![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
178 Cards in this Set
- Front
- Back
|
palmer erythema, spider angiomatas, and gynecomatastia
|
cirrhosis
-all caused by hyperestrinism |
|
|
soft, yellow, greasy liver
|
fatty liver hepatic steatosis
|
|
|
astrerixis
|
Hepatic (portosystemic) encephalopathy
-flapping tremor and neurologic sign, caused by nitrogenous metabolites which can not be detoxified by the damaged liver |
|
|
most common primary malignacy of the liver
|
hepatocellular carcinoma
-often associated with Hep B infection |
|
|
inc in AFP(a-fetoprotien)
|
Hepatocellular carcinoma
-also present in yolk sac tumors |
|
|
triad of cirrhosis, skin pigmentation, and diabetes mellitus
"bronze diabetes) |
Idiopathic hemochromotosis
-primary defect in iron absorption leading to a net accumulation |
|
|
macronodular pattern on liver surface
|
posthepatic (postnecrotice, macronodular) cirrhosis
|
|
|
middle-aged femail with prutitus, jaundice, xanthomas, and antimitochondrial antibodies
|
primary billiary cirrhosis
-histologically characterized by granulomatous destuction of intrahepatic bile ducts |
|
|
billary tract disease, commonly seen in association with ulcerative colitis
|
primary sclerosing cholangitis
-histologically characterized by onion-skin fibrosis of bile ducts |
|
|
councilman bodies
|
viral hepatitis
-apoptotic hepatocytes |
|
|
hepatolenticular degeneration causing extrapyramidal motor signs
|
Wilson disease
-copper deposits in the liver, corniea of the eye (Kayser-Fleischer rings), and putamen and lenticular nucleai of the basal ganglia |
|
|
sudden right upper quadrant or epigastric pain with nausea, vomitting and leukocytosis
|
acute calculous cholecystitis
|
|
|
micronoducles on the liver surface in early stages
|
alcoholic cirrohsis
|
|
|
mallory bodies, neutrophilic infitrate, and hepatocyte swelling andnecrosis
|
alcoholic hepititis
->Mallory bodies associated ith accumulation of cytokeratin intermediate filaments in heptocytes |
|
|
most common liver disese in US?
|
alcoholic liver disease
|
|
|
fatal thrombbotic occulustion of the hepatic vein associated with poly cythemia vera and other hypercoagulable states
|
Budd-Chiari syndrome
|
|
|
obstructive jaundice with palpable enlarged gallbalder
|
carcinoma of the head of the pancrease or carcinoma of the extrabiliay ducts and ampula of Vater
Courvoisler law obstructive jaundice with palpable gallblader indicates probable tumor -jaundice iwth nonpalpable gallblader indicates probable gallstones |
|
|
obese multiparous women with fat intolerance
4 F's: female, fat, fertile, forty supersaturation of bile with cholesterol due to: 1. inc hepatocyte cholesterol secretion 2. dec bile salt / lecithin |
cholelithiasis (gallstones)
|
|
|
grossly distended abdomen, esophageal, varicies, caput meducsae, and hemorrhoids
|
cirrhosis, caused by portal hypertenstion and active portocaval anastomoses
|
|
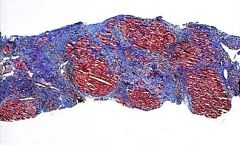
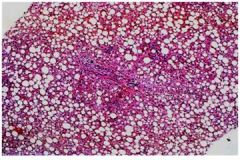
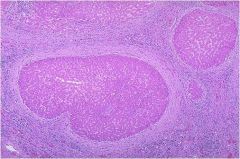
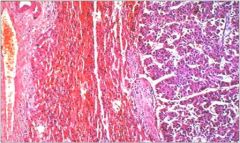
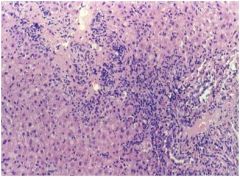
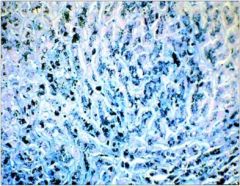
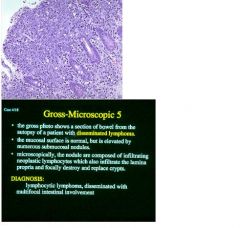
low mag trichrom stain
|
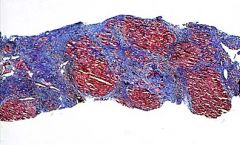
clinically the patient may have hepatice failure
|
|
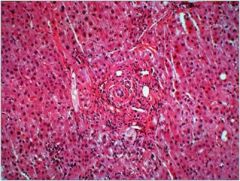
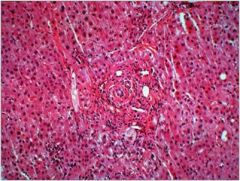
most likely eteology or cause for pathologic change shown in this liver biopsy
|
hemochromatosis
-inherited disease characterized by inc intestinal Fe uptake, result in systemic overload and eventually cellular toxicity and death |
|
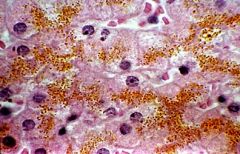
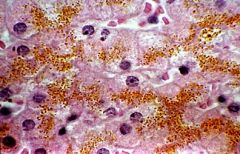
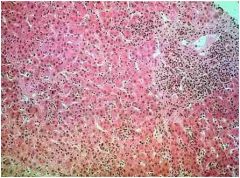
most likely clinicopathologic syndrome corresponding to changes in liver biopsy
|
cholestasis
-bile secretory impairment or failure, resulting in hepatocellular and serum accumulation of bile constituents and prominent elevation of alkaline phospatase and other enzymes derived from heptocyte canalicular membrane |
|
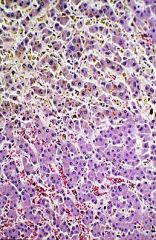
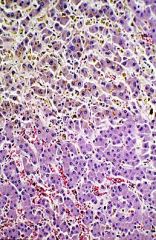
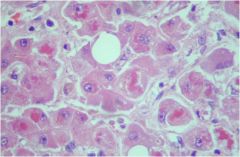
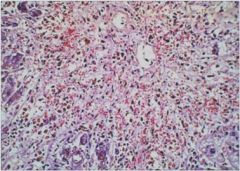
which of the following is false for this liver biopsy from an alcholic abuser?
a. histologic change reversible b. liver enlarged c. pt consumes 10 - 20 gm alcohol per day for 2 - 3 weeks d. serum alkaline phosphatatse may be elevated e. pt hepatic illness is most likely clinically mild |

