![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
145 Cards in this Set
- Front
- Back
|
what is the normal number of RBC/microL?
|
4-5x10^6
|
|
|
what is the diameter of a normal RBC?
|
7-8 micrometers and 2 micrometers thick
|
|
|
how do RBCs generate energy?
|
they lack mitochondria and other cellular organelles (including a nucleus) so they rely on anaerobic glycolysis for energy in maintaining hemoglobin function
|
|
|
why do RBC's have a limited lifespan?
|
they lack organelles such as nucleus or ribosomes to renew proteins for function
|
|
|
what is the avg. lifespan of a RBC?
|
120 days
|
|
|
describe the diameter of a microcyte (RBC)?
|
<6 micrometers
|
|
|
describe the diameter of a macrocyte?
|
9-12 micrometers
|
|
|
what is the name of the condition where RBC's become swollen, loose hemoglobin due to lysis or leaky membrane, and the hemoglobin is excreated in large numbers in the urine?
|
Black water fever
|
|
|
what happens when the blood becomes hypertonic when compared to the RBC?
|
crenation - RBC's shrink which causes the formation of tiny spins which extend from their surface
|
|
|
in a RBC, what facilitates the formation of carbonic acid from CO2 and H2O?
|
carbonic anhydrase
|
|
|
what does carbonic acid disassociate into?
|
1. H+
2. HCO3 (bicarbonate) |
|
|
in what form is most of the CO2 generated by cells carried to the lungs?
|
bicarbonate
|
|
|
describe the process by which bicarbonate is able to cross the RBC membrane?
|
the integral membrane protein, AE1 couples the efflux of bicarbonate with influx of chloride (Cl-)
|
|
|
in addition of AE1 what other enzymes can be found in RBC's?
|
those of the glycolytic pathway and the monophosphate shunt
|
|
|
describe the lipid, carbohydrate, and protien components of the RBC cell membrane?
|
50% protein
40% lipid 10% carbohydrates |
|
|
what is the cytoskeleton composed of in the RBC?
|
1. spectric tetramers
2. actin protofilaments 3. band 4.1 |
|
|
what holds the cell membrane to the RBC cytoskeleton?
|
ankyrin, which attaches the cytoskeleton to AE1 in the cell membrane
|
|
|
what are the most common Rh antigens in the human population?
|
C, D, and E
|
|
|
what percentage of Americans have an Rh antigen on their RBC's?
|
85%
|
|
|
What type of cell is described below?
Bluish pink cytoplasm (or blue cytoplasmic reticulum if stained with brilliant cresyl blue); no nucleus; biconcave disk-shaped; diameter 7-8 μm |
Reticulocyte
|
|
|
how many reticulocytes are in 1 L?
|
25-85x10^9
|
|
|
what type of blood component is described below?
|
Pale blue cytoplasm;
purple granules; no nucleus; biconvex disk-shaped; diameter 3 μm |
|
|
what number of platelets are found in 1 L of normal blood?
|
150-350x10^9
|
|
|
how long do reticulocytes circulate in the blood before the mature?
|
2 days
|
|
|
how long do platelets circulate in the blood?
|
9-10 days
|
|
|
describe the avg. amount of leukocytes per microL?
|
6000-10000
|
|
|
what are the two main groups of leukocytes?
|
1. granulocytes
2. agranulocytes |
|
|
what types of granules are described below?
found only in granulocytes; their staining properties (neutrophilic, eosinophilic, or basophilic) distinguish the three granulocyte types |
Specific granules
|
|
|
what types of granules are described below?
Occur in both agranulocytes and granulocytes. Their content of lytic enzymes suggests that they function as lysosomes. |
Azurophilic granules
|
|
|
what are the 2 categories of agranulocytes?
|
1. leukocytes
2. monocytes |
|
|
The following describes which category of leukocytes?
Unsegmented nuclei and are described as mononuclear leukocytes |
agranulocytes
|
|
|
what types of granules could be found in a lymphocyte of monocyte?
|
Azurophilic only
|
|
|
what is the normal variation percentage of lymphocytes in the white blood cell count of normal blood
|
20-45%
|
|
|
what are the 2 major types of lymphocytes?
|
1. Memory and effector cells
2. Null cells |
|
|
what percentage of lymphocytes in the blood are T cells?
|
80%
|
|
|
when stimulated by an antigen, what do lymphocytes do?
|
the undergo blast transformation which is characterized by enlargement and sequential mitotic divisions
|
|
|
what to B cells differentiate into?
|
plasma cells which produce antibodies
|
|
|
what do T cells differentiate into? (3)
|
they can become
1. Cytotoxic (killer) cells 2. Helper T cells 3. Suppressor T cells |
|
|
what are the variety of signaling molecules which T cells release that influence the activity of macrophages and other leukocytes involved in an immune response?
|
lymphokines (ex interferon)
|
|
|
What type of cells is described below?
