![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
What is Anasarca
|
Severe generalized edema with widespread subcutaneous tissue swelling
|
|
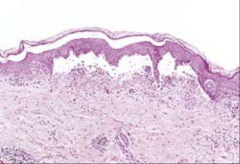
1. What here makes this classified as edema?
|
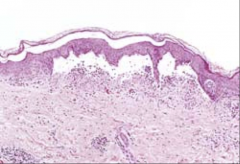
1. Microscopically manifests as subtle swelling with separation of the ECM
|
|
1. What are common etiologies of pitting edema?
|
1. CHF, Hypoproteinemia
|
|
1. What is the normal weight of both lungs together?
2. In this picture, what are the signs of pulmonary edema? 3. What are possible etiologies? |
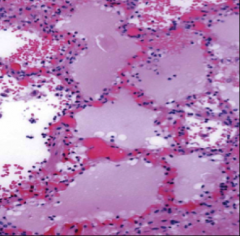
1. 750g
2. Frothy, blood-tinged mixture of air, edema fluid and RBCs 3. Left Ventricular Failure, ARDS, Bacterial infections, Hypersensitivity Reactions, Renal failure |
|
|
1. What is localized brain edema associated with?
2. What is generalized brain edema associated with? 3. Describe he morphology of brain edema |
1. Brain abscess and neoplasm
2. Encephalitis, hypertensive crises, obstruction to venous flow 3. Swollen gyri with narrowed sulci and flattened against the skull |
|
|
1. What is the difference between hyperemia and congestion?
2. Which organs are most effected by Congestion? 3. What is the difference between acute and chronic congestion? |
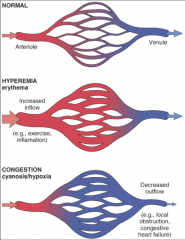
1. They both have increased blood volume, but:
Hyperemia - Active process w/ augmented blood inflow due to arteriolar dilation Congestion - Increased blood vol is passive and caused by impaired flow from tissue - TISSUES APPEAR CYANOTIC BECAUSE OF DECREASED OXYGENATION DUE TO THE CONGESTION 2. Lungs and Liver - venous-dependent organs 3. Acute - distended vessels and edema Chronic - Capillary rupture with hemorrhage, Hemosiderin, parenchymal cell atrophy and scarring, brown tissue |
|
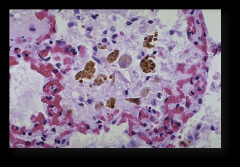
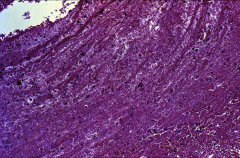
1. Is this acute or chronic congestion and why?
|
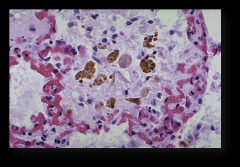
1. Chronic - Hemosiderin laden macrophages, fibrotic septa
|
|
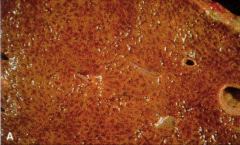
1. What is the etiology of nutmeg liver (Pictured - gross)?
2. Describe the morphology |
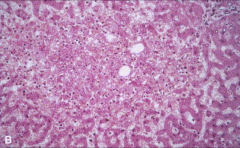
1. Right heart failure, hepatic vein or SVC obstruction
2. Central regions of hepatic lobules grossly red-brown and slightly depressed Centrilobular necrosis microscopically (Pictured) with hepatocyte drop out and hemorrhage and fibrosis |
|
|
1. What is the morphology of acute liver congestion?
|
1. Distention of ventral veins and sinusoids
May or may not have central hepatocyte necrosis |
|

1. What is the etiology of splenic congestion?
2. Describe the morphology |
1. Cirrhosis, splenic vein obstruction or portal vein obstruction, EHF
2. Splenomegaly with intact architecture |
|
|
1. Definition - Extravasation of blood into the extravascular space after vessel rupture due to initial hardening
|
1. Hemorrhage
|
|
|
Types of Hemorrhage. Sizes, causes, locations:
1. Hematoma 2. Petechiae 3. Purpura 4. Ecchymoses 5. Hemothorax, Hemopericardium, Hemarthrosis |
1. Large accumulation of blood from insignificant to massive
2. 1-2mm - Skin, mucous membranes, serosal surfaces. Due to increased intravasc pressure, low platelets, or platelet defects 3. >/= 3mm - associated w/ trauma, vasculitis, increased vascular fragility. Same places as petechiae 4. >1-2cm - Common bruises from trauma 5. Large accumulations of blood in the body cavities |
|

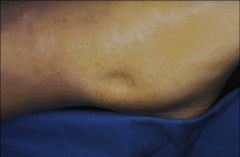
1. What type of hemorrhage is pictured here and what size do we normally see it in?
2. What makes the blue-green color of this bruise? 3. What makes a bruise yellow/brown? |
1. Ecchymosis - >1-2cm
2. Enzymatic conversion of Hemoglobin (Red) into Bilirubin 3. Hemosiderin |
|