which of the following is false for this liver biopsy from an alcholic abuser?
c. pt consumes 10 - 20 gm alcohol per day for 2 - 3 weeks pt must drink 80 gm/day to acheive reversible injury (steatosis) one beer = 10 gm EtOH |
|
|
< 3 mo
encephalopathy hypoglycemia bleeding renal failure elevated ast/alt |
acute hepatic failure
|
|
|
-have sx for years
-portal htn (acities & angiomata) -encephalopathy -may or may not have hypoglycemia -bleeding -renal failure mildly elevated ast/alt and T. Bili |
chronic hepatic failure
|
|
|
portal htn (ascities & angiomata)
synthetic derangements (dec albumin, inc PT, hypogonadism, wasting) possible encphalopathy |
cirrhosis with probable chronic hepatic failure
|
|
|
what liver disease causes the liver to dec in size due to shrinkage from collagenous scares?
|
cirrhotic liver (typically but not always)
|
|
|
what hepatic syndrome has alkaline phosphatase ice 3 to 10 times the normal?
|
cholestasis
|
|
|
< 3 mo
encephalopathy hypoglycemia bleeding renal failure elevated ast/alt |
acute hepatic failure
|
|
|
-have sx for years
-portal htn (acities & angiomata) -encephalopathy -may or may not have hypoglycemia -bleeding -renal failure mildly elevated ast/alt and T. Bili |
chronic hepatic failure
|
|
|
portal htn (ascities & angiomata)
synthetic derangements (dec albumin, inc PT, hypogonadism, wasting) possible encphalopathy |
cirrhosis with probable chronic hepatic failure
|
|
|
what liver disease causes the liver to dec in size due to shrinkage from collagenous scares?
|
cirrhotic liver (typically but not always)
|
|
|
what hepatic syndrome has alkaline phosphatase inc 3 to 10 times the normal?
|
cholestasis
|
|
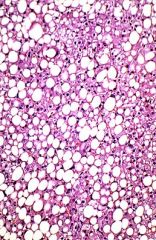
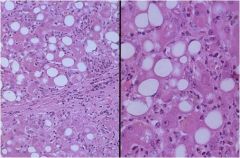
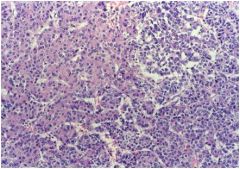
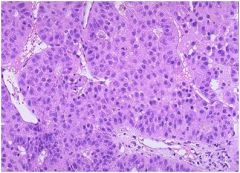
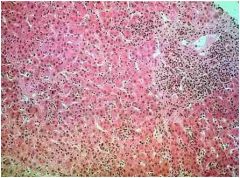
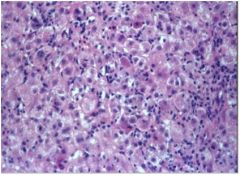
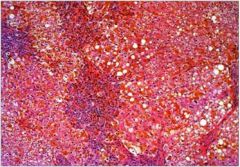
what is this hepatic syndrome?
|
Fatty change, asymptomatic or mild hepatocellular
injury/cholestasis syndrome |
|
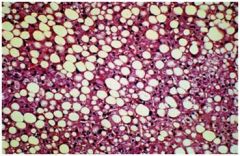
hepatic syndrome?
|
Fatty change, asymptomatic or mild hepatocellular
injury/cholestasis syndrome |
|

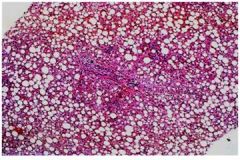
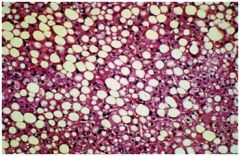
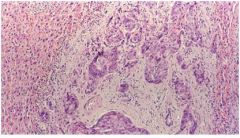
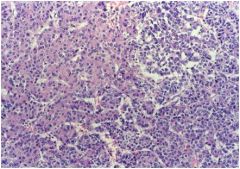
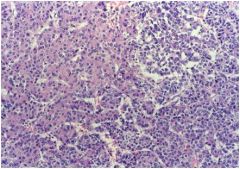
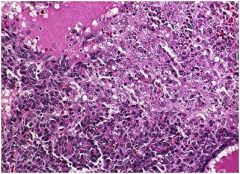
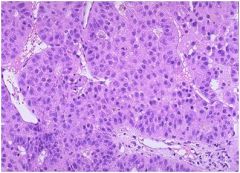
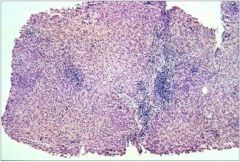
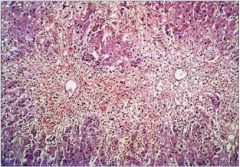
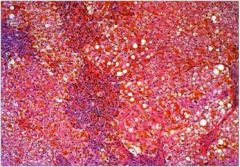
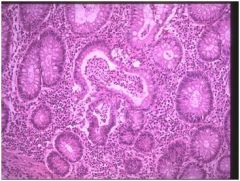
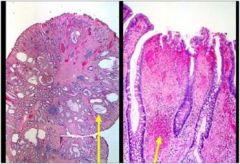
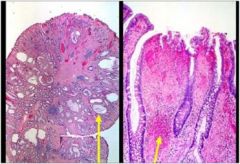
hepatic syndrome?
|

