![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
- 3rd side (hint)

|
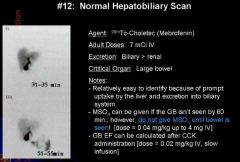
HIDA Scan: Normal
|
|
|
|
HIDA ISOTOPES:
|
99M TC DISOFENIN (DISIDA)
99M TC MEBROFENIN |
HIDA: dimethyl
o 85% excreted by the liver, 15% by the kidneys o Good visualization at bili levels of 5-7 mg/dl DISIDA: diisopropyl (Disofenin) o Approximately 88% hepatic excretion, 10% renal o Good visualization at bilirubin levels approaching 20 Disofenin: (Mebrofenin) o An analog of lidocaine [3] o m-3-bromo-trimethyl-IDA, has greatest resistance to displacement by bilirubin. Over 80% of the administered activity is cleared from the blood by liver hepatocytes within 10 minutes [5]. There is about 98% hepatic excretion of the agent [3]. The agent is excreted by the hepatocytes without metabolism or modification [5]. The agent is excreted into the bile by adenosine tri-phosphate dependent export pumps- the multidrug resistance associated proteins 1 and 2- without undergoing biotransformation during transit through the hepatocyte [4]. Excretion of the agent is not affected by elevated levels of serum bilirubin [5]. o T1/2 of uptake is about 6 minutes, and the T1/2 of excretion is about 14 minutes. |
|
|
Normal HIDA findings:
|
- Prompt clearance of blood pool
- rapid liver uptake, peaking in 15 min - bile ducts usually visible within 10-30 min - gb and small bowel visible within 1 hour. Activity in duodenum may mimic gb limited entero gastric reflux of tracer is a normal finding |
|
|
|
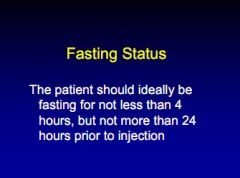
HIDA PRE-TREATMENT
|
|
|
|
|
HIDA DOSE:
|
2-8 mCi of disofenin or mebrofenin
|
|
|
|
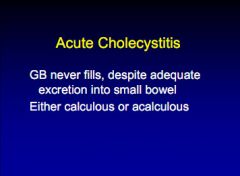
HIDA: What if GB not visible
|
Use morphine as delayed imaging alone not reliable
-- causes contraction at sphincter of oddi increasing pressure in the CBD Morphine-augmented scan provides more reliable results then simply delayed imaging alone. |
|
|
|
HIDA: how to give morphine
|
0.04 mg/kg (total 2-3mg) IV at 45-60 minutes if no GB tracer is in bowel and continue to image for up to an add 45 min. If still no GB then not likely to fill.
|
|
|
|
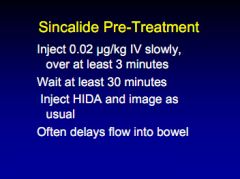
HIDA FASTING STATUS:
|
|
|
|

|
|
|
|
|
HIDA: rim sign
|
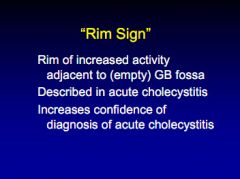
|
|
|
|
Causes of HIDA false positive
|
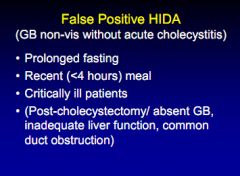
|
|
|
|
HIDA: causes of false neg
|
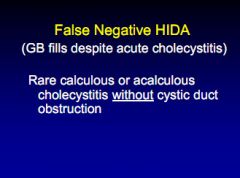
|
|
|
|
HIDA: reliability
|
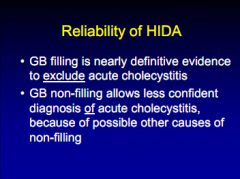
|
|
|
|
HIDA:biliary atresia
|
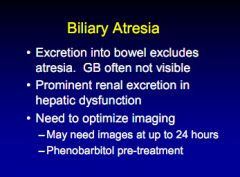
|
|
|
|
Gallbladder EF
|
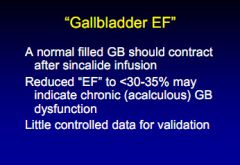
|
|
|

|
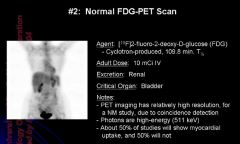
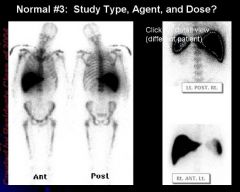
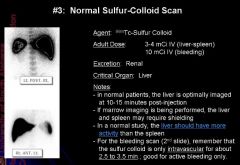
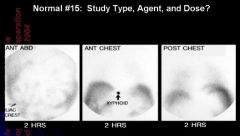
normal 99m tc sulfur colloid scan
|
Given IV at a dose of about 10 mCi
Critical organ is the Liver : USES: - hemangioma of the liver, gastric emptying, reflux, peritoneal scans, pulmonary aspiration, splenic remnant. - Filtered used for lymphoscintigraphy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
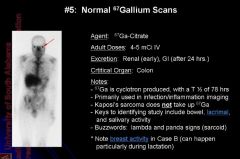
# decay: by electron capture to ground state of Zn-67
# energy levels(of diagnostic use): 92 KeV (38%); 184 KeV (23%); 300 KeV (16%) # physical half life: 3.3 days (78 hr) # biologic half life: 2-3 weeks |
|
|
|
|
|
Abdominal
|
Pertaining to the abdomen.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
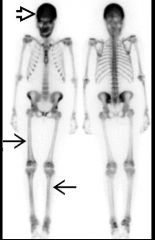
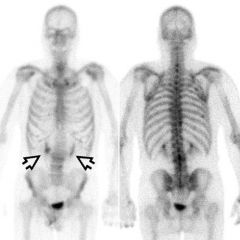
DDx superscan
|
common
Metastases, Diffuse Click to close this panel less common Renal Osteodystrophy Myelofibrosis Hyperparathyroidism (HPTH) Hyperthyroidism Mastocytosis Click to close this panel rare Aplastic Anemia Leukemia Lymphoma Osteopetrosis |
|
|
|
Hyperparathyroidism
|
Terminology
* Primary HPT * Secondary HPT (renal osteodystrophy) * Tertiary HPT Imaging Findings * Superscan: Absent renal, soft tissue activity; diffusely ↑ uptake in axial and appendicular skeleton (vs. axial predominance with metastatic disease) * Brown tumors: Increased activity in expansile bone lesion in patient with HPT * Soft tissue uptake on bone scan: Lung, stomach, kidneys, heart, pancreas due to soft tissue calcification Top Differential Diagnoses * Malignancy * Osteomalacia * Osteoporosis * Other Nonosseous Uptake on Bone Scan Clinical Issues * Usually asymptomatic: Suspect in patients with hypercalcemia on routine blood chemistry analysis * In outpatients, 1° HPT is most common cause of hypercalcemia * In inpatients, malignancy is most common cause of hypercalcemia (1° HPT is second) Diagnostic Checklist * Differential diagnosis for superscan, soft tissue uptake on bone scan includes HPT * Consider HPT in patient with sites of focal increased bone activity (brown tumors) and superscan |
|
|
Osteosarcoma
|
Terminology
* Primary malignant tumor of bone whose cells produce osteoid and have osteoblastic differentiation Imaging Findings * Radiograph, CT or MR: Heterogeneous metaphyseal mass * Tc-99m MDP bone scan: Increased activity in primary tumor, metastases (bone, lung) * Tl-201, MIBI, FDG PET: High grade tumors = intense activity around photopenic region (less obvious with lower grade tumor) * Ga-67: Increased activity in primary tumor, metastases; not helpful in following response to therapy * FDG PET/CT: Assess heterogeneous lesions for optimal biopsy site, whole body staging, evaluate response to therapy, restage Top Differential Diagnoses * Trauma * Infection * Paget Disease * Other Primary Bone Tumor * Benign Bone Lesions * Bone Metastases Clinical Issues * Pain localized to a palpable mass * 10-20% of patients have metastatic disease at presentation * Metastasis commonly involve lung and bone |
