![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
87 Cards in this Set
- Front
- Back
|
Does a periapical abscess result from acute or chronic periapical inflammation?
|

Periapical abscess = Acute
|
|
|
Does a periapical granuloma result from acute or chronic periapical inflammation?
|

Periapical granuloma = Chronic inflammation
|
|
|
What are some complications if a Periapical Abscess enters the blood stream?
|

Bacteremia
Cavernous sinus thrombosis |
|
|
What are some complications from Periapical Abscess penetration?
|

Penetration of the:
Mucosal sinus Skin sinus |
|
|
What are some complications if a Periapical Abscess Spreads to Soft Tissues?
|

Abscess
Cellulitis |
|
|
What are some complications if a Periapical Abscess Spreads through the jaw?
|

Osteomyelitis
Periosteitis |
|
|
What are some complications if a Periapical Abscess becomes chronic?
|

Chronic abscess
Chronic osteomyelitis |
|
|
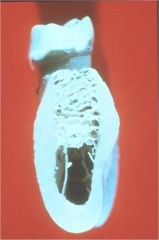
What condition arises as a result of a periapical granuloma?
|

Periapical (Radicular) Cyst
|
|
|
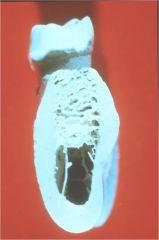
What is a mass of chronically inflamed granulation tissue at the apex of a non-vital tooth?
|

Periapical Granuloma (Chronic apical Periodontitis)
|
|

What are the Clinical Features of a Periapical Granuloma?
|

1. Asymptomatic but pain with acute exacerbation
2. Tooth shows No mobility or sensitivity to percussion 3. Tooth is NON-VITAL so it does Not respond to pulp testing |
|

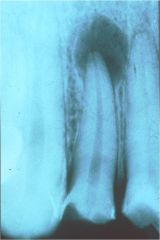
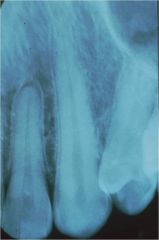
What are the Radiographic features of a Periapical Granuloma?
|
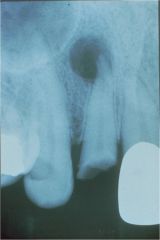
1. Circumscribed or ill-defined radiolucency
2. Loss of apical Lamina Dura 3. Root Resorption possible 4. Cannot differentiate a periapical granuloma from a cyst based on size and radiographic appearance |
|

How is a Periapical Granuloma Treated?
|

1. Root canal (if tooth is restorable)
2. Extract tooth and curettage of all apical soft tissue for microscopic examination (Non-Restorable tooth) 3. Follow restored asymptomatic teeth at 1 & 2 year intervals |
|

What are some of the possible sources of epithelium to create a Periapical Cyst? (radicular cyst, apical periodontal cyst)
|
Sources of epithelium include:
1. Rests of Malassez (most common) 2. Crevicular epithelium 3. Sinus lining 4. Sinus tract epithelium |
|

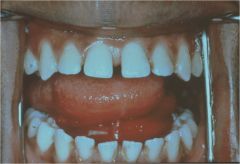
What are the clinical features of a Periapical Cyst?
|

1. Asymptomatic unless there is an acute exacerbation
2. Swelling and sensitivity from large cysts 3. Mobility of adjacent teeth as cyst enlargens 4. Non-Vital tooth (does not respond to pulp testing) |
|

What malignancy has been rarely reported in a periapical cyst?
|
Squamous Cell Carcinoma
|
|

What is the accumulation of acute inflammatory cells at the apex of a non-vital tooth?
|
Periapical abscess
|
|

What are two situations that would lead to periapical abscess?
|
1. de novo
2. acute exacerbation of a chronic periapical lesion |
|

What are the clinical features of Periapical Abscess?
|
1. Acute vs Chronic
2. Symptomatic vs Asymptomatic 2a. Symptomatic: pain, sensitivity to percussion, extruded tooth, and swelling 3. No response to Cold or Electric pulp testing 4. Headache, chills, fever, and malaise |
|
What are the radiographic features of a Periapical Abscess?
|
1. PDL may appear thickened or an ill-defined radiolucency
2. May not appear on radiograph if little bone destruction has occurred |
|

How is a periapical abscess treated?
|

1. Drain and eliminate the focus of the infection
2. Source of infection removed using endodontics or extraction 3. Analgesics & antibiotics are needed in severe cases |
|

What should you do if a periapical abscess progresses to a parulis?
|

It may subside after endo or extraction. If not it is surgically removed along with curettage of the sinus tract
|
|

What is a mass of subacutely inflamed granulation tissue at the opening of the intraoral sinus tract?
|