Cirrhosis, there are regenerative nodules
surrounded by “bands” of collagen |
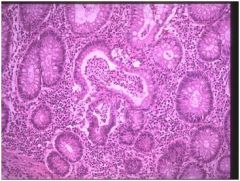
|
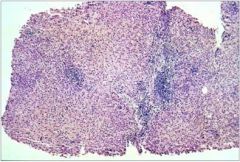
hepatic syndrome?
|
Cirrhosis, there are regenerative nodules
surrounded by “bands” of collagen |
|
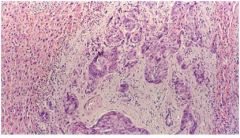
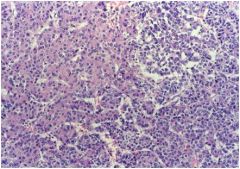
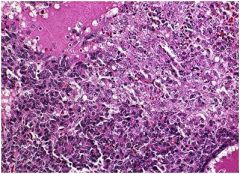
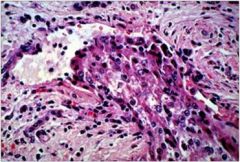
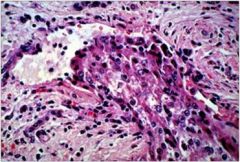
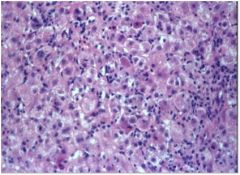
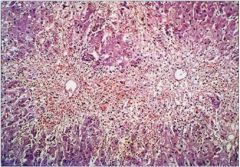
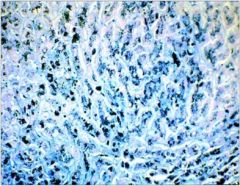
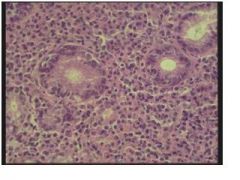
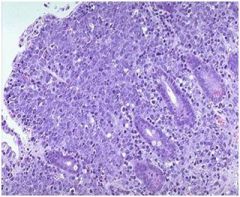
hepatic syndrome?
|
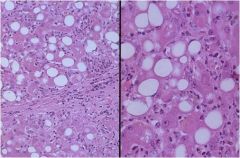
Alcoholic hepatitis (PMN's, Mallory hyaline, lobular disarray, steatosis, fibrosis syndrome), causes an acute cholestatic or hepatocellular injury syndrome
|
|
hepatic syndrome?
|
Alcoholic hepatitis (PMN's, Mallory hyaline, lobular disarray, steatosis, fibrosis syndrome), causes an acute cholestatic or hepatocellular injury syndrome
|
|
|
which of the following 3 hepatic syndromes is least likely to cause hepatomegaly?
a. cholestasis syndrome b. cirrhosis c. alcholic hepititis |
b. cirrhosis
Cirrhosis. Fatty change and alcoholic hepatitis increase liver size by virtue of intracellular accumulation and ↑ cellularity, respectively. Cirrhotic livers are typically (but not always) decreased in size due to shrinkage from collagenous scars. |
|
|
– ↑↑↑ alk phos with pruritus (deposition of bile acids
in skin) – xanthomas ( ↓ cholesterol excretion) |
cholestasis
|
|
|
inc ast/alt
|
heptocellular injury
|
|
|
elevated transaminase and alk phos
|
heptocellular carcinoma
|
|
|
anti-mitochondrial antibody (AMA) is a confirmatory test for what hepatic syndrome?
|
primary billary cirrohsis (PBC)
|
|
|
is copper elevated in cholestasis / duct obstruction?
|
Hepatic copper is ↑ in any cause of cholestasis/duct obstruction due to impaired
excretion into bile. |
|
|
why is copper elevated in Wilson's disease?
|
an inability to export copper from hepatocytes.
|
|
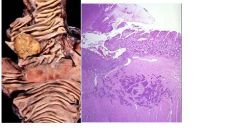
hepatice syndrome?
|
Adenocarcinoma (cholangiocarcinoma), with obvious glandular
differentiation. |
|
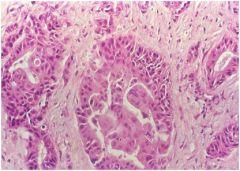
hepatic syndrome?
|
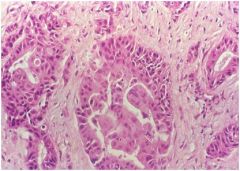
Adenocarcinoma
(cholangiocarcinoma), with obvious glandular differentiation. |
|
hepatic syndrome?
|
Hepatoblastoma, with “embryonal” appearance and “mesenchymal” differentiation. (Recall-this is a pediatric neoplasm.)
|
|
hepatic syndrome?
|
Hepatoblastoma, with “embryonal” appearance and “mesenchymal” differentiation. (Recall-this is a pediatric neoplasm.)
|
|
hepatic syndrome?
|
Hepatoblastoma, with “embryonal” appearance and “mesenchymal” differentiation. (Recall-this is a pediatric neoplasm.)
|
|
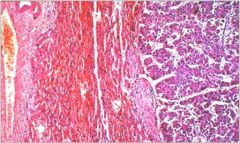
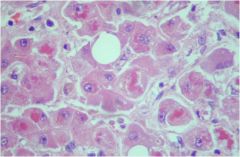
hepatic syndrome?
|
Hepatocellular carcinoma (HCC) in which tumor cells resemble hepatocytes (cord-like growth+resemblance to hepatocytes).
Note: HCC is associated with cirrhosis (of virtually any etiology) as well as HBV infection. |
|
hepatic syndrome?
|
Hepatocellular carcinoma (HCC) in which tumor cells resemble hepatocytes (cord-like
growth+resemblance to hepatocytes). Note: HCC is associated with cirrhosis (of virtually any etiology) as well as HBV infection. |
|
hepatic syndrome?
|
vascular invasion by the tumor, which is very typical of HCC. If this were extensive, it may have caused hepatic vein thrombosis, which presents with a syndrome of rapidly developing/worsening portal hypertension ( ↑ ascites, variceal bleeding) with tender hepatomegaly.
|
|
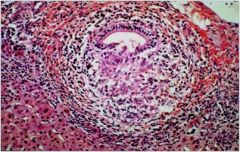
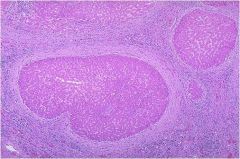
hepatic syndrome?
|