|

|
Stress Fracture
|
Terminology
* Stress fracture: Abnormal stress or overuse imposed on otherwise normal bone Imaging Findings * Typically positive on all 3 phases * Angiographic and blood pool phase positivity may become less conspicuous after 2-4 weeks * Delayed phase abnormality can persist for ≥ 6-12 months * Usually focal, fusiform or oval configuration of increased activity * Focal activity (e.g., < 1/5th length of tibia) * Whole body scan: Evaluate for other abnormalities, no additional radiation * SPECT recommended to increase sensitivity, especially when evaluating spine Top Differential Diagnoses * Shin Splints/Tibial Periostitis * Joint Derangement, Trauma, Avulsion * Neoplasm: Benign or Malignant Clinical Issues * Chronic skeletal pain with weight-bearing or repetitive use in absence of trauma * Symptoms may be vague and mimic other etiologies * Age: ↑ With age (↓ bone density) * Gender: M:F = 1:2 * Prognosis generally very good providing early recognition, appropriate therapy, compliance * Resolution may take 1-18 months or more |
|

|
Osseous Necrosis
|
Terminology
* Ischemic death of trabecular bone and marrow Imaging Findings * Best diagnostic clue: MR: T1 peripheral, geographic ↓ signal; T2 ↓ signal peripheral border, ↑ signal inner border * Morphology: Humeral/femoral head: Linear/wedge-shaped photopenia * Bone scan 80-85% sensitive with use of SPECT * May see involvement of multiple joints in patients with underlying disease (e.g., sickle cell disease) Top Differential Diagnoses * Fracture * Transient Osteoporosis * Infection * Bone Tumor * Bursitis * Osteoarthritis Clinical Issues * Pain, initially with sudden onset * Warmth, tenderness, erythema sometimes seen with acute infarct * Male > female (up to 8x in most locations) * Spontaneous osteonecrosis knee: Elderly females * Symptomatic disease may lead to structural failure and severe secondary arthritis * Asymptomatic disease may resolve * AVN of hip: Increased risk of involvement of opposite hip Nuclear Medicine Findings * Bone scan o Bone scan 80-85% sensitive with use of SPECT o Vascular phase + Photopenic defect + May have donut sign due to surrounding hyperemia, adjacent synovitis + SPECT imaging helpful in unmasking hyperemia from avascular area o Reparative phase + Photopenia diminishes + Increased activity due to osteoblastic response o May see involvement of multiple joints in patients with underlying disease (e.g., sickle cell disease) * Tc-99m sulfur colloid o Defines distribution of viable red bone marrow ("marrow map"), reticuloendothelial system o Symptomatic sites of AVN: Decreased activity immediately after vaso-occlusive event o Asymptomatic sites of AVN: Decreased activity in area of old bone infarct o Useful in identifying patients with expanded marrow, such as sickle cell patients o Limitations of use of Tc-99m sulfur colloid in AVN + Developmental regression of red marrow in extremeties (distal to proximal): Adult pattern is axial and proximal appendicular + Elderly: May lose red marrow signal in proximal femurs, humeri; may be asymmetrical + Loss of red marrow signal with infection, trauma o Dose: 8-10 mCi (296-370 MBq), image 20-30 min post injection # Dose: Tc-99m MDP bone scan * Pediatrics: (Age + 1/Age + 7) x adult dose * Adult: 20-30 mCi (740 MBq-1.11 GBq) * Inject away from site of interest |
|
|
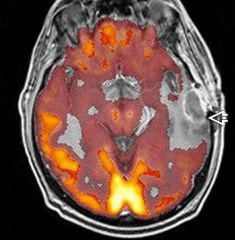
Radiation Necrosis vs. Recurrent Tumor
|
Terminology
* Includes edema, arteritis, leukoencephalopathy, mineralizing microangiopathy, necrotizing leukoencephalopathy, posterior reversible encephalopathy syndrome (PRES), radiation injury, radiation-induced tumors Imaging Findings * Multivoxel MRS: Characteristic patterns in recurrent tumor, radiation necrosis * FDG PET: Tendency for increased metabolism in recurrent tumor, low in radiation necrosis * However, FDG PET currently not typically reimbursed for radiation necrosis vs. recurrent brain tumor Top Differential Diagnoses * Abscess * Multiple Sclerosis * Vascular Dementia * Progressive Multifocal Leukoencephalopathy Pathology * XRT: Spectrum from edema to cavitating WM necrosis; demyelination; coagulation necrosis: Favors WM Diagnostic Checklist * Distinguishing residual/recurrent neoplasm from XRT necrosis difficult using morphology alone * MRS, FDG PET, Tl-201 or Tc-99m sestamibi SPECT all options for recurrent tumor from radiation necrosis |
|
|
Skeletal Muscle Disorders
|
Imaging Findings
* Best diagnostic clue: Focal ↑ muscle uptake on bone scan indicates muscle injury * Symmetrically "hot" renal cortex on bone scan often associated with muscle injury (renal myoglobin deposition) * Bone scan uptake in specific muscles may occur within a week of strenuous exercise * Compartment syndrome: Higher risk if ↑ muscle uptake on bone scan following trauma or infection * Increased uptake on bone scan in involved muscle groups: Correlates with muscle weakness * Focal uptake of FDG in muscle groups: Exercise, inflammation, metastases * Diffuse FDG uptake in all skeletal muscle: Metabolic causes * Bone scan: Very sensitive for muscle injury, actively forming myositis ossificans * C+ MR: Best modality for necrotizing fasciitis * To assess muscle injury: Tc-99m pyrophosphate bone scan preferred over diphosphonate Top Differential Diagnoses * Hypermetabolic Brown Adipose Tissue (HBAT) * Musculoskeletal Tumors * Tumoral Calcinosis Diagnostic Checklist * Bone scan: Increased uptake in skeletal muscle = muscle injury * FDG PET: Patterns of both generalized and focal muscle uptake less specific for muscle injury |