Parulis (gum boil)
|
|

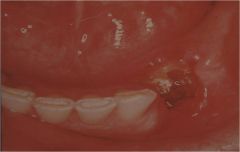
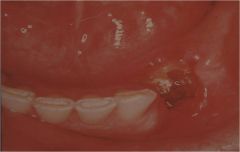
What are the clinical features of a parulis?
|
1. red tumescence (or yellow if pus filled)
2. Buccal gingiva 3. Children and young adults 4. Asymptomatic |
|

What is the cause of a parulis?
|
Parulis is caused by inflammation arising from a periodontal or periapical abscess
|
|
|
What is the significance regarding drainage of a parulis?
|
Cyclical drainage occurs until the underlying condition is resolved
|
|
|
What is a diffuse inflammation of soft tissues, which is not circumscribed or confinded to one area, but which in contradistinction to an abscess, tends to spread through tissue spaces and along fascial planes?
|

Cellulits
|
|
|
What are the two dangerous forms of cellulitis that are of interest to dentists?
|

Ludwig Angina
Cavernous Sinous Thrombosis |
|

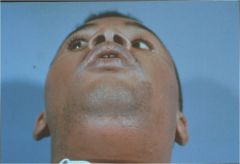
What are the Clinical features of Ludwig Angina?
|

1. Swelling of floor of mouth, tongue and submandibular region
2. Sublingual space involvement causes posterior enlargement, elevation and protrusion of the tongue (woody tongue) 3. Submandibular space enlargement causes enlargement and tenderness of the neck about the hyoid bone (bull neck) 4. Initially unilateral but progresses to bilateral 5. Pain in neck and floor of mouth 6. Dysphagia, dysphonia, dysarthria, drooling, sore throat and restricted neck movement may occur 7. Involvement of lateral pharyngeal space can cause respiratory obstruction 8. Tachypnea, dyspnea, tachycardia, stridor and restlessness 9. Fever, chills, leukocytosis and elevated SED rate is common |
|
What is the treatment of Ludwig Angina?
|
1. Maintenance of the airway
2. Antibiotic therapy 3. Surgical drainage |
|
|
What is the prognosis for Ludwig angina?
|
With appropriate therapy, the incidence of mortality is 8%
|
|
|
What are the clinical features for Cavernous Sinus Thrombosis?
|
1. Swelling around the eye with enlargement of the eyelids and conjunctiva
2. Protrusion and fixation of the eyeball may occur 3. Induration and swelling of forehead and nose is common 4. Lacrimation, photophobia, pupil dilation and loss of vision 5. Pain over the eye and along the opthalmic and maxillary branches of the trigeminal nerve occurs 6. Fever, chills, sweating, tachycardia, nausea and vomiting 7. CNS involvement includes tachycardia, tachypnea, irregular breathing, stiff neck, stupor and delirium 8. Brain abscess possible |
|
|
What is the treatment for Cavernous Sinus Thrombosis?
|
1. Extract tooth
2. Establish drainage 3. High dose antibiotics 4. Corticosteroids to decrease inflammation and prevent vascular collapse 5. Anticoagulant may or may not help. One theory is they prevent thrombosis and septic emboli, but some say their usage increases vascular complications. |
|
|
What is an acute or chronic inflammatory process in the medullary spaces or cortical surfaces of bone that extends away from the intitial site of involvement. In the oral region, it is usually a bacterial infection.
|
Osteomyelitis
|
|
|
What are some predisposing factors of osteomyelitis?
|
1. Alcohol & tobacco use
2. IV drug use 3 Diabetes mellitus 4. Malaria 5. Anemia 6. Malnutrition 7. Malignancy 8. AIDS 9. Radiation, osteopetrosis, osteitis deformans (Paget disease) and late stage cemento-osseous dysplasia may result in hypovascularized bone |
|
|
What are the demographics for Acute Osteomyelitis?
|
1. All ages may be affected
2. Men mostly 3. Mandible primarily involved |
|
What are some of the clinical manifestations of Acute Osteomyelitis?
|
Fever, leukocytosis, lymphadenopathy, significant sensitivitym pain or paresthesia may occur. Soft tissue swelling and redness may be present.
|
|
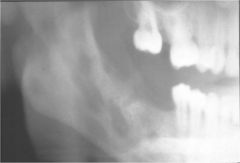
How does Acute Osteomyelitis appear radiographically?
|

1. Radiographs may be unremarkable or demonstrate an ill-defined radiolucency
2. Fragments of necrotic bone may separate from vital bone and be exfoliated (sequestrum) |
|
|
How is Acute Osteomyelitis treated?
|
Antibiotics and drainage
Most of the time this is sufficient and does not need surgery |
|
|
What are some clinical manifestations of Chronic Osteomyelitis?
|
1. Swelling, pain, sinus formation, purulent discharge, sequestrum formation, tooth loss or pathologic fracture may occur.
2. During quiescent periods, the lesions may be asymptomatic or present minimal discomfort |
|
What does Chronic Osteomyelitis look like radiographically?
|
Patchy, ragged, and ill-defined radiolucency often containing sclerotic foci. This is often referred to as a Moth-Eaten pattern
|
|
|
How is Chronic Osteomyelitis treated?
|