shows Primary Biliary Cirrhosis (PBC)
def: chronic, progressive, AUTOIMMUNE destruction of the medium sized intra-hepatic bile ducts, characterized by presence of anti-mitochondrial antibodies (AMA) pathology: “florid duct lesion” (mononuclear infiltration/granulomatous inflammation of bile duct epithelium) |
|
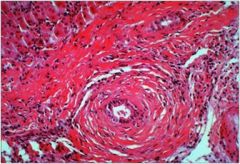
hepatic syndrome?
|
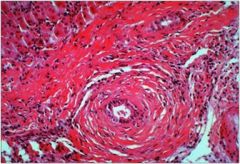
Primary Sclerosing Cholangitis (PSC) - idiopathic fibrosis and obliterative inflammation with segmental dilation of intra and/or extrahepatic bile ducts, often associated with UC
pathology: periductal concentric fibrosis |
|
hepatice syndrome
|
Primary sclerosing cholangitis (PSC) - indiopathic obliterative inflammation and fibrosis of intra and/or extrahepatic bile ducts
Pathology: periductal concentric fibrosis often with chronic inflammation |
|
hepatic syndrome?
|
Chronic active hepatitis, with periportal mononuclear infiltrates
and focal “piecemeal” necrosis of hepatocytes near the limiting plate. (Causes a chronic hepatocellular injury syndrome.) |
|
hepatic injury?
|

Chronic active hepatitis, with periportal mononuclear infiltrates and focal “piecemeal” necrosis of hepatocytes near the limiting plate. (Causes a chronic hepatocellular injury syndrome.)
|
|
hepatic syndrome?
|
Acute viral hepatitis, with “ballooning”, lobular “disarray” and
hyperplasia of Kupffer cells.(Causes an acute hepatocellular injury syndrome.) |
|
hepatice injury?
|
Acute viral hepatitis, with “ballooning”, lobular “disarray” and
hyperplasia of Kupffer cells.(Causes an acute hepatocellular injury syndrome.) |
|
hepatic syndrome?
|
Massive necrosis, with hepatocyte “dropout”, minimal
inflammation and little regeneration. |
|
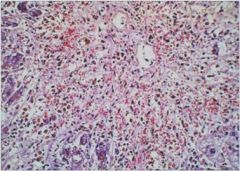
hepatic syndrome?
|
Massive necrosis, with hepatocyte “dropout”, minimal
inflammation and little regeneration. |
|
hepatic syndrome?
|
Fibrosis with ↑↑↑ iron compatible with hemochromatosis. This
disease causes gradual hepatic damage + damage to heart, endocrine glands, pancreas. |
|
hepatic syndrome?
|
Fibrosis with ↑↑↑ iron compatible with hemochromatosis. This
disease causes gradual hepatic damage + damage to heart, endocrine glands, pancreas. |
|
|
when does the liver size inc?
|
with alcholic or viral hepatitis
|
|
|
whendoes the liver size dec?
|
during fulminant hepititis / massive necrosis, which is characterized by shrinkage due to extensive cell loss
|
|

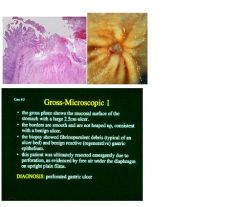
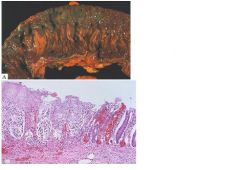
describe?
|

• Normal esophagus is lined by smooth mucosa that is nearly white or pink-gray
• longitudinal esophageal mucosal folds are pliable • the gastric mucosa is pink, darker than the esophagus, moist, and glistening • the junction of esophagus and stomach (squamocolumnar junction), or ‘Z’ line may be slightly irregular\ DIAGNOSIS • normal gastroesophageal junction |
|