|
|

Paget Disease
|
Terminology
* Paget disease (PD) of bone; osteitis deformans; osteoporosis circumscripta (skull) * Disorder of abnormal/excessive bone remodeling characterized by coarse trabeculae, sclerosis, and expansion of one or more bones * Although thickened, abnormal bone weaker and bone deformity or fracture common Top Differential Diagnoses * Bone Metastases * Primary Bone Tumor * Fibrous Dysplasia (FD) Clinical Issues * Asymptomatic ~ 90% * Painful extremities, bowing long bones, secondary osteoarthritis * ↑ Serum alkaline phosphatase, ↑ urinary and serum hydroxyproline * Malignant degeneration rare (generally < 1%) Diagnostic Checklist * Bone scan most sensitive test to detect PD * Whole body bone scan: Diagnose, assess extent of PD * Focal increased activity over background of affected bone: Consider fracture, malignant degeneration * Bone metastases vs. PD can be difficult differential diagnosis * New sites in patient with long-standing PD suggest metastatic disease * Radiographic, MR, biopsy correlation may be necessary to distinguish PD from metastases |
|

|
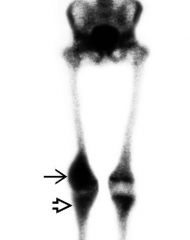
Hypertrophic Osteoarthropathy
|
Imaging Findings
* Best diagnostic clue: Tc-99m (diphosphonate) bone scan shows symmetric ↑ activity of diaphyseal, metaphyseal surfaces of long bones * Distal femur, tibia/fibula and radius/ulna most common * Skeletal scintigraphy for evaluation and surveillance * Linear increased tracer accumulation = periosteal reaction Top Differential Diagnoses * Skeletal Metastases * Thyroid Acropachy * Paget Disease * Venous Insufficiency * Hypervitaminosis A * Infantile Cortical Hyperostosis * Camurati-Engelmann Disease * Stress Fracture Pathology * Primary HOA: Autosomal dominant * Secondary HOA: No significant genetic correlation * Epidemiology: Secondary HOA accounts for ≥ 95% of HOA * Pulmonary disease associated with secondary HOA: Classically bronchogenic carcinoma or pulmonary metastases Diagnostic Checklist * Tc-99m MDP bone scan to evaluate therapy response * Consider secondary HOA in patients undergoing bone scintigraphy for malignancy staging workup |
|
|
Obstructive Uropathy
|
Imaging Findings
* Degree of obstruction inferred by renal + collecting system washout curves: O'Reilly classification * Type-I curve (normal): Spontaneous washout of activity from collecting system prior to Lasix (furosemide) administration (washout T 1/2 < 10 minutes) * Type II curve (high grade obstruction): Progressive rise in activity in collecting system, even after Lasix * Type IIIa curve (dilated, non-obstructed): Activity continues to rise until Lasix given, then washes out normally (washout T 1/2 ≤ 10 min) * Type IIIb curve (partial obstruction): Activity continues to rise until Lasix; thereafter decreases but washout T 1/2 > 10 min * Acute obstruction: IVP or NECT * Chronic obstruction: Tc-99m MAG-3 renography with Lasix * Postural drainage maneuver: Greatly reduces number of false positive or indeterminate Lasix renograms * Rationale: Many causes of false positive or indeterminate scans show normal emptying in upright position Top Differential Diagnoses * Dilated, Non-Obstructed Collecting System * Renal Vein Thrombosis * Renal Artery Stenosis * Acute Tubular Necrosis * Vesicoureteral Reflux * Medical Renal Disease * Multicystic Dysplastic Kidney |
|

|
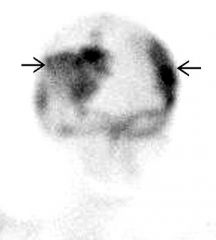
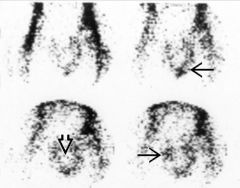
reflex sympathetic dystrophy
Complex Regional Pain Syndrome Nuclear Medicine Findings * Three-phase bone scan: "Classic" findings o Angiographic phase: Hyperemia in affected limb o Blood pool phase: Increased periarticular activity when compared with unaffected limb o Delayed phase: Increased periarticular activity in affected limb; abnormal activity increases distally * Stage 1: Usually normal bone scan * Stage 2: Hyperemia on angiographic phase, increased periarticular activity on blood pool and delayed phase o Decreased blood flow can be seen, suggests vasospasm, more common in children * Stage 3: Hyperemia on angiographic phase, increased periarticular activity on blood pool and delayed phase |
Terminology
* Complex regional pain syndrome (CRPS) * Painful disorder of extremities * Usually due to injury, surgery, vascular event * Usually unilateral; bilateral in ~ 25% * Stage 1: Extremity pain characterized by aching, throbbing, burning, cold/touch intolerance, swelling * Stage 2: Muscle wasting, ↑ soft tissue edema, brawny skin, ↑ pain, vasomotor abnormalities * Stage 3: ↓ Range of motion, digit/joint contracture, waxy skin, brittle, ridged nails, vasomotor abnormalities, ↓ pain Imaging Findings * Tc-99m MDP bone scan: Classically, increased periarticular activity in affected limb on delayed images * Periarticular activity increases distally Clinical Issues * Burning, stinging pain * Vasomotor instability * Hyperesthesia * Skin changes (thickened, waxy), hair loss Diagnostic Checklist * Bone scan to look for signs of "classic" CRPS findings * High intensity uptake on bone scan suggests better prognosis, positive response to therapy * Early bone scan in patient with suspected CRPS to effect early therapy if positive * Palmar and plantar delayed planar images to best display periarticular activity |
|
|
Gallium diffuse lung uptake ddx:
|
sarcoid
PCP Lymphoma |
|
|
|
Gallium nodular uptake
|
lymphoma
sarcoid |