1. What type of hemorrhage is pictured here and what size do we normally see it in?
2. What populations do we see this in? 3. Where can this cause bleeding, easily? |
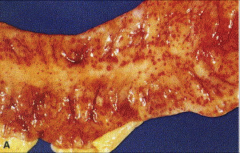
1. Petechiae - 1-2mm
2. People with platelet disorders 3. Throughout the GI tract |
|

1. What is this?
2. What causes it? |
1. Hemoperitoneum
2. Rupture from trauma |
|
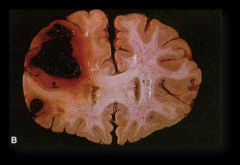
1. What percentage of blood volume loss is necessary to cause Hemorrhagic (hypovolemic) shock?
2. Why is this bleed so important in the brain, but wouldn't be important subcutaneously? |
1. 20%
2. The location of the bleed matters because the skull is unyielding and you get increased pressure and herniation of the brain stem |
|
|
1. What are the 3 components that Hemostasis and thrombosis depend on?
|
1. Vascular Endothelium
2. Platelets 3. Coagulation Cascade |
|
|
1. What causes the brief vasoconstriction that appears after vascular injury?
2. What happens shortly after? |
1. Endothelin - potent endothelium-derived vasocontrictor
2. The platelet and coagulation response causes vasodilation (Normal Hemostasis) |
|
|
1. What causes activation of platelets?
2. What happens to the platelets once they are activated? 3. What is contained in the Alpha Granules of platelets? 4. What is contained in the Dense bodies (Delta Granules) of platelets? |
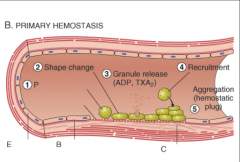
1. Exposure to ECM protein constituents such as:
Collagen, Proteoglycans, Fibronecin, Adhesion glycoproteins (VON WILLEBRAND FACTOR) 2. Adhesion and shape change, Secretion of granular contents, and Aggregation (Aka PRIMARY HEMOSTASIS), surface expression of phospholipid complex to Ca++ and coagulation factor binding 3. Alpha Granules - P-selectin, Coagulation and growth factors 4. Dense Bodies - ATP, ADP, Ca2+, vasoactive amines (Histamine and Serotonin) |
|
|
1. What is Bernard-Soulier Syndrome?
2. What is von Willebrand Disease? |
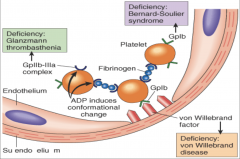
1. Problems with Glycoprotein 1b (pictured) - Patients extravasate fluid into the extracellular space
2. Problems with vWF (pictured) Patients extravasate fluid into the extracellular space |
|
|
1. What is the difference between an Primary and Secondary hemostatic plug?
|
1. Primary - reversible. undergoes fibrosis and is removed
Secondary - irreversible, fused mass of fibrin and platelets |
|
|
1. What are two other names for tissue factor?
2. What is tissue factor and what makes it? 3. What is its function? |
1. Factor III and Thromboplastin
2. Membrane bound procoagulant protein synthesized by endothelial cells 3. Initiation of the coagulation cascade --> Thrombin generation |
|
|
1. What causes platelet aggregation and what inhibits platelet aggregation from the Eicosanoids?
|
1. PGI2 Inhibits aggregation - I FOR INHIBIT - also VasoDILATED
TXA2 Activates aggregation - A FOR ACTIVATE - also vasoCONSTRICTS |
|

