![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
1. What are common manifestations of Drug Induced Nephrotoxicity?
1b. What are the symptoms? 2. What is the most common presentation of DIN in hospitalized patients? 3. What often causes DIN in hospitalized patients? 4. What drugs are implicated in hemodynamically mediated kidney injury due to decrease in GC Hydrostatic pressure? 5. What does allergic interstitial nephritis cause? |
1. Decline in GFR, Increase serum creatinine and BUN
1b. Malaise, anorexia, vomiting, SOB, edema 2. Acute Tubular Necrosis 3. Aminoglycosides, Contrast Media, Cisplatin, Ampho B, Foscarnet, Mannitol 4. ACE inhibitors and NSAIDs 5. 3% of all cases of Acute Kidney Injury (AKI) |
|
|
1. Which patients are at high risk for drug induced nephrotoxicity?
2. How can we assess renal function when beginning new drugs? |
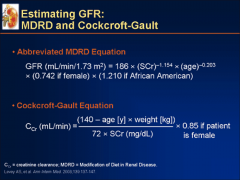
1. > 60y/o, diabetics, exposure to other nephrotoxic drugs, heart failure, GFR <60 ml/min
2. Cockcroft-Gault GFR Equation, or MDRD) |
|
|
1. What are common manifestations of Drug Induced Nephrotoxicity?
2. What are the symptoms? 3. What are the signs? What do PCT and DCT injury cause? |
1. Decline in GFR, Increase serum creatinine and BUN
2. Malaise, anorexia, vomiting, SOB, edema 3. Decresed urine output w/ above stressors (#1) Progression to volume overload and HTN Proximal Tubular Injury --> Metabolic acidosis w/ bicarburia and reduced serum Phosphate, uric acid, K+, and Mg+ Distal Tubular Injury --> Polyuria from failure to concentrate urine Metabolic acidosis from impaired urinary acidification HyperK+ from impaired Na+ recovery and K+ excretion |
|
|
Tubular Epithelial Cell Damage
1. Where is this damage often localized? 2. What causes this on a cellular level? 3. Which drugs cause this? |
1. PCT and DCT epithelia
2. Impaired mitochondrial function --> Oxidative stress 3. Aminohglycosides Radiocontrast media Cisplatin Amphotericin B Foscarnet Osmotically active agents: Immunoglobulins, Dextrans, Mannitol |
|
|
Aminoglycoside Toxicity
1. Incidence 2. Clinical Presentation 3. Pathogenesis 4. Risk factors 5. Management |
1. 58% of patients
2. Gradual rise in Serum Creatinine Decrease in CrCl after 6-10 days of therapy 3. Epithelial Cell Damage --> Reduction in GFR Obstruction of tubular lumen --> back leakage of glomerular filtration across damaged epithelium AGs collect in PCT cells --> Damage Mito, Ribosomes 4. Aggressive dosing, Synergistic drug tox, preexisting clinical condition 5. Watch Cr Clearance, Hydration, discontinuation of other nephrotoxic agents Dose drug according to CrCl and age |
|
|
Amphotericin B Toxicity
1. Incidence 2. Clinical Presentation 3. Pathogenesis 4. Risk factors 5. Prevention |
1. 80% when cumulative doses approach 4g
2. K+, Na+, Mg wasting Impaired urine concentrating ability Leak of H+ our of tubular lumen --> Distal Tubular acidosis 3. Tubular epithelial cell toxicity w/ increased tubular permeability and necrosis, atrial vasoconstriction and ischemia Medullary tubular epithelial cell necrosis and kidney injury 4. CKD, higher doses, volume depletion, and co-administration of diuretic and nephrotoxins (cyclosporine in particular) Rapid infusion 24 hour continuous infusion much better than 4 hour infusion 5. Liposomal preparations Limic cumulative dose Avoice co-administration w/ other nephrotox drugs Hydration |