|
|
|
Gallium parotid uptake increased in
|
Sarcoid
Sjogren's Radiation |
|
|
|
Normal Pressure Hydrocephalus
|
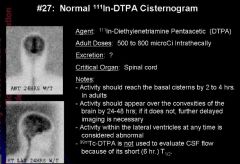
Terminology
* Normal pressure hydrocephalus (NPH) * Radionuclide cisternography (RNC) Imaging Findings * Prominent ventricular activity at 24 h on In-111 DTPA cisternography is best indicator of NPH * "Flow void" in aqueduct on MR indicates NPH (vs. high obstructive hydrocephalus) * NHP: 50% correlation with improvement after shunt * Normal immediate RNC images: Rapidly ascent to head * Normal 1-2 h RNC images: Ascends to basal cisterns * Normal 4-6 h RNC images: Reaches Sylvian & suprasellar cisterns, ventricular penetration * Normal 24 h RNC images: No ventricular activity on planar images (may be faint on SPECT); flow over convexities to top of head * Normal 48 h RNC images: Homogeneous distribution of tracer around brain * NPH: Prominent ventricular activity at 24 h and beyond * NPH: Flow to top of head may be normal or slow Clinical Issues * Heterogeneous triad (10% of NPH): Dementia, gait apraxia, urinary incontinence Diagnostic Checklist * Whether ventricular dilation is solely due to atrophy * Prominent ventricular activity at 24 h is single diagnostic feature of NPH on RNC |
|
|

|
Terminology
* Cerebrospinal fluid (CSF) rhinorrhea, CSF otorrhea, CSF fistula, pseudomeningocele * Spontaneous, iatrogenic or post traumatic escape of CSF from the normal CSF space Imaging Findings * Best diagnostic clue: Visualization of CSF outside of its expected location * Location: Nose, nasopharynx, paranasal sinuses, temporal bone or ear, along spinal canal * Activity seen outside the expected location of CSF * Activity in nose or ear packs significantly higher than level in a concurrent blood sample * Nose or ear pack counts are much more sensitive than imaging * Pack counts are considered positive if more than double blood counts, but in positive studies are often several orders of magnitude hotter than blood * CSF is labeled with In-111 DTPA about 500 microcuries by intrathecal injection (2-5 mCi Tc-99m DTPA for overpressure technique) * Tracer injection must be done carefully to avoid leakage of tracer out of injection site * Mixing tracer with metrizamide prior to injection will cause metrizamide to act as transport vehicle, bringing tracer to potential leak site sooner for intracranial level leaks and facilitating combined nuclear and CT imaging * Packs should not be removed if possible until tracer is seen on images bathing area of clinical concern |
|
|
|

Terminology
* Spontaneous or traumatic twisting of testis & spermatic cord within scrotum, resulting in vascular occlusion/infarction * Results from inadequate fixation of testis to tunica vaginalis through gubernaculum testis (bell-clapper deformity) ⇒ testis torsing on spermatic cord Imaging Findings * Tc-99m pertechnetate testicular scan: Sensitivity 80-90% * During first 1-2 hours, flow may be normal * Blood flow: Absent flow via spermatic cord * Static image: Photopenia in affected testicle when compared with normal testicle * Blood flow: Increased (hyperemia) with testicular infarction * Static image: Halo sign = testicular infarction Top Differential Diagnoses * Epididymo-Orchitis * Testicular Abscess * Hydrocele * Varicocele * Inguinal Hernia * Neoplasm * Trauma Clinical Issues * Clinical profile: Male child with acute scrotal pain * Surgical emergency: Testicular infarction if torsion not treated promptly * Spontaneous detorsion in 7% |
|
|
|
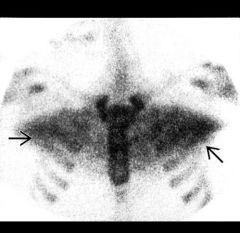
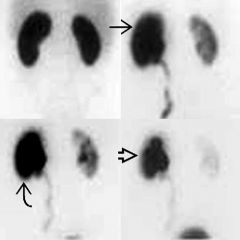
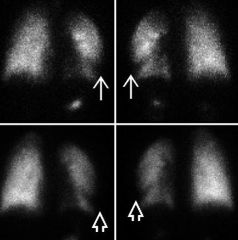
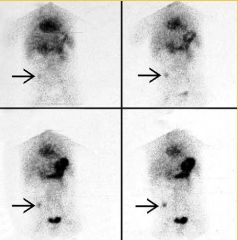
Anterior and posterior Tc-99m aerosol ventilation shows peripheral ventilation defect (white arrow) in left lung (upper panels). Perfusion images show matching moderate defect (white open) in left lung (lower panels). Same patient as next image.
Imaging Findings * Location: Lower lobes > upper lobes * V/Q detects > 95% of emboli which completely occlude pulmonary arterioles > 2 mm * Most patients with acute PE have radiographically normal chest * Chest X-ray (CXR): To exclude clinical mimics of PE; adjunct to interpretation of V/Q scan * CTA: Usually first-line PE examination in clinical practice today * CTA: 83% sensitivity; 96% specificity for PE * High probability: ≥ 80% likelihood of acute PE * High probability: At least 2 large (or arithmetic equivalent) mismatched segmental perfusion defects * Intermediate probability: 20-79% chance of acute PE * Intermediate probability: At least 1 moderate, but less than 2 large (or arithmetic equivalent), mismatched segmental perfusion defects * Intermediate probability: Matching VQ defects with corresponding focal chest x ray opacity, or moderate to large VQ mismatches (with clear chest) that do not meet size or number criteria for high probability * Intermediate probability: Patterns difficult to categorize as either low or high probability * Low probability: ≤ 20% likelihood of acute PE * Low probability: Matched VQ defects with clear chest * Low probability: Small perfusion defects * Low probability: Nonsegmental perfusion defects (cardiomegaly, enlarged vasculature, overlying structures): Likely normal perfusion |
|
|
|
VQ mismatch DDX:
|
PE
vasulitis radiation therapy, wegener's, autoimune Tumor compression of PA Pleaural effusion Radiation Therapy Hypoplastic PA |
|
|
|
Restrictive lung disorders
|
-the needed elastic work to expand the lung increases requiring respiratory muscles to generate more force than normal.