1. Antibiotics administered Intravenously in High Doses
2. Surgical removal of all infected tissue 3. Scintigraphic techniques 4. Hyperbaric oxygen 5. Direct delivery of antibiotics via antibiotic-impregnated polymethyl-methacrylate beads |
|
|
What diagnosis encompasses a group of presentations that are characterized by pain, inflammation and varying degrees of gnathic periosteal hyperplasia, sclerosis and lucency?
|

Diffuse Sclerosing Osteomyelitis
|
|
|
What are three categories that Diffuse Sclerosing Osteomyelitis is discussed?
|

1. Diffuse sclerosing osteomyelitis
2) Chronic Tendoperiostitis 3) SAPHO syndrome |
|
|
When is the term Diffuse Sclerosing Osteomyelitis allowed?
|
Only in cases where the infectious process is Directly (not secondarily, ie florid cemento-osseous dysplasia with superimposed inflammation) responsible for the bony sclerosis
|
|
What is a residual area of condensing osteitis that remains after resolution of the inflammatory focus?
|
Bone Scar
|
|

What is characterized as localized areas of bone sclerosis associated with the apices of teeth with pulpitis or pulpal necrosis?
|

Condensing Osteitis
|
|
|
What is another term for condensing osteitis?
|
Focal Sclerosing Osteomyelitis = Condensing Osteitis
|
|
|
What are some other terms for Osteomyelitis w/Proliferative Periostitis?
|
Osteomyelitis w/Proliferative Periostitis = Periostitis Ossificans = Garre's Osteomyelitis
|
|

If bony destruction is seen in association with the cortical surface or new periosteal bone, then one should consider the possibility of a neoplastic process like Ewing sarcoma. What condition is this associated with?
|

Proliferative periostitis
|
|
|
What are the other terms for Alveolar Osteitis?
|
Dry Socket = Fibrinolytic Alveolitis = Alveolar Osteitis
|
|
|
What develops as a result of destruction of the blood clot which naturally occurs following tooth extraction, preventing normal healing?
|
Alveolar Osteitis
|
|
|
Local trauma, estrogens and bacterial pyrogens are known to stimulate _______ which can destroy the clots. This is Alveolar Osteitis.
|
Fibrinolysins
|
|
|
What is the frequency of Alveolar Osteitis related to extrations?
|
25-30% of impacted mandibular 3rd molar extractions
1-3% of all extractions overall |
|
|
How long does it take to develop dry socket and once established, how long until it resolves?
|
3-4 days develop
10-40 days resolve |
|
|
Which patients are high risk for Alveolar Osteitis?
|
1. Taking oral contraceptives
2. Smokers 3. Existing pericoronitis 4. alveolar osteitis Hx 5. more traumatic extractions |
|
|
Which patients are high risk for Alveolar Osteitis?
|
1. Taking oral contraceptives
2. Smokers 3. Existing pericoronitis 4. alveolar osteitis Hx 5. more traumatic extractions |
|

How does Acute Osteomyelitis Present Radiographically?
|
Unremarkable or have an ill-defined radiolucency
Necrotic bone separates,forming sequestrum |
|
|
Which condition presents clinically as Fever, leukocytosis, lymphadenopathy, significant sensitivity, pain or paresthesia, soft tissue swelling and redness?
|
Acute Osteomyelitis
|
|
|
How is Acute Osteomyelitis treated?
|

Antibiotics and Drainage
Rarely need surgery |
|
How does Chronic Osteomyelitis present radiographically?
|

Patchy, ragged, and ill-defined radiolucency, sclerotic foci, Moth Eaten
|
|

Which condition presents as Swelling, pain, sinus formation, purulent discharge, sequestrum, tooth loss, pathologic fracture?
|

Chronic Osteomyelitis
|
|
How is Chronic Osteomyelitis treated?
|

IV antibiotics in high doses
Surgical removal of infected tissue Scintigraphic, Hyperbaric oxygen, Direct delivery of antibiotics |
|

What demographic is mostly affected by Diffuse Sclerosing Osteomyelitis?
|

Adults
|
|

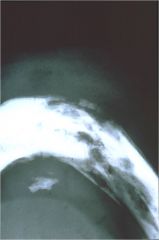
How does Diffuse Sclerosing Osteomyelitis manifest radiographically?
|

Increased radiodensity around sites of chronic infection. Multifocal or entire quadrant.
|
|
|
How does Diffuse Sclerosing Osteomyelitis present clinically?
|