Circulating cells that morphologically resemble lymphocytes but exhibit neither B-cell nor T-cell They may represent circulating stem cells of lymphocytes or other blood cell types. |
null cells (type of lymphocyte)
|
|
|
what are the two primary lymphoid organs in the human?
|
1. thymus = T cell programing
2. bone marrow = B cell programing |
|
|
Does this describe a antigen activated or primarily circulating lymphocyte?
Spherical, often flattened on one side, densely heterochromatic, purplish blue to black |
primarily circulating lymphocyte
|
|
|
Does this describe a antigen activated or primarily circulating lymphocyte?
Large, less heterochromatic, reddish purple. |
antigen activated
|
|
|
Does this describe a antigen activated or primarily circulating lymphocyte?
Thin rim around nucleus, pale basophilia, many ribosomes, sparse ER, few mitochondria, small Golgi, few azurophilic granules, no specific granules. |
primarily circulating lymphocyte
|
|
|
Does this describe a antigen activated or primarily circulating lymphocyte?
More abundant, pale basophilia, many ribosomes, sparse ER, few mitochondrial, small Golgi, few azurophilic granules, no specific granules. |
antigen activated
|
|
|
what type of WBC is described below?
Mean circulation time 10 hours for majority of cells; variable time in lymphoid organs and tissues; majority of cells are long lived. |
Lymphocyte
|
|
|
what type of WBC is described below?
Circulate for 1-3 days; variable time in tissues. |
Monocyte
|
|
|
what type of WBC is described below?
Circulation time 6-10 hours; 2-3 days in tissues. |
Neutrophil
|
|
|
what type of WBC is described below?
Circulation time 1-10 hours; up to 10 days in tissues. |
Eosinophil
|
|
|
what type of WBC is described below?
Circulation time estimated as 1-10 hours; variable time in tissues. |
Basophil
|
|
|
what type of WBC is described below?
Nucleus is usually kidney- or horseshoe- shaped, eccentric. Chromatin less dense, “smudgy” appearance, reddish purple, 2-3 nucleoli may be seen. |
Monocyte
|
|
|
what type of WBC is described below?
Cytoplasm is abundant, faint blue-gray, many small azurophilic granules, no specific granules, many small mitochondria, well-developed Golgi, sparse RER and olyribosomes |
Monocyte
|
|
|
what type of WBC is described below?
Condensed chromatin, multilobed (usually 3 lobes, more than 5 [hypersegmented] in aging cells), small heterochromatic drum stick may extend from one lobe. Represents female Barr body (inactive X chromosome). |
Neutrophil
|
|
|
what type of WBC is described below?
Abundant small (0.3-0.8 μm), salmon pink, specific (neutrophilic) granules; fewer reddish-purple azurophilic granules. Specific granules contain alkaline phosphatase and bactericidal cationic proteins called phagocytins, abundant glycogen. |
Neutrophil
|
|
|
what type of WBC is described below?
Condensed chromatin, usually 2 lobes, often partly obscured by abundant specific granules. |
Eosinophil
|
|
|
what type of WBC is described below?
Abundant large (0.5-1.5 μm), brightly eosinophilic, specific granules that are specialized lysosomes carrying peroxidase, acid phosphatase, cathepsin, ribonuclease and major basic protein (MBP, eosinophilic antiparasitic agent). In EMs, specific granules are ovoid with a dense internum surrounded by an electronlucent externum. Fewer, reddishpurple azurophilic granules. |
Eosinophil
|
|
|
what type of WBC is described below?
Condensed chromatin, usually 3 lobes often in an S shape, partially or completely obscured by abundant, dark specific granules. |
Basophil
|
|
|
what type of WBC is described below?