- more elastic work is required to inflate the lung |
|
|
|
Difference between cellulitis, osteo, fracture and tumor on 3 phase:
|
Cellulitis is hot on flow and bp and cold on delayed
osteo and fractre both hot on all three oninflammatory will show on delayed +- flow. |
|
|
|
Dif for positive 3 phase:
|
osteo
trauma hypervascular tumor RDS neuropathic joint |
|
|
|
Acute renal failure on nucs
|
Terminology
* Causes: Prerenal (perfusion), intrinsic renal, postrenal (obstructive) Imaging Findings * Tc-99m DTPA: Glomerular filtration, < clearance than tubular agents; used to calculate GFR * Tc-99m MAG3: Tubular secretion; better images than Tc-99m DTPA; estimate ERPF * Prerenal failure: Heart failure, hypovolemia, hypotension, dehydration * Most intrinsic renal diseases: Non-specific decreased flow/function on renal scan * Mild-moderate ATN: Blood flow relatively normal, rising (delayed) nephrogram phase * Severe ATN, frank cortical necrosis: Poor blood flow; decreased or absent cortical uptake * Pyelonephritis: Patchy striated scintigraphic nephrogram, poor clearance * Catastrophic vascular occlusion: Lack of flow/function to involved kidney * Renal vein thrombosis: Asymmetrically enlarged "hot" kidney; may mimic obstruction * Over time, radiotracer & cortical uptake falls * Acute complete obstruction: May not visualize collecting system * Bladder outlet obstruction: Often non-specific ↓ flow, function Top Differential Diagnoses * Urine Leak * Chronic Renal Failure |
|
|
|
Polycystic kidney disease on nucs
|
Nuclear Medicine Findings
* Technetium-99m (Tc99m) mercaptoacetylinetriglycerine (MAG3) o Multiple photopenic masses o Delayed clearance of radionuclide + Obstruction of collecting system due to cysts + Decreased renal function * Indium-111 labeled WBC scan o Detects infected renal cysts o Increased tracer uptake, markedly at cyst periphery |
|
|
|
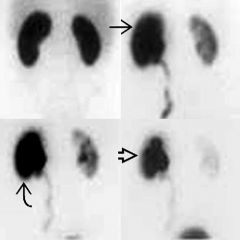
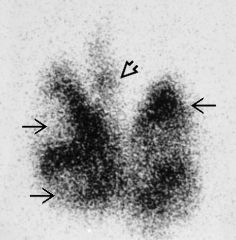
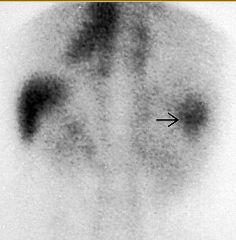
Bone scan shows abnormal orientation of the renal collecting systems and approximation of the lower poles (black open). This can be the only clue to horseshoe kidney when the isthmus is not seen.
Terminology * Horseshoe kidney, crossed (with or without fusion) ectopia, simple renal ectopia, thoracic kidney * Normal renal tissue outside of the expected location in the retroperitoneum * Often asymptomatic with diagnosis being incidental Imaging Findings * Best diagnostic clue: Normal kidney seen outside of the expected location and/or abnormally oriented on any imaging modality * Frequently an incidental finding on bone scan or renal imaging * Abnormally located or oriented functional renal parenchyma Pathology * > 50% of ectopic kidneys have a hydronephrotic collecting system * Vesicoureteral reflux incidence reported to be as high as 70% and varies with type of ectopy * Blood supply can be anomalous for all types of renal ectopy Clinical Issues * Most are incidental findings at autopsy, on routine perinatal screenings, or on other diagnostic imaging Diagnostic Checklist * Horseshoe kidneys may be subtle if isthmus is fibrous * Ectopic renal tissue overlying an osseous structure on a bone scan may mimic a bone lesion |
|
|
|
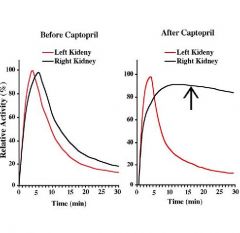
Renovascular Hypertension
Terminology * Renin-angiotensin system increases renal blood flow when renal hypoperfusion detected * ↑ Blood pressure maintains renal perfusion and glomerular filtration rate (GFR) * Angiotensin-converting enzyme inhibitor (ACE-I) drugs prevent formation of angiotensin II causing renal function to fall in patients with RVHT * ACE-I antihypertensive medications (e.g., captopril & enalapril) are used to identify RVHT on renogram Imaging Findings * Best diagnostic clue: ACE-I renogram showing functional deterioration after ACE-I administration when compared to baseline renogram * ACE-I renogram: Excellent detection of clinically significant RAS; sens > 90% & spec 95% in those with good renal function * Renogram using Tc-99m DTPA: Shows an overall decrease in uptake and function of kidney with RAS after ACE-I * Renogram using Tc-99m MAG3: Shows significant cortical retention of radiotracer in kidney with RAS after ACE-I Diagnostic Checklist * 2-day protocol: If ACE-I renogram performed first is normal, no need to perform baseline renogram = no RVHT * Protocol pitfalls: Poor absorption of ACE-I, dehydration, hypotension, effects of full bladder |
|
|
|
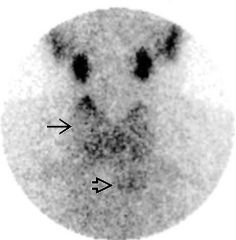
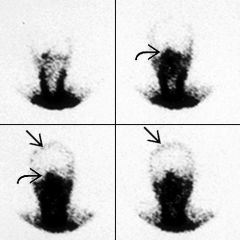
Anterior thyroid scan shows thyroid enlargement and bilateral nodules (black arrow) in a patient with multinodular goiter. Note pyramidal lobe also evident (black open).
Multinodular Goiter Terminology * Adenomatous thyroid hyperplasia ⇒ nodules in enlarged thyroid * Many nodules become autonomous * Some nodules become toxic ⇒ toxic nodular goiter Imaging Findings * Heterogeneous radiotracer uptake with irregular, nodular thyroid contour * Discrete nodules may be hot (increased activity), cold (photopenic), warm, or isointense/not visualized * Most nodules cold Top Differential Diagnoses * Graves Disease * Hashitoxicosis * Toxic or Autonomous Nodule * Post-Viral Subacute Thyroiditis * Cancer * Riedel Thyroiditis Clinical Issues * Rx dose: Typically 20-25 mCi (740-925 MBq) I-131 * Requires weeks to months to become fully effective * Multiple doses may be required * Subtotal or total thyroidectomy recommended for very large, compressive goiter Diagnostic Checklist * Elderly: MNG + subclinical hyperthyroidism common * Radioactive iodine treatment for symptomatic (cardiac) relief |
|
|

|
Anterior thyroid scan shows large hot nodule (black arrow) in right thyroid lobe. Note little uptake in normal thyroid tissue (black open) as thyroid hormone released by toxic nodule suppresses TSH, inhibiting radiotracer uptake.