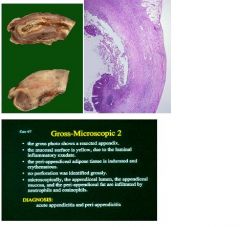
describe
|

• Normal esophagus is lined by smooth mucosa that is nearly white or pink-gray
• extending proximally from GEJ are red patches and streaks • areas of friability and bleeding are also present • DIAGNOSIS • esophagitis, consistent with acid reflux |
|

describe?
|

• The gastric mucosa erythematous (red) and ‘blotchy’
• numerous small superficial erosions are apparent • note the small, smooth-bordered, benign ulcer DIAGNOSIS • gastritis • benign ulcer |
|
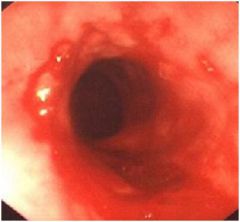
describe?
|
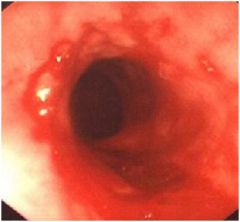
• Normal esophagus is lined by smooth mucosa that is nearly white or pink gray
• extending proximally from the GEJ are red patches and streaks • the Z line is irregular, with tongues of columnar appearing mucosa extending proximally • islands of squamous-appearing mucosa are present within the tongues of columnar-appearing mucosa DIAGNOSIS • Barrett’s esophagus (requires biopsy information) |
|

describe?
|
• This slide shows active esophagitis.
• The squamous mucosa and subepithelial tissue is infiltrated by eosinophils and neutrophils . • The presence of eosinophils is consistent with (but not diagnostic of) reflux esophagitis . • In response to the inflammation, the epithelium is reactive, as evidenced by the basal zone hyperplasia. |
|

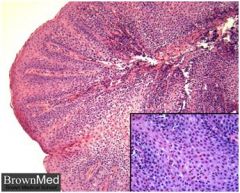
describe?
|
• These slides are an example of Helicobacter pylori-associated gastritis.
• The typical morphology includes plasma cells within the superficial lamina propria, and active inflammation of the pits (pit abscesses). • The inset is a silver strain (Warthin-Starry) that shows the curved bacilli. They do not invade, but are trapped within the surface mucous and attached to the apical surface of the foveolar cells. |
|
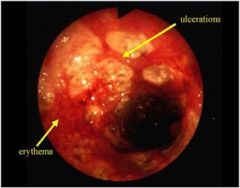
describe?
|

• Mucosa is erythematous and hyperemic
• erosions and ulcerations are present • pseudomembranes may be present • the mucosal vascular pattern is not apparent • linear ulcers may be present • disease is continuous from the rectum, but may stop abruptly DIAGNOSIS • suggestive of ulcerative colitis (history and biopsy will be helpful in evaluation) |
|
describe
|
• This slides shows chronic active colitis.
• The active neutrophils component • The glands are branched and irregularly spaced. • Paneth cells are present in this sigmoid biopsy(metaplasia). • This histology is typical of inflammatory bowel disease(IBD) and could represent either ulcerative colitis or Crohn’s disease. In the absence of granulomata, these entities can be indistinguishable on biopsy. • Therapy for IBD includes sulfasalazine, steroids, and other immunosuppressive agents. |
|
describe?
|
• The biopsy shows crypts atrophy (loss) (mucosal atrophy)
• The presence of mucosal atrophy, crypt distortion, and epithelial metaplasia (Paneth cells in the left colon) is diagnostic of chronic colitis. • There are few neutrophils infiltrating the epithelium (inactive colitis) • There is no dysplasia. (this is the part of the diagnosis in which you were most interested ) DIAGNOSIS • chronic inactive colitis • no dysplasia |
|
describe?
|
• This is an example of juvenile polyp.
• These are often present in younger patients (hence the name) and commonly present with rectal bleeding. • Grossly these polyps are typically smooth and glistening. • Microscopically, cystically-dilated non-neoplastic glands are present within the inflammatory stroma. • The disorganized appearance of the glands as well as disorganized strands of smooth muscle within the lamina propria have led some to conclude that these are hamartomatous polyps. • 85%-90% are solitary, and these are NOT associated with increased risk of cancer. Polypectomy is the only therapy necessary. • For a patient with numerous polyps and uncontrollable bleeding, colectomy may be necessary. An elevated cancer risk in these patients also leads to some advise colectomy. • juvenile polyposis coli is an autosomal dominant inherited disease |
|
describe
|
• This is adenoma.
• The cells are by Definition, dysplastic, with nuclear elongation pseudostratification. • Dysplastic morphology = neoplastic biology. • While not malignant, adenomas do have malignant potential and are considered premalignant. • Classification as a patient who ‘makes adenomas’ puts his patient in a higher risk category and requires more frequent colonoscopic surveillance with polypectomy. • Aggressive removal of adenomas at surveillance colonoscopy reduces the incidence of colon cancer. • For young patients with hundreds of adenomas ,the diagnosis is familial adenomatous polyposis, an autosomal dominant inherited disease. Colectomy prior to the development of cancer is the therapy of choice. |
|
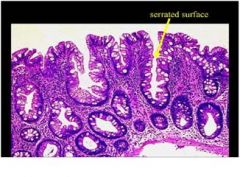
describe
|
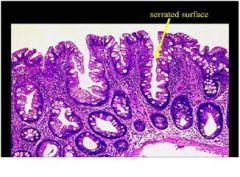
• This is hyperplastic polyp.
• Grossly these are typically small (<5mm) lesions most common the left colon. • Histologically the cells are not cytologically dysplastic, and, due to crowding, develop pseudopapillary infoldings with characteristic ‘sawtooth’ or ‘serrated’ shape. • At present these polyps have no clinical significance (unless mistaken for adenomas). |
|
describe
|
• This is an adenoma with intramucosal carcinoma in the stalk.
• The transformation to high grade dysplasia and intramucosal carcinoma is apparent as the cells become more crowded, and form cribriform and sheetlike structures. • Intramucosal carcinoma is present at the stalk margin, thus, this polyp deserves a surgical segmental resection in case it represents the surface of a deeply invasive carcinoma. • If the intramucosal carcinoma were only present at the surface of the polyp, well away from the margin, Polypectomy would be definitive therapy. No further therapy would be necessary in that case, as resected • intramucosal carcinomas have a <1% chance of metastasizing (due to the absence of lymphatics in the lamina propria of the colon). |
|