1. Recite the coagulation cascade
2. Which factors are in the Intrinsic? 3. Which factors are in the Extrinsic? 4. Which factors are in the Common? |
![2. 12, 11, 9, 8 [10, 2, 5]
3. 7, [10, 2, 5]
4. 10, 5, 2, 13, Fibrin](https://images.cram.com/images/upload-flashcards/867469/1766636_m.png)
2. 12, 11, 9, 8 [10, 2, 5]
3. 7, [10, 2, 5] 4. 10, 5, 2, 13, Fibrin |
|
|
1. How is the Prothrombin Time (PT) Tested and what does it test for?
2. How is the Partial Thromboplastin Time (PTT) Tested and what does it test for? |
1. Tests the function of the proteins in the extrinsic pathway Add Tissue Factor (3) and Phospholipids to Citrated plasma (Na+ Citrate chelates Ca++ and prevents spontaneous clotting)
Add exogenous Ca++ and time the clotting 2. Tests the function of the proteins in the intrinsic pathway: Add negatively charged particles (Ground Glass) to activate Factor 12 (Hagemon Factor), Phospholipids, and Ca++ Time how long it takes for fibrin to clot |
|
|
1. Why is a relatively small amount of thrombin so potent?
|
1. G-protein coupled receptor is clipped by thrombin
The resultant tethered peptide binds to another site on the receptor and activates the G-protein on the vascular endothelium, platelets, and smooth muscle |
|
|
1. How does Thrombin promote inflammation?
|
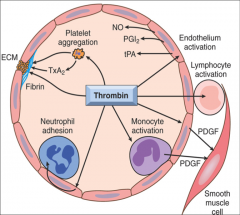
1. Mobilization of P-selectin
Production of chemokines and Cytokines Expression of endothelial adhesion molecules (CAMs) Induction of COX Pathway --> Production of Prostaglandins Production of PAF and NO Promotes leukocyte recruitment via changes in endothelial shape |
|
|
1. Why does interfering with clotting treat underlying inflammatory disease associated with Disseminated Bacterial Infections and Sepsis?
|
1. Inhibits coagulation, and therefore doesn't allow for inflammation to amplify in one spot. Instead, the factors leave the area and are filtered out
|
|
|
1. What does Non-injured tissue have to inhibit clotting?
|
1. Antithrombins
2. Endothelial Thrombomodulin 3. t-PA - Tissue Plasminogen Activator 4. Plasminogen Activator inhibitors |
|
|
1. What is the function of proteins C and S?
2. What activates them? |
1. Inactivate Factors Va and VIIIa
2. Endothelial Thrombomodulin causes Thrombin to activate them |
|
|
1. What is Virchow's Triad
|
1. 3 primary influences on Thrombus formation
Endothelial Injury - can cause thrombosis by itself Alteration in normal blood flow - non-laminar flow brings platelets to the endothelium and retard the inflow of clotting factor inhibitors Hypercoagulability - less of a contributor |
|
|
1. How to hyperviscosity syndromes (Polycythemia Vera) or deformed RBCs (Sickle Cell) result in small vessel stasis?
|
1. Alters the laminar flow and causes congestion
|
|
|
Hypercoagulability:
1. Factor V Gene Mutation - How does it work? 2. Inherited lack of anticoagulants - Which ones? |
1. 60% have recurrent thrombosis. Leiden mutation renders Factor V resistant to cleavage by activated C protein
2. Antithrombin III, Protein C, Protein S |
|
|
How can these lead to acquired Hypercoagulability?
1. Pregnancy 2. Aberrant Hepatic Synthesis 3. Cancers 4. Heparin induced thrombocytopenia syndrome 4. Antiphospholipid antibody syndrome |
1. Hyperestrogen
2. More coagulation factors made than Antithrombin III 3. Release of procoagulant tumor products 4. Administration of unfractionated heparin --> induces circulating Ab that cause platelet activation and endothelial injury 5. Patients with Abs against anionic phospholipids --> platelet activation Autoimmunity |
|
|
In which directions do thrombi extend?
1. Arterial 2. Venous 3. How does an Embolus happen? |
1. Arterial - Retrograde from the attachment point
2. Venous - Extend in the direction of blood flow 3. Propagation tail may not be well attached and can fragment into circulation |
|
|
1. What is the morphology of a thrombus from Cardiac or Arterial?
2. What is the morphology of a thrombus from Venous or Phlebothrombosis 3. Where are venous thrombi most likely to be found? |
1. Gray-red with Lines of Zahn (microscopic laminations)
2. Long red-blue cast of the vein lumen Contains more enmeshed RBCs with sparse fibrin strands (RED or STASIS Thrombi) 3. Lower extremity (90%) |
|
1. What are Lines of Zahn?
2. Where are they most likely to be found? |
1. Microscopic laminations with Pale layers of platelets and fibrin alternating with darker red and cell-rich layers
2. Left Ventricle overlying an old infarct Ruptured atherosclerotic plaques Aneurysmal sacs |
|

1. What is Libman-Sacks Endocarditis?
2. What other kinds of endocarditis can you have? Picture - What kind of disease is it: 3. Left 4. Left Middle 5. Right Middle 6. Right |