Thyroid Adenoma, Hyperfunctioning Terminology * Plummer disease: Solitary toxic nodule or toxic multinodular goiter (MNG) * Follicular adenomas: Neoplasms arising from epithelial cells; usually well-encapsulated, benign, autonomous * Thyrotoxicosis results from hyperfunctioning nodule releasing thyroid hormone Imaging Findings * I-123 or Tc-99m pertechnetate scan: Single, usually large hot nodule; minimal or no activity in remaining thyroid * Overall cancer risk in hot nodule < 4% (< 1% in hyperthyroid patient with toxic hot nodule) Top Differential Diagnoses * Toxic Multinodular Goiter * Graves Disease * Hashimoto Thyroiditis * Unilobar Thyroid Agenesis * Thyroid Cancer * Subacute Thyroiditis Clinical Issues * Medical therapy: Thyroid-blocking propylthiouracil (PTU) or methimazole * Often used to achieve protective euthyroid state before radioiodine ablation, thyroidectomy * Radioiodine ablation: 25-30 mCi (925-1110 MBq) I-131 usually effective * Surgical treatment: Lobectomy or nodule excision |
|
|
|
|
Anterior thyroid scan shows Hashimoto thyroiditis (black arrow) with substernal goiter (black open).
Terminology * Chronic thyroiditis, chronic lymphocytic thyroiditis * Part of spectrum of autoimmune thyroid diseases * Cellular and humoral-mediated thyroid destruction Imaging Findings * Tc-99m pertechnetate or I-123 scan: Pattern highly variable * I-123 or I-131 uptake: Variable, depending on stage Top Differential Diagnoses * Diffuse Nontoxic or Endemic Goiter * Riedel Struma: Fibrous Invasive Thyroiditis * Multinodular Goiter * Invasive/Infiltrative Disease * Recovering Subacute Thyroiditis * Medication Effects Pathology * US: Most common cause of hypothyroidism * Worldwide: 2nd leading cause of hypothyroidism (iodine deficiency = 1st) Clinical Issues * Hypothyroidism * Goiter * Other signs/symptoms: Hyperthyroidism or Hashitoxicosis (rare) Diagnostic Checklist * Radioactive iodine uptake: Increased, normal or decreased * Hashimoto thyroiditis on scan: May mimic Graves, multinodular goiter, nontoxic goiter, or other autoimmune thyroiditis |
|
|
|
|
Anterior thyroid scan shows Hashimoto thyroiditis (black arrow) with substernal goiter (black open).
Terminology * Chronic thyroiditis, chronic lymphocytic thyroiditis * Part of spectrum of autoimmune thyroid diseases * Cellular and humoral-mediated thyroid destruction Imaging Findings * Tc-99m pertechnetate or I-123 scan: Pattern highly variable * I-123 or I-131 uptake: Variable, depending on stage Top Differential Diagnoses * Diffuse Nontoxic or Endemic Goiter * Riedel Struma: Fibrous Invasive Thyroiditis * Multinodular Goiter * Invasive/Infiltrative Disease * Recovering Subacute Thyroiditis * Medication Effects Pathology * US: Most common cause of hypothyroidism * Worldwide: 2nd leading cause of hypothyroidism (iodine deficiency = 1st) Clinical Issues * Hypothyroidism * Goiter * Other signs/symptoms: Hyperthyroidism or Hashitoxicosis (rare) Diagnostic Checklist * Radioactive iodine uptake: Increased, normal or decreased * Hashimoto thyroiditis on scan: May mimic Graves, multinodular goiter, nontoxic goiter, or other autoimmune thyroiditis |
|
|
|
|
Anterior thyroid scan shows Hashimoto thyroiditis (black arrow) with substernal goiter (black open).
Terminology * Chronic thyroiditis, chronic lymphocytic thyroiditis * Part of spectrum of autoimmune thyroid diseases * Cellular and humoral-mediated thyroid destruction Imaging Findings * Tc-99m pertechnetate or I-123 scan: Pattern highly variable * I-123 or I-131 uptake: Variable, depending on stage Top Differential Diagnoses * Diffuse Nontoxic or Endemic Goiter * Riedel Struma: Fibrous Invasive Thyroiditis * Multinodular Goiter * Invasive/Infiltrative Disease * Recovering Subacute Thyroiditis * Medication Effects Pathology * US: Most common cause of hypothyroidism * Worldwide: 2nd leading cause of hypothyroidism (iodine deficiency = 1st) Clinical Issues * Hypothyroidism * Goiter * Other signs/symptoms: Hyperthyroidism or Hashitoxicosis (rare) Diagnostic Checklist * Radioactive iodine uptake: Increased, normal or decreased * Hashimoto thyroiditis on scan: May mimic Graves, multinodular goiter, nontoxic goiter, or other autoimmune thyroiditis |
|
|
|
Anterior thyroid scan shows Hashimoto thyroiditis (black arrow) with substernal goiter (black open).
Terminology * Chronic thyroiditis, chronic lymphocytic thyroiditis * Part of spectrum of autoimmune thyroid diseases * Cellular and humoral-mediated thyroid destruction Imaging Findings * Tc-99m pertechnetate or I-123 scan: Pattern highly variable * I-123 or I-131 uptake: Variable, depending on stage Top Differential Diagnoses * Diffuse Nontoxic or Endemic Goiter * Riedel Struma: Fibrous Invasive Thyroiditis * Multinodular Goiter * Invasive/Infiltrative Disease * Recovering Subacute Thyroiditis * Medication Effects Pathology * US: Most common cause of hypothyroidism * Worldwide: 2nd leading cause of hypothyroidism (iodine deficiency = 1st) Clinical Issues * Hypothyroidism * Goiter * Other signs/symptoms: Hyperthyroidism or Hashitoxicosis (rare) Diagnostic Checklist * Radioactive iodine uptake: Increased, normal or decreased * Hashimoto thyroiditis on scan: May mimic Graves, multinodular goiter, nontoxic goiter, or other autoimmune thyroiditis |
|
|
|
Well-Differentiated Thyroid Cancer, PET