|
|
1. Which patients are at risk of developing nephrotoxicity from ACE Inhibitors and ARBs?
|
1. CHF
Chronic Renal Disease Diabetic Nephropathy |
|
|
HMG-CoA Reductase Inhibitors - Statins
1. How does Rhabdomyolysis cause DIN? 2. What are the symptoms? 3. What increases the risk of Rhabdomyolysis? |
1. Lysis of myocytes --> Intratubular precipitation of myoglobin --> Acute, Severe kidney injury
2. Weakness, myalgia, tea-colored urine 3. Gemfibrozil, Niacin, CYP3A4 inhibitors (Erythromycin, Itraconazole) Drugs of abuse |
|
|
Crystal Nephropathy
1. What is it and what does it do? 2. What drugs/supplements/chemicals are insoluble at physiologic urine pH and is associated with intratubular precipitation in dehydrated, orliguric patients? 3. How does Foscarnet cause Crystal Nephropathy? 4. What do protease inhibitors cause? NOTE: Sulfonamides and Ciprofloxacin also cause Crystal Nephropathy |
1. Precipitation of crystals in the Distal Tubular Lumen --> Obstructs urine flow
2. Acyclovir, Triamterene, High dose Vitamin C, Ethylene glycol 3. Complexes with Ca2+ to form crystals in renal glomeruli --> GLomerulonephritis and tubular necrosis 4. (Indinavir) - Crystalurea, Crystal neuropathy, dysuria, urinary frequency, back and flank pain, nephrolithiasis |
|
|
Acute Allergic Interstitial Nephritis
1. Clinical Signs: when do they appear and what are they? 2. What drugs cause 90% of the cases? |
1. 5-14 days after drug therapy
Fever, Maculopapular rash, EOSINOPHILIA, sterile pyuria and hematuria, low-level proteinuria, oliguria HyperK+, HypoNa+, Polyuria, hypouricemia, low bicarb, metabolic acidosis 2. Acyclovir, AG, Ampho B, b-lactams, Erythromycin, Rifampin, Sulfonamides, Tetracyclines, Vancomycin, Trimethoprim-sulfamethoxazole, Acetazolaminde, Amiloride, Chlorthalidone, Loop diuretics, Triamterene, Thiazide diuretics. |
|
|
Beta Lactam Toxicity
Imipenem > Cephalosporins > Penicillin 1. How do they cause Acute Interstitial Nephritis? 2. How does the drug do this? 3. How does the immune reaction progress? |
1. Through an immune reaction
2. Behaves as a hapten --> immune response in the kidney 3. Proliferative lymphocytes and Macs invade tubular interstitium --> Tubular damage and 2ndary fibrosis |
|
|
Nephrotoxic Potential of Diuretics:
1. Furosemide 2. Hydrochlorothiazide 3. Triamterene 4. Mannitol |
1. Furosemide – hypokalemia, alkalosis, high urate, hyponatremia, azotemia (high BUN, creatinine).
2. Hydrochlorthiazide - hypokalemia, alkalosis, high urate, hyponatremia, hypercalcemia. 3. Triamterene – Hyperkalemia, acidosis (less potent and more toxic than amiloride) Triamterene precipitation in nephron. 4. Mannitol – filtered and not absorbed --> takes out water --> systemic hypernatremia, hyperkalemia Excessive mannitol can accumulate ECF --> cause edema, hyponatremia |
|
|
Mannitol
1. How does it cause DIN? |
1. Osmotic diruesis --> Shrinks ECF --> HyperNa+ and HyperK+
2. Vacuolization, Swelling and necrosis of nephron epithelial cells w/ decline in renal function Vasoconstriction of Glomerular Afferent Arteriole and Decreased RBF and GFR Result: Oliguria, Edema, Hyponatremia |
|
|
Contrast Media Nephrotoxicity
1. What causes it? 2. Who is at highest risk? 3. How can we protect these patients? |
1. combination of renal ischemia and direct toxic effects on renal tubular cells
2. Pre-existing renal insufficiency, DM, and CHF 3. 4 hrs before contrast medium injection and for at least 12 hours hours afterward: inject small dose of contrast medium and maintain continuous saline (0.9%) infusion. Encourage Hydration Discontinue Metformin 1 day before and several days later to avoid lactic acidosis |
|
|
Aspirin, NSAIDs, COX-2 Inhibition
1. What is the effect on the kidney? 2. What condition do these drugs cause in patients with impaired renal function? |
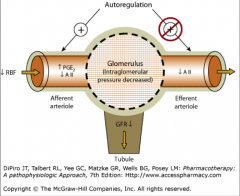
1. COX-2 --> increases PGE2 and PGI2 (Vasodilators)
Disabling COX-2 --> Decrease in RBF and GFR 2. Acute renal failure |
|
|
Immunosuppressives - Calcineurin Inhibitor Toxicity
1. What is THE major reason for stopping therapy? What percentage of patients does this happen in? 2. What drugs should these not be used with? 3. How do Immunosuppressives cause renal impairment? NOTE: Cyclosporine, Tacrolimus |
1. Renal Toxicity - 75% of patients
2. NSAIDs, Aminoglycosides 3. Dose dependent vasoconstriction of the AFFERENT ARTERIOLES --> Renal impairment in at-risk patients |
|
|
Fanconi Syndrome - Tetracycline
1. Pathogenesis 2. What compounds are lost in the urine? 3. What can loss of these compounds lead to? |
1. Impairment in the Proximal Tubule Function
Certain compounds that should be absorbed are excreted instead 2. Glucose, AAs, Urate, Phosphate 3. Growth Failure, Rickets, Abnormal bone mineralization (osteomalacia) |
|
|
Azotemia - Tetracycline
1. What is the pathogenesis? 2. What do lab tests show? |
1. Volume or Pressure of blood flow through the kidney drops --> Blood filtration drops or does not occur at all --> Waste products remain in the blood stream
2. Azotemia - Nitrogen-type wastes (Creatinine and Urea) accumulation |
|
|
Nitrogen Mustard Toxicity
1. What does Cyclophosphamide causedo? 2. What is required to avoid toxicity? 3. What is Ifosfamide for? 4. What is it always used with? |
1. Immunosuppressant, Hemorrhagic cystitis (acrolein)
2. Good hydration, MENSA if high dose or renal dysfunction 3. Hemorrhagic cystitis 4. MENSA (2-Mercaptoethane Sulfonate) |
|
|
Platinums: Cisplatin, Carboplatin, Oxaliplatin
1. What does Cisplatin do? 2. What is Carboplatin? 3. How is Carboplatin dosed? |
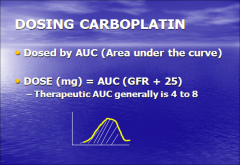
1. Cisplatin induces lipid peroxidation and free radicals in the Proximal Tubule --> Induce apoptosis or necrosis
2. 2nd Generation - Like cisplatin, but with LESS RENAL TOXICITY 3. Area Under the Curve - CALVERT FORMULA Dose (mg) = AUC (GFR+25) Generally 4-8 |
|
|
Bisphosphonates
1. What are the toxicities? 2. How can we avoid nephrotoxicity with these? |
1. Acute tubular necrosis
Collapsing focal segmental glomerulonephritis (FSG) 2. Monitor serum Creatinine prior to each Tx Withhold therapy if renally insufficient Adjust doses in patients w/ pre-existing chronic kidney dz |
|
|
Lithium
1. What is the toxicity? 2. What is the effect on the collecting duct? 3. What is a rare, slow progressing toxicity? |
1. Li+ Induced downregulation of Vasopressin (V2) --> Nephrogenic diabetes insipidus
2. Li+ --> Increases PGs in collecting duct --> degradation of AQP2 H2O channels --> Decline in urine concentrating ability 3. Chronic tubulointerstitial neuropathy |