describe
|
see above
|
|

describe?
|
see above
|
|
describe?
|

see above
|
|
describe
|
see above
|
|
describe
|

see above
|
|
|
2 critical factors for diverticulosis?
|
1. higher intraluminal than intra-abdominal pressure
2. weak point in bowel wall, through which mucosa can herniate |
|
|
when does diverticulosis becomes diverticulitis?
|
1. acute inflammation of one or more diverticula
2. can be due to neck obstruction as with appendicitis 3. can result in serositis and rupture and perforation - weakened wall, little m. propria |
|
|
hallmark of hepatocellular carcinoma
|
elevated aminotransferase (transaminases)
|
|
|
problem is largely of "Nitrogenous" origin with some correlation with hyperammonemia
|
hepatic encephalopathy manifested by mental status disturbances, hyperreflexia, eeg changes and asterixis (flapping tremor)
|
|
|
-jaundice (bilirubin)
-xanthomas (from cholesterol) -pruritus (bile acids) |
signs and sx of Cholestasis
|
|
|
what systemic disease can present with:
1. constipation 2. peptic ulser disease due to hypergastrinemia 3. Multiple endocrine neoplasia synderome: develop diarrhea due to secreatagogue - producing tumor 4. pancretitis |
hyperparathyroidism, also see inc Ca and with MEN see zolinger-ellison syn and VIPoma
|
|
|
systemic condition associated with:
-GERD -hemorrhoids -gallstones -n/v |
pregnancy
|
|
|
what aspect of gi tract in HIV pt effect with:
1. candida 2. cmv 3. herpes simplex |
esophagus
|
|
|
what aspect of gi tract in HIV pt effect with:
1. mycobacterium avium complex (MAC) 2. TB 3. cryptosporidium |
small intestine
|
|
|
what drug toxicity is idiosyncratic and unpredictable?
|
acetaminophine
|
|
|
autosomal recessive inheritance, associated with HLA-A3 haplotype
inc intestinal iron uptake resulting in systemic overload and eventually cellular toxicty and death |
primary hemochromatosis
gold standard dx test - liver biopsy |
|
|
gingival hyperplasia, gingivitis, hemorrhage, petechia and ulceration of mucosa all relate to what disease?
|
leukemia
|
|

what disease is associated with these oral manifestations?
|

leukemia
|
|

what is this?
|

lichen planus - lower risk associated with malignancy, autoimmune, has branching features,looks like moss on a tree
|
|

what pt population is most likely to have this?
|

this is Moniliasis, also known as candidosis or thrush which is seen in pt whor are immunocompromised such as in cancer, tb, hiv, diabetes, etc
|
|

what is the cause of this?
|

fluorosis
|
|

what pt population should this be avoided in?
|

this is tetracycline staining which should not be given to pregnant women or young children as antibiotic tx
|
|

what is this and what disease first orally manifests in this way?
|

hairy leukoplakia is white in color and can NOT be scraped off and frequently the first sign of hiv infection
|
|