Imaging Findings * PET scan indicated & approved for reimbursement by CMS in patients with thyroidectomy, radioactive I-131 therapy, elevated serum thyroglobulin, but negative I-131 whole body scan * Best FDG PET yield: Patients with stimulated thyroglobulin > 10 mU/L * FDG uptake by WDTC is often only moderate (mean SUV ~ 2.5 at 60 min) * Elevated thyrotropin (TSH) nearly doubles SUV in sites of WDTC over suppressed state * High resolution neck ultrasound: Preferred method for surveillance following I-131 therapy by most endocrinologists * FNA of any suspicious lymph nodes can be accomplished at the time of ultrasound * FDG PET should optimally be performed with elevated TSH * Optimized dosage schedule for rhTSH is not yet established, but Medicare pays for two injections; we recommend 0.9 gm IM on day 1 and day 2, and FDG PET on day 3-5 (all acceptable) Clinical Issues * If pre-Rx I-131 scan negative, consider giving therapeutic I-131 if Tg ↑: Often effective if post-Rx I-131 scan proves positive * Non-iodine avid recurrence: FDG PET may help identify areas ammenable to surgical removal Diagnostic Checklist * Focal uptake in thyroid may represent thyroid cancer (~ 50%) |
|
|

|
Well-Differentiated Thyroid Cancer
Anterior I-123 scan shows large cold nodule (10-20% chance of thyroid cancer). Imaging Findings * Primary: Cold nodule on radioiodine scan * Primary: Solid or mixed characteristics on ultrasound * Uptake in thyroid bed after surgery usually normal thyroid tissue * Follicular WDTC: Hematogenous spread to lungs, bones * Papillary WDTC: Lymphatic spread to cervical/mediastinal nodes, lung * Cold nodule on I-123 scan: May be hot/warm on Tc-99m O4- * Normal: Salivary glands, saliva, nasopharynx * Cervical nodes: Focal radioiodine uptake * Lung mets: Diffuse or focal (may be inapparent by CT) * Bone mets may be inapparent by conventional bone scan * Diffuse liver uptake rarely metastatic: Metabolized radiolabeled thyroid hormone * Non-iodine avid WDTC * FDG PET (stimulated scan more sensitive) * Low iodine diet 2 weeks prior to scan * Withhold thyroxine 4-6 weeks * May give Cytomel for 1 month, then withdraw 2-3 weeks prior to scan * I-131 2-3 mCi day 1, whole body scan day 3-4 * I-123, 800-1000 μCi day 1, whole body scan day 2 * Oblique neck images or Tc-99m O4- scan if salivary gland vs. lymph node * Non-iodine avid tumor: Tc-99m Sestamibi or FDG PET: Best if TSH elevated * Thyroglobulin > 2.0 ng/mL indicates thyroid tissue |
|
|

|
Graves
Terminology * Diffuse toxic goiter * Autoimmune thyrotoxicosis induced by thyroid stimulating antibodies (TSAs) Imaging Findings * Tc-99m pertechnetate or iodine-123 scan shows homogeneously increased uptake with high target-to-background levels * Superimposed nodules occur in 5-10% * ↑ Radioactive iodine uptake almost always present (> 35-40%); usually higher than other hyperthyroidism causes * If uptake exceeds 50-80%, Graves diagnosis confirmed Top Differential Diagnoses * Subacute Thyroiditis * Multinodular Goiter, Toxic Adenoma * Hashimoto disease with "Hashitoxicosis" * Medication/Contrast Effects * Non-Thyroid Endogenous Sources Pathology * Most common cause of hyperthyroidism * ↓ TSH most sensitive * Elevated T4, T3 despite ↓ TSH typical * Anti-thyroid antibodies: Anti-TSH receptor in serum Clinical Issues * Most common: 3rd-5th decade * Gender: M < F (1:7-8) |
|
|

|
Subacute Thyroiditis
Terminology * Subacute thyroiditis (SAT) * Inflammatory thyroid disorder with 3-phase clinical course Imaging Findings * Best diagnostic clue: Very low thyroid RAI uptake + clinical hyperthyroidism * In acute phase SAT, thyroid RAI uptake very low (often < 1% at 24 hours) * Uptake key to differentiating SAT from other causes of hyperthyroidism (e.g., Graves) * Uptake improves with recovery phase, eventually normalizes * RAI therapy contraindicated (self-limited disease) * Thyroid scan shows very low, absent thyroid activity in early SAT Top Differential Diagnoses * Graves Disease * Toxic Multinodular Goiter & Toxic Adenoma * Hashimoto Disease * Infiltrative Thyroid Diseases * Acute Thyroiditis * Iatrogenic Factors Diagnostic Checklist * Major cause of hyperthyroidism with very low uptake * Important to distinguish from other causes of hyperthyroidism because RAI therapy contraindicated * Most often, low thyroid uptake enough to diagnose SAT * Uptake may be normal in recovery phase of SAT * Thyroid scan necessary only in diagnostic dilemmas |
|
|
|
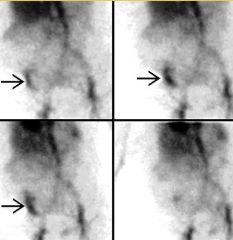
Posterior Tc-99m RBC scintigraphy shows persistent tracer in superior right hepatic lobe (black arrow) on delayed imaging, consistent with CH.
Imaging Findings * Tc-99m RBC scan: Most useful nuclear medicine imaging strategy * Initially photopenic, slow visualization, with subsequent filling by 2 hrs as RBCs slowly replace pooled blood in dilated sinusoids * Filling typically uniform or progressive from peripheral to central but can be opposite * On delayed imaging: Tc-99m RBCs in CH more intense than adjacent hepatic parenchyma * Limits of resolution on Tc-99m RBC scan 1-2 cm * Specificity ~ 99% in larger lesions * False positives very rare * 20-25 mCi (740-925 MBq) Tc-99m pertechnetate * Whole blood labeling kit to tag Tc-99m to RBCs in vitro * SPECT useful for 3D visualization and localization * Many lesions initially identified incidentally by other modalities: CT, MR, US Clinical Issues * Typical appearance requires no further imaging unless clinically indicated * Important to correctly identify CH with noninvasive imaging to avoid complications of biopsy (hemorrhage) Diagnostic Checklist * Tc-99m RBC scan in cases not characteristic of hemangioma by conventional imaging * Tc-99m RBC scan particularly useful with larger CH: Heterogeneous appearance can confound CECT/MR interpretation |
|
|
|
Coronal Tc-99m sulfur colloid SPECT shows subcapsular tracer accumulation in lateral portion of right hepatic lobe (black arrow).