1. Patients with SLE get this because of circulating immune complexes causing inflammation of the heart valves
2. Bacterial (infective) and Non-bacterial thrombotic (vegetative) 3. Rheumatic Heart Dz - small vegetations along lines of closure 4. Infective Endocarditis - Bulky, large vegetations that cause extensive valve damage 5. Non-bacterial - small vegetations on line of closure 6. Libman-Sacks - underneath surface of the valve |
|
|
1. What can the outcome of a thrombus be?
2. Where is the most common place to lodge a thromboembolism? 3. What is a paradoxical embolism? |
1. Dissolution by fibrinolytic activity
Organization and Recanalization - Firbosis and Incorporation of the thrombus into the endothelial wall Embolization 2. Main Pulmonary Artery, or Across the saddle (Saddle Embolus) 3. Emboli pass through atrial or ventricular defects into the systemic circulation (Completely Skip the Lungs) |
|
|
Clinical Significance of Thrombi
1. Superficial - Varicose Saphenous Veins 2. Deep - Large veins, typically above the knee 3. How many cases of DVT are symptomatic? |
1. Local congestion and pain - Rarely embolize
Local edema and impaired venous drainage --> Predisposition to skin infection and varicose ulcers 2. Embolize more easily (into the lung) - Venous obstruction offset by collateral flow 3. 50% |
|
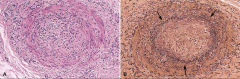
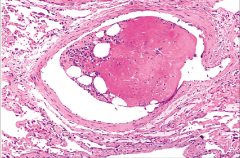
1. What is indicated by the black arrows on these thrombi that have reorganized?
2. Why are there no lines of Zahn? |
1. Intact internal and external elastic laminae
2. There is granulation tissue and fibrosis, which means that the thrombus is no longer present, but has been removed. |
|
1. What is DIC (Disseminated Intravascular Coagulation)?
2. What causes it? 3. What is the mechanism and why is it so dangerous? 4. How does this lead to shock? |
1. Widespread FIBRIN THROMBI ONLY in the microcirculation
2. NOT A PRIMARY DISEASE - It is a complication of any diffuse activation of thrombin 3. Concurrent consumption of coagulation factors and activation of fibrinolysis --> Results in serious bleeding (Hemorrhagic Diathesis) 4. Thrombosis leads to Microinfarction of tissue Hemorrhage leads to Shock |
|
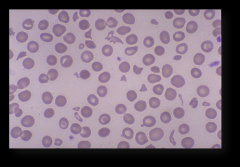
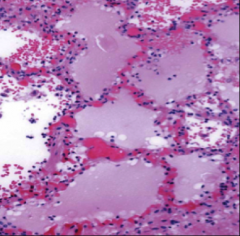
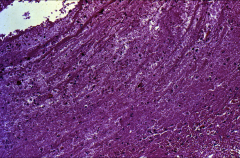
1. What is pictured here?
2. What condition is it associated with? |
1. Blood smear with Schistocytes
2. DIC - Disseminated Intravascular Coagulation |
|

1. What is this?
|
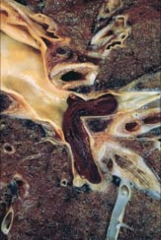
1. Embolus
|
|
|
1. What is a systemic Thromboembolism?
2. Where do they come from? 3. How can we assess the extend of damage that one will get from an embolus? |
1. Embolus in the arterial circulation
2. 80% - Intracardiac mural thrombi 60% Secondary to MI 25% from within dilated left atria (secondary to rheumatic fever valve injury) If arteriolar - 75% from lower extremities 3. Collateral circulation dictates how bad the injury will be |
|
|
1. What is the presentation of a fat embolus?
|
1. Sudden pulmonary insufficiency (1-3 days post injury)
20-50 y/o Diffuse petechial rash Neurologic symptoms --> Irritability and restlessness to Coma Thrombocytopenia and anemia may occur |
|
|
1. What is the pathogenesis of a fat embolism?
2. How is it diagnosed? 3. What are associated findings? |
1. Obstruction of vessel by microemboli of neutral fat
Local platelet and RBC aggregation Free Fatty Acid release Toxic injury, Platelet activation, Granulocyte recruitment 2. ID microvascular fat globules Frozen sections and special stains 3. Edema, Hemorrhage, Hyaline membranes in lungs |
|
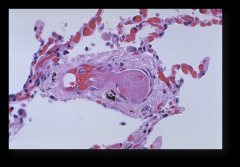
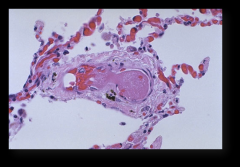
1. What is this?
|
1. Fatty Bone marrow embolus
|
|
|
1. What is an example of air embolism?
|
1. Decompression sickness - Depressurization allows dissolved gases to expand and bubble out of solution to form emboli
|
|
|
1. Definition - Area of ischemic necrosis usually caused by occlusion of the arterial supply
2. When in a vein, which organs are most at risk? 3. What factors influence the development of an Infarct? |
1. Infarct
2. Organs with a single venous flow: Ovary and Testes 3. Anatomic pattern of vascular supply, Rate of development of occlusion Vulnerability to hypoxia O2 content of blood |
|
|
Infarcts can be either Red (hemorrhagic) or White (anemic).
1. Where do red infarcts occur? 2. Where do white infarcts occur? |
1. Venous occlusion, loose tissues (lung), dual circulations (Lung, SI), Previously congested outflow
2. Solid organs - Heart, Spleen, Kidney - with end arterial circulations (few anastamoses) |