Less abundant, variable sized (0.3-1.5 μm), reddish-violet to black specific basophilic) granules. Granules contain heparin and histamine to be released in response to allergic stimuli. Fewer, reddish-purple azurophilic granules. |
Basophil
|
|

what type of WBC is this?
|
basophil
|
|
what type of WBC is this?
|
basophil
|
|
what type of WBC is this?
|
eosinophil
|
|

what type of WBC is this?
|
eosinophil
|
|

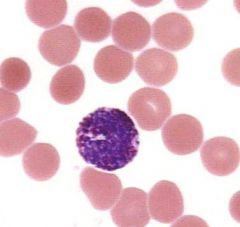
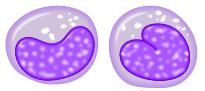
what type of WBC is this?
|
lymphocyte
|
|
what type of WBC is this?
|
lymphocyte
|
|
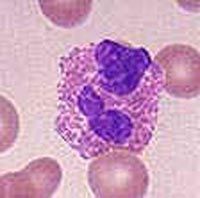
what type of WBC is this?
|
macrophage
|
|
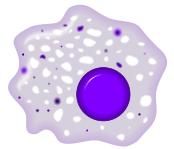
what type of WBC is this?
|
macrophage
|
|
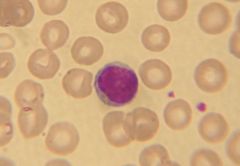
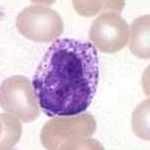
what type of WBC is this?
|
monocyte
|
|

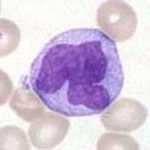
what type of WBC is this?
|
neutrophil
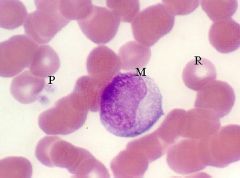
|
|
what type of WBC is this?
|
basophil
|
|
what type of WBC is this?
|
Monocyte
|
|

what type of WBC is this?
|
Neutrophil
|
|
|
what are the most abundant circulating leukocytes?
|
neutrophils (60-70%) of circulating RBC's
|
|
|
how often do neutrophils undergo mitosis?
|
never, they are completely differentiated
|
|
|
what type of WBC makes up 1-4% of the circulating WBCs?
|
Eosinophils
|
|
|
what do eosiniphils preferentially phagocytize?
|
antigen/antibody complexes
|
|
|
when can the numbers of circulating eosinophils be seen to increase?
|
during parasitic infections and allergic responses
|
|
|
when do levels of eosinophils drop in blood?
|
during corticosteroid therapy
|
|
|
what are the least numerous leukocytes?
|
basophils <1% of all circulating WBC's
|
|
|
what cells do basophils function very similarly to?
|
mast cells
|
|
|
what are the smallest formed elemets in the blood?
|
platelets
|
|
|
what cells produce platelets through a process of budding?
|
megakaryocytes
|
|
|
what is the typical lifespan of a platelet cell?
|
8 days
|
|
|
how many platelets can be found in a normal microliter of blood?
|
150,000-300,000
|
|
|
what are the two distinct regions of platelets?
|
the hyalomere and the granulomere
|
|
|
does the following describe the hyalomere or granulomere of a platelet?
Contains a few mitochondria, glycogen granules, and various purple granules. |
granulomere
|
|
|
which platelet granule is described below?
Contain fibrinogen, platelet-derived growth factor, and other platelet-specific proteins? |
Alpha granules
|
|
|
What type of platelet granules are described below?
contain calcium ions, pyrophosphate, ADP, and ATP; take up and store serotonin |
Dense bodies (delta granules)
|
|
|
What type of platelet granules are described below?
contain fibrinogen, platelet-derived growth factor, and other platelet-specific proteins |
Alpha granules
|
|
|
What type of platelet granules are described below?
contain only lysosomal enzymes |
Lambda granules
|
|
|
what does this describe, the granolomere or the hyalomere?
contains a marginal bundle of microtubules that helps to maintain the platelet’s discoid shape |
hyalomere
|
|
|
Describe the structure and composition that allows platelets to achieve there ultimate function of adhesion during clot formation?
|
glycocalyx - rich in glycosaminoglycans
|
|
|
where is the Surface-opening tubule system found in a platelet and what is its function?
|
Hyalomere and it expedites rapid uptake and release of molecules from activated platelets
|
|
|
where is the Dense tubular system found in a platelet and what is its function?
|
Hyalomere and it probably sequesters calcium
ions to prevent platelet “stickiness” |
|
|
what is the function of the compenents found in α-Granules?
|
Contains factors that facilitate vessel repair, platelet aggregation, and coagulation of blood
|
|
|
what is the function of the compenents found in δ-Granules (dense bodies)?
|
Contained factors facilitate
platelet aggregation and adhesion, as well as vasoconstriction |
|
|
what is the function of the compenents found in λ-Granules (lysosomes)?
|
Contains enzymes that facilitate clot resorption
|
|
|
describe the fluid content of extracellular space as compared to that of blood for small molecules and electrolytes?
|
that are practially the same because they are constantly being interchanged
|
|
|
describe the concentration of proteins in the extracellular fluid as compared to that in blood?