Focal Nodular Hyperplasia Imaging Findings * Typical FNH: Fibrous central scar with radiating septae * Right lobe > left (2:1) * Usually 2-5 cm * Tc-99m IDA scintigraphy * Prompt tracer extraction 2° to ↑ vascularity * Delayed clearance: Disorganized biliary canaliculi ⇒ poor tracer transit * CECT, MR C+: Brightly enhancing on early arterial phase, delayed enhancement of central scar Top Differential Diagnoses * Hepatic Adenoma * Hepatocellular Carcinoma (HCC) or Metastatic Disease * Regenerative Nodules * Hemangioma * Superior Vena Cava Syndrome * Budd Chiari Syndrome, Hepatic Venous Occlusive Disease Diagnostic Checklist * Practical limits of resolution are 1-2 cm for SPECT, 2-3 cm for planar scintigraphy * Tc-99m HIDA: Early visualization with persistent tracer/delayed washout * Functional hepatocytes extract tracer promptly; disorganized canaliculi prevent rapid excretion * HCC: Initially cold to ≥ 1 hr, delayed fill-in can be seen (bile lakes) * Tc-99m SC: Lesions with iso- or hyper-accumulation do not require biopsy |
|
|
|
GI Bleeding Localization
Imaging Findings * Best diagnostic clue: Technetium (Tc) labeled red blood cells (RBC) appearing in tubular structure distinct from normal vascular or organ structure; moves in relatively short time intervals (min) * Upper GI bleed: Proximal to ligament of Treitz * Lower GI bleed: Distal to ligament of Treitz * Display: Frame by frame hard copy or computer monitor; cine loop for continuous viewing Top Differential Diagnoses * Peptic Ulceration and Erosive Gastritis * Esophageal Varices * Small Bowel Bleed * Diverticulosis and Colonic Angiodysplasia (AVM) Pathology * Duodenal ulcer (24%), gastric erosions (23%) * Gastric ulcer (21%), varices (10%) * Diverticulosis (43%), vascular ectasia (20%) Clinical Issues * Hematemesis: Bloody vomitus; red, coffee grounds * Melena: Black, tarry stools (100-200 mL of blood in upper GI tract is required to produce melena) * Hematochezia: Red blood per rectum * Occult blood detected by stool chemical testing Diagnostic Checklist * Tc-99m RBC for hemodynamically stable cases * Angiography for hemodynamically unstable cases |
|
|
|
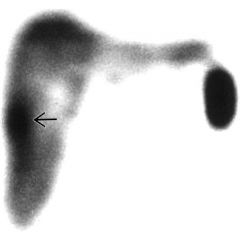
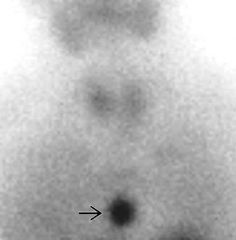
Anterior Meckel scan shows a focus of activity in the right lower quadrant (black arrow) whose intensity parallels that of the stomach and remains focal with no nearby bowel or renal activity.
meckel diverticulum Terminology * The remains of an improperly closed omphalomesenteric or vitelline duct arising from the ileum a short distance above the cecum which may contain ectopic gastric mucosa Imaging Findings * Focal increased activity usually but not necessarily in the right lower quadrant appears with a time course matching that of the stomach * Location: Usually in the right lower quadrant of the abdomen * Best imaging tool: Scanning using Tc-99m pertechnetate * The abnormality usually appears during the first ten minutes after tracer injection * Continuous imaging may be more helpful than static images * Stomach secretions passing into bowel should be prevented * Positioning the patient RPO while still positioning the camera to obtain anterior images is often sufficient to delay gastric emptying * Pharmacologic preparation is advised Top Differential Diagnoses * Gastrointestinal Bleeding from Other Causes * Intestinal Duplications Containing Gastric Mucosa * Visualization of Portion of the Right Ureter Diagnostic Checklist * Time course of the abnormal activity often parallels that of the stomach |
|
|
|
Terminology
* Complete, irreversible cessation of brain function * Medical determination of death has serious legal ramifications * An individual who (is dead) has sustained either * (1) Irreversible cessation of circulatory and respiratory functions * (2) Irreversible cessation of all functions of the entire brain, including the brain stem * A determination of death must be made in accordance with accepted medical standards Imaging Findings * Absence of uptake lipophyllic brain tracer [Tc-99m HMPAO (Ceretec), ECD (Neurolite, bicisate)] = brain death * Lipophyllic tracers: Do not require bolus technique * Lipophyllic tracers: Allow assessment of cerebrum & cerebellum/brainstem * Absence of brain perfusion on CBF scan (Tc-99m DTPA or Tc-99m pertechnetate) = brain death * Imaging may confirm but does not substitute for clinical criteria * Best imaging tool: Scintigraphy using lipophyllic tracers (consider bedside imaging if available) + EEG Top Differential Diagnoses * Diffuse Cerebral Edema * Technical Difficulty * Massive Cerebral Infarction Clinical Issues * Remember: BD is primarily clinical diagnosis, legal criteria vary |
General Features
* Best diagnostic clue o Absence of uptake lipophyllic brain tracer [Tc-99m HMPAO (Ceretec), ECD (Neurolite, bicisate)] = brain death + Lipophyllic tracers: Do not require bolus technique + Lipophyllic tracers: Allow assessment of cerebrum & cerebellum/brainstem o Absence of brain perfusion on CBF scan (Tc-99m DTPA or Tc-99m pertechnetate) = brain death + Limited in that requires good bolus technique and adequate cardiac output + Limited in that only allows assessment of anterior circulation (anterior and middle cerebral arteries) * Location: In many states, must assess CBF to both supra- and infratentorial brain (brainstem, cerebellum) * Imaging may confirm but does not substitute for clinical criteria |
|
|
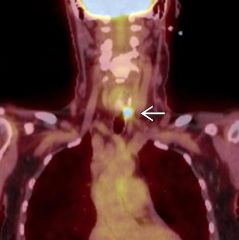
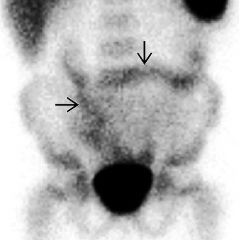
Parathyroid Adenoma, Ectopic
Anterior parathyroid scan shows focal increased activity (black arrow) overlying the mediastinum. At surgery, an intrathymic parathyroid adenoma was resected. Terminology * Parathyroid adenoma arising from aberrantly located parathyroid gland Imaging Findings * Best diagnostic clue: Focal increased activity in neck or thorax on parathyroid scintigraphy * Carotid sheath, thoracic inlet, mediastinum, great vessels, cardiac border * Up to 10% of solitary parathyroid adenomas ectopic * Best imaging tool: Tc-99m sestamibi parathyroid scintigraphy Top Differential Diagnoses * Benign Thyroid Pathology * Malignancy * Infection/Inflammation Clinical Issues * Directed surgical resection most common treatment |
|
|
|
autonomous functioning thyroid nodul
Inflammatory Bowel Disease Terminology * Inflammatory bowel disease (IBD), Crohn disease (CD), ulcerative colitis (UC), indeterminate colitis * Chronic inflammatory disease of gastrointestinal (GI) tract Imaging Findings * Focal, fixed accumulation of radiolabeled leukocytes at sites of inflammation in GI tract wall * CD: Activity in any part of GI tract (mouth to anus); terminal ileum (65-75%) > right colon > colon only (20-30%) > perianal; skip lesions * UC: Contiguous activity distally; rectum (almost always) > rectosigmoid (16%) > left colon (7%) > entire colon (4%); also backwash ileitis * Normal distribution in reticuloendothelial system (bone marrow, spleen, liver) * Tc-99m based agents show nonspecific activity in lungs, bowel, gallbladder, urine Top Differential Diagnoses * Infection * Vasculitis * Malignancy * Mesenteric Ischemia * GI Bleeding * Pancreatitis * Graft vs. Host Disease * Epistaxis * Infectious Colitides Diagnostic Checklist * Labeled leukocyte scintigraphy very sensitive but nonspecific for inflammation |
|