what is this and what is it a sign of?
|

this is erythroleukoplakia a pre-malignant lesion
|
|
|
major salivary gland tumors are
|
most often found in parotid glands
|
|
|
what lab finding is most associated with portal htn?
|
serum-ascites albumin gradient
|
|
|
achalasia
diffuse esophageal spasm (DES) nutcracker esophagus scleroderma dm, aging what type of dysphagia do all of these have in common? |
esophageal motor dysphagia
-difficulty with peristalsis, smooth muscle spasm, les fxn also called TRANSPORT dysphagia |
|
|
-cva
-polyositis -MG -circophyryngeal achalsia -zenker's (pharyngoesophageal) diverticulum what type of dysphagia do all of these have in common? |
Oropharyngeal dysphagia - difficulties with swallowing mechanism
also refered to as TRANSFER dysphagia |
|
|
what condition has less incompetence (always open) and aperistalsis in distal 1/2 of esophagus?
|
scleroderma bc smooth mucle inflitrated and atrophy from collagen deposition
|
|
|
what condition presents as dyspagia and chest pain made worse by emotional distress and by drinking hot fluids
|
diffuse esophageal spasms (DES)
|
|
|
failure if LES to fully relax after swallowing
loss of autonomic (auerbach's) ganglia in the body of the esophagus and lower esophaeal sphincter area resulting in esopheageal dilation |
achalasia
this is a type of esophageal motor dysphagia often called transport dysphagia |
|
|
what type of acute pancretitis has the highest mortality
|
severe or necrotizing acute pancretitis
|
|
|
what can cause all of the following:
-gastric cancer of body and antrum (distal stomach) -gastric ulcer -duodenal ulcer -gastric lymphoma |
h. pylori
|
|
|
what three conditions would fasting have little or no effect on diarrhea?
|
1. cholera - exogenous luminal stimuli from bacteria toxin
2. VIPoma - endogenous humoral peptide from tumor enters blood and stimulates enterocytes to secrete 3. celiac sprue - intrinsic crypt hyperplasia results in increased secretion |
|
|
UES myotomy (incision of sphincter muscle) or Botulinum toxin (Botox) is used for the treatment of what disease type?
|
oropharyngeal dysphagia
|
|
|
the following are used to dx what condition?
1. serology - measuring antibodies 2. rapid urease test (CLO-test) on biopsy 3.C13 or C14 - urea breath test 4. stool test |
gastritis due to h pylori
|
|
|
what condition is dx with the following tests?
1. serology: anti-parietal cell antibodies, anti-IF antibodies 2. serum gastrin levels very high due to loss of neg feedback to antral G-cells 3. EGD and biopsy - see mucosal atrophy 4. schilling test - measuring vit B12 absorption |
autoimmune gastritis
|
|
|
type of colon cancer?
sx: -crampy abdominal pain -constipation -streaks of blood mixed wit stool |
sigmoid colon cancer
|
|
|
how is Zollinger -Ellison syndrome (gastrinoma) dx?
|
fasting serum gastrin levels - usually elevated also see antral G-cell hyperplasia and achlorhydria
secretin stimulation test - in gastromia pt see inc in gastrin levels |
|
|
what do the following cause?
1. steatorrhea 2. colon 3. bile salt malabsorption 4. fatty acid malabsorption |
hyperoxaluria - excess urniary oxalate, bc calicum usually binds to oxalate but with fatty acid malabsorption the fatty acids bind to the calcium leaving the oxalate to be absorbed in the colon
|
|
|
rod shaped bacilli which infiltrate the lamina propria of the small bowel mucosa by destending PAS positive macrophages and villous blunding (proximal small bowel > ileum)
|
Whipples's diseae due to tropheryma whippelii
|
|
|
all of the following are associated with:
1. appendiceal carcinoid tumor 2. increased serum serotonin 3. metastitic disease 4. diarrhea |
carcinoid syndrome
|
|
|
what colon related disease risk of cancer is directly related to extent, duration of disease and age of sx onset?
|
ulcerative colilits
|
|
|
idiopathic fibrosis and obliterative inflamation with segmental dilation of intra and/or extrahepatic bile ducts, often associated with IBD (70% have UC)
|
primary sclerosing cholangitis (PSC)
|
|
|
what IBD has the discriminating feature of deep fissues / linear ulcerations?
|
Crohn's disease
|
|
|
what disease is characterized by:
-hypercalmeia -hemorrhage -abdominal pain -fat accumulation in acinar cells -respiratory distress |
acute pancreatitis
|
|
|
all of the following are predisposed to form ___?____
1. chronic hemolysis 2. inc chenodeoxycholic acid secretion 3. DM 4. dec bile salt enterohepatic circulation |
gallstones
|
|
|
Fe deficient anemia
glossitis cheilosis are a tetrad of sx for what syndrome? |
Plummer-Vinson Syndrome
-associated with inc risk of upper esophageal squamous cell carcinoma |
|
|
webs in the distal esophagus at or just above the gastroesophageal jxn associated with hiatal hernia
|
schatzki rings
|
|
|
protien folds incorrectly and is retained in the RER accumulating within the heptocytes appearing as cytoplasmic globules which statin with PAS stain
|
alpha - 1 antitrypsin deficiency
-combined progressive injury of hepatic / pulmonary tissue injury due to inheritance of mutated protease inhibitor (Pi) which is normally synthesized in the liver |
|
|
what structural disorder is associated with the following:
1. cardiac malformations 2. esophageal atresia 3. upper esophagus ends in a blind pouch 4. associated with aspiration |
congenital trachoeo-esophageal fistula
|
|
|
adenoma (gland-forming carcinoma) derived from intrahepatic bile ducts
-no bile production -intense desmoplastic (fibroblastic )rxn to tumor cells |
cholangiocarcinoma
|
|
|
hemorragic/necrosis surrounded by granulation tissue and fibrosis
-also lack true epithelial lining |
pancreatic pseudocyst
|
|
|
disease with polyps that do not have malignant potential but pt has inc risk of carcinoma at other sites including breast, pancrease, lung, gynecologic
|
peutz-jeghers polyposis
|
|
|
polyps disease that is hereditary and has an increase risk of colon cancer
|
juvenile polyposis - a polyposis syndrome, autosomal dominant inheritance
DO NOT confuse this with Juvenile polyps (hamartomatous polyps) which have not increased risk of carcinomas |
|
|
colon cancer with germline defect in DNA mismatch repair gene, results in replication errors positive phenotype, microsatellite instability and inc DNA mutation rate
|
hereditary nonpolyposis colon cancer
|
|
|
virus not associated with chronic carrier condition
|
HEV
|
|
|
Interferon (IFN) in combo with rebaverin can be used to treat which hepitits virus
|
HBV
|
