooth beta muscle -the resistance vessel -can be regulated one at a time by local factors if related to metabolism
|
|
|
|
Active Hyperemia |
-if muscles work harder, use more oxygen and generate more CO2, all vasodilaters. -nitric oxide very important vasodilater -causes changes in flow, not pressure (more blood to specific region, but not quicker) |
|
|
|
Perfusion |
areas that have been excluded builds up metabolites from local factors to open up capillaries to receive blood. |
|
|
|
Capillaries: Exchange hnotes |
•Plasma and cells exchange materials across thin capillary walls •Capillary density: is related to metabolic activity of cells •Capillaries have the thinnest walls –Single layer of flattened endothelial cells –Supported by basal lamina •Bone marrow, liver, and spleen do not have typical capillaries but rather sinusoids |
continuous capillaries have leaky junctions |
|
|
Velocity of bloodflow (hpic) *note: velocity is dependant on cross sectional area. maintains cardiac output, always has same volume of blood moving through system regardless of Cross sec area |

|
|
|
|
Capillary Exchange |
•Exchange between plasma and interstitial fluid occurs by paracellular pathway or endothelial transport •Small dissolved solutes and gases move by diffusion, depending on lipid solubility and concentration gradient (O2, CO2, glucose, ions, water) •Larger solutes and proteins move mostly by vesicular transport –In most capillaries, large molecules (including selected proteins) are transported by transcytosis (protein hormones) |
|
|
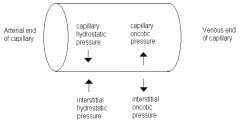
Starlings law of capillaries |
(Capillary hydrostatic pressure + interstitial oncotic pressure) - (interstitial hydrostatic pressure + capillary oncotic pressure) = Filtration pressure |
oncotic pressure: protein osmotic pressure plasma has higher osmotic pressure than interstitial because of these proteins. this is also called protein colloidal. |
|
|
Albumin |
biggest protein floating in your plasma that is the biggest factor in protein colloidal pressure (oncotic pressure) exists inside the capillary |
|
|
|
Capillary Exchange (starlings forces) hnotes |
•Bulk flow –Mass movement as a result of hydrostatic or osmotic pressure gradients •Absorption: fluid movement into capillaries –Net absorption at venous end –Caused by colloid (protein) osmotic pressure •Filtration: fluid movement out of capillaries –Caused by hydrostatic pressure –Net filtration at arterial end |
arteriole end has way more hydrostatic pressure than venous end of capillary |
|
|
The Lymphatic Sytem hpic |
•Return fluid and proteins to circulatory system •Pick up fat absorbed and transferring it to circulatory system •Serve as filter for pathogens
|

|
|
|
Veins are capacitance vessels |
•The veins are more compliant than the arteries. •They can accommodate more blood at a lower pressure. • 61% of the blood in body is found in the systemic veins and venules. • Mobilizing venous blood increases venous return (squeezing a vein increases arteriole pressure) |
|
|
|
Venous return |
•Factors that promote the return of blood from the veins to the heart will increase stroke volume via the Frank Starling Law of the Heart (preload). –Sympathetic stimulation to the veins –Respiratory pump –pressure changes with breathing that enhance blood return –Musculoskeletal pump –Increasing plasma volume (IV fluids, aldosterone, blood transfusion) |
|