No pain or swelling
|
|
|
How is Diffuse Sclerosing Osteomyelitis treated?
|

Remove the source of the infection
|
|
|
How does Chronic Tendoperiostitis present radiographically?
|
Areas of radiolucency are observed in areas of radiodensity. Sclerosis is limited to one quadrant. Erosion of inferior border of mandible.
|
|
|
How does Chronic Tendoperiostitis manifest clinically?
|
Recurrent pain, swelling of cheek and trismus
|
|
|
How is Chronic Tendoperiostitis treated?
|
Resolving muscle overuse (relaxation techniques, exercises, splints)
|
|
|
What does SAPHO stand for?
|
Synovitis Acne Pustulosis Hyperostosis and Osteitis
|
|
|
What demographic is most affected by SAPHO?
|
< 60 years old mostly affected
|
|
|
How does SAPHO present radiographically?
|
Diffuse areas of osteolysis with some bony sclerosis
|
|
|
What is another term for SAPHO (Synovitis Acne Pustulosis Hyperostosis and Osteitis)?
|
CRMO (Chronic Recurrent Multifocal Osteomyelitis)
|
|
|
What is significant regarding clinical manifestation of SAPHO?
|
Bone lesions may present without associated skin involvement
|
|
|
How is SAPHO treated?
|
Steroids and NSAIDs
Typically incomplete resolution |
|
|
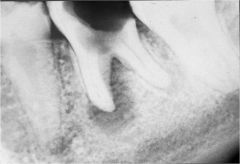
Who is mostly affected by Condensing or Focal Sclerosing Osteitis?
|
Children in the Mandibular molar/premolar region
|
|

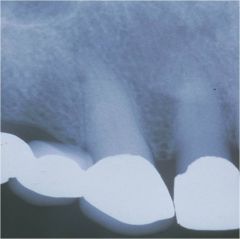
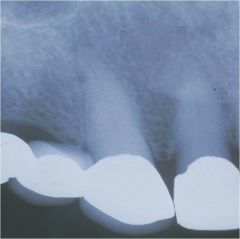
How does Condensing Osteitis present radiographically?
|

Radiodensity near the apex of the tooth exhibiting a thickened PDL or apical inflammatory lesion
No radiolucent border Not separated from apex of tooth |
|

What causes condensing osteitis?
|

Tooth pulp has pulpitis or necrosis
|
|
|
How is Condensing Osteitis treated?
|
Do NOT expand the jaw during diagnosis
Endodontics or extraction bone scar |
|
|
What age is most affected by Osteomyelitis with proliferative periostitis?
|
mean age of 13
affects the mandibular molar/premolar region and inferior border of the mandible |
|
|
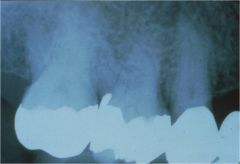
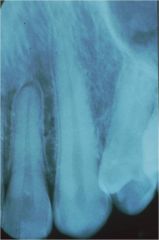
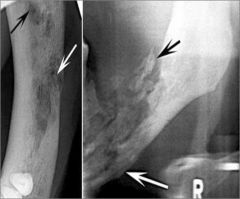
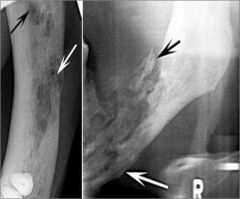
How does Osteomyelitis with proliferative periostitis present radiographically?
|
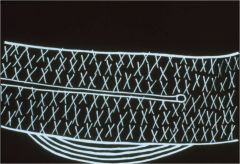
Radiopaque laminations of bone that roughly parallel each other and the underlying cortical surface
|
|
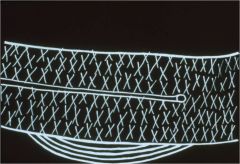
How does Osteomyelitis with proliferative periostitis manifest clinically?
|

It is a periosteal reaction to the presence of inflammation from a Carious tooth.
Periosteum forms rows of reactive, vital bone that parallel each other and expand the bone |
|
|
How is Osteomyelitis with proliferative periostitis treated?
|
Endodontics or Extraction
Typically takes 6-12 months to resolve after treatment |
|
|
What age range is most affected by alveolar osteitis?
|
40-45
|
|
How does alveolar osteitis present clinically?
|

Clot is lost leaving a bare bony socket.
Severe pain and foul odor |
|

How is Alveolar Osteitis treated?
|
Irrigate the socket then pack with an obtundent and an antiseptic dressing (iodoform gauze with eugenol)
Change dressing every 24 hours for the first 3 days the every 2-3 days |
|
|
**********************************
What are three Periapical conditions that are associated with NON-Vital teeth? ********************************** |
1. Periapical Cyst
2. Periapical Granuloma 3. Periapical Abscess |