|
|
acute hepatitis presents significant greate danger for pregnant women
|
HCV
|
|
|
pathology with the following sx?
-severe Malase -jaundice -enlarged liver -aminotransferase elevated 15x |
mononuclear inflitrates limited portal triad
|
|
|
collagen synthesis
macrovascular steatosis hypertrophy of ser cell swelling |
effects of alcohol on hepatocytes
|
|
|
cell death and mononuclear infiltrate focal and tend to center on portal triad, occuring near the limiting plate (piecemeal necrosis)
|
chronic hepitits
|
|
|
associated with "foamy degeneration": accumulation of cholestrol and other lipids in some hepatocytes adn sinusoidal cells gives a bubbly or foamy apprearence
|
hepatocellular injury in cholestasis
|
|
|
where is conjugated bilirubin normally secreted
|
bilirubin is normally secreted into the space of Disse
|
|
|
associated with portal granulomas (granulomatous bile duct destruction)
|
primary biliary cirrhosis
|
|
|
fibrosis in sinusoids close to central vein
|
alcoholic liver disease
|
|
|
regenerative nodules throughout the liver, alteration of hepatic architecture by fibrosis
|
cirrhosis
|
|
|
-pruritis, fatigue, jaudice
-elevated alk phos -liver biopsy reveals centrilobular bile canalicular pluging with normal triads -associated with UC |
primary sclerosing cholangitis
|
|
|
present as submucosal polyps
|
carcinoids
|
|
|
altered luminal phase absorption fxn
|
cystic fibrosis
|
|
|
frequent site of obstruction 2nd to intra-abdominal adhestion or hernia
|
jejunum / ileum
|
|
|
-crampy abdominal pain
-weight loss -bloody diarrhea |
UC
|
|
|
-abdominal pain often in LRQ
-bloody diarrhea -sometimes see gallstones or calcium oxalate kidney stones |
CD
|
|
|
IBD that does not involve the jejunum
|
UC
|
|
|
gut vascular disorder?
syndrome associated with wt loss, abdominal pain, diarrhea |
chronic intestinal ischemia
|
|
|
-seizure
-cerebral edema -renal failure what liver disease/ syndrome is associated with the above sx? |
acute hepatic failure
|
|
|
presents with bergan's traid of acute abdominal pain, spontaneous GI emptying, history of cardiac disease
|
mesenteric arterial emboli
SMA most common site for emboli |
|
|
due to low flow condition and may be managed medically
|
nonocculusive mesenteric ischemia
|
|
|
most pt lack predisposing condition, high rate of re-thrombosis
|
mesenteric venous thrombosis
|
|
|
sudden onset of abdominal pain, sugical findings inlcude necrosis of the small bowel and right and transverse colon
|
mesenteric arterial thrombosis
|
|
|
seen in association with low cardiac output states, heart failure and dialysis
|
nonocculusive mesenteric ischemia
|
|
|
most frequent site of obstruction due to volvulus
|
colon
|
|
|
a risk factor for severe acute hep A infection
|
hep C
|
|
|
complication of gastroparesis, a motor disturbance seen in DM pt
|
bezoar - concentrations of vegetable matter that build up in the stomach, often becoming symptomatic
|
|
|
NSAIDS, slow release potassium cholride tablets and doxycycline can all cause
|
intestinal ulcers
|
|
|
what gi disease is associated with renal failure
|
angiodysplasias
|
|
|
what gi condition is associated with dermatomyositis?
|
transfer dysphagia
-skeletal muscle diseases frequently give rise to significant chewing and swallowing problems |
|
|
best way to determine pancreatic necrosisas as a result of acute pancretitis
|
abdominal ct scan with IV contrast
|
|
|
steatorrhea
recurrent abdominal pain vit b12 deficiency DM |
chonic pancretitis
|
|
|
drug used for prophylaxis of ulcers to prevent complications of excessive NSAID use for inflammatory arthritis
|
misoprostol - a prostaglandin analogue
|
|
|
pseudomemebranous colitis is most closely associated with what?
|
antibiotic use
|
|
|
what conditions have a serum-ascites albumin gradient of less than 1.1 g/dl
|
cirrhosis
chf constrictive pericarditis hepatiac vein thrombosis |
|
|
what is used to improve portalsysttemic encephalopathy?
|
lactulose
neomycin laxatives antibiotics |
|
|
-hypoalbuminemia
-inc hepatic lymph prod and flow -renal Na retention -splanchnic and systemic arterail vasodilation -inc sinusoidal hydrostatic pressure |
formation of ascities in cirrhosis
|
|
|
-jaundice
-itching -caricoma of the head of the pancrease what necessary tx would this pt need |
intramuscular injection of vit k to correct patient ptt time
|
|
|
tonic contraction of rectosigmoidal area and absence of normal peristaltic contraction causing functional obstruction and dilation proximal to obstucted segment
|
hirschsprung disease - congenital defect in migration of ganglion cells of neural crest- dervived
|
|
|
A 45 year old male presents to the emergency room complaining of abdominal pain and lack of appetite. He has past medical history significant for diabetes mellitus, hypertension and gastroparesis. On EKG evaluation, he is noted to have prolonged QT interval which converts to a fatal arrhythmia. Which one of the following is linked to his current EKG findings?
a. Cisapride b. Erythromycin c. Domperidone d. Metoclopramide |
A 45 year old male presents to the emergency room complaining of abdominal pain and lack of appetite. He has past medical history significant for diabetes mellitus, hypertension and gastroparesis. On EKG evaluation, he is noted to have prolonged QT interval which converts to a fatal arrhythmia. Which one of the following is linked to his current EKG findings?
a. Cisapride - correct answer. the major reason this drug was pulled from the market was secondary to this fact. b. Erythromycin - incorrect. known to effect QT interval, should be monitored for prolongation c. Domperidone - incorrect. no known issues with prolonged QT interval or fatal arrhythmia d. Metoclopramide - incorrect. no known issues with prolonged QT interval or fatal arrhythmia |
|
|
Which one of the following is the best first line treatment option for mild to moderate colitis?
a. Surgical excision b. 5-ASA c. Azathioprine d. Metoclopramide |
Which one of the following is the best first line treatment option for mild to moderate colitis?
a. Surgical excision - incorrect. would be considered second-line unless the patient had severe toxic mega colon and/or fistula formation b. 5-ASA - correct answer; considered as first line therapy in mild to moderate colitis c. Azathioprine - incorrect. immunomodulators are only considered for maintenance therapy d. Metoclopramide - incorrect. not in the treatment algorithm for ulcerative colitis |