|
much lower in extracellular fluid
|
|
|
what is the chief protein in the bloods colloid osmotic pressure?
|
albumin
|
|
|
what are the 5 major types proteins found in blood?
|
1. albumin
2. lipoproteins 3. globulins 4. compliment 5. clotting proteins such fibrinogen |
|
|
aside from their function in immunity, what other functions do globulins carry out?
|
Transports metal ions, protein-bound lipids, and lipid-soluble vitamins
|
|
|
what are the three lopiproteins one might find in the blood?
|
1. Chylomicrons
2. VLDL 3. LDL |
|
|
what provides the structure/scaffolding for the components of bone marrow?
|
reticular cells and reticular fiber
|
|
|
how do the blood cells and platelets formed in the bone marrow get into the blood stream?
|
through the sinusoids throughout the bone marrow comparments which have large gaps allowing passage of cells and platelets
|
|
|
reticular fibers are composed of which type of collagen?
|
type 3
|
|
|
what is another name for reticular cells?
|
adventitial cells
|
|
|
where are RBC's brocken down? (3)
|
1. Bone marrow
2. Liver 3. Spleen |
|
|
when an RBC is broken down what are the 3 components that must be delt with?
|
1. globin
2. porphyrin rings 3. iron |
|
|
what is the name of stored iron in macrophages?
|
ferritin and hemosiderin
|
|
|
how are porphyrin rings taken from the body?
|
they are conjugated with bilirubin
|
|
|
what is the group of a macrophage supplying iron to surrounded developing erythrocytes called?
|
erythroblastic island
|
|
|
what are the 2 important types of cytokines that stimulate WBC formation?
|
1. colony-stimulating factors (CFSs) and interluekins
|
|
|
What factor has this function?
Promotes CFU-GM mitosis and differentiation; facilitates granulocyte activity |
GM-CSF
|
|
|
What factor has this function?
Promotes CFU-G mitosis and differentiation; facilitates neutrophil activity |
G-CSF
|
|
|
What factor has this function?
Promotes CFU-M mitosis and differentiation |
M-CSF
|
|
|
What factor has this function?
Promotes proliferation of PHSC, CFU-S, and CFU-Ly; suppresses erythroid precursors |
IL-1
|
|
|
What factor has this function?
Stimulates activated T- and B-cell mitosis; induces differentiation of NK cells |
IL-2
|
|
|
What factor has this function?
Promotes proliferation of PHSC, CFU-S, and CFU-Ly as well as all unipotential precursors (except for LyB and LyT) |
IL-3
|
|
|
What factor has this function?
Stimulates T- and B-cell activation and development of mast cells and basophils |
IL-4
|
|
|
What factor has this function?
Promotes CFU-Eo mitosis and activates eosinophils |
IL-5
|
|
|
What factor has this function?
Promotes proliferation of PHSC, CFU-S, and CFU-Ly; also facilitates CTL and B-cell differentiation |
IL-6
|
|
|
What factor has this function?
Promotes differentiation of CFU-LyB; enhances differentiation of NK cells |
IL-7
|
|
|
What factor has the following function?
Induces neutrophil migration and degranulation |
IL-8
|
|
|
What factor has the following function?
Induces mast cell activation and proliferation; modulates IgE production; promotes T helper cell proliferation |
IL-9
|
|
|
What factor has the following function?
Inhibits cytokine production by macrophages, T cells, and NK cells; facilitates CTL differentiation and proliferation of B cells and mast cells |
IL-10
|
|
|
What factor has the following function?
Stimulates NK cells; enhances TCL and NK cell function |
IL-12
|
|
|
which cells produce GM-CSF?
|
T cells; endothelial cells
|
|
|
which cells produce G-CSF?
|
Macrophages; endothelial cells
|
|
|
which cells produce M-CSF?
|
Macrophages; endothelial cells
|
|
|
which cells produce IL-1
|
Monocytes; macrophages; endothelial cells
|
|
|
which cells produce IL-2?
|
Activated T cells
|
|
|
which cells produce IL-3
|
Activated T and B cells
|
|
|
what cells produce IL-4?
|
Activated T cells
|
|
|
what cells produce IL-5?
|
T cells
|
|
|
what cells produce IL-6?
|
Monocytes and fibroblasts
|
|
|
what cells produce IL-7?
|
Adventitial reticular cells?
|
|
|
what cells produce IL-8?
|
Leukocytes, endothelial cells, and smooth muscle cells
|
|
|
what cells produce IL-9?
|
T helper cells
|
|
|
what cells produce IL-10?
|
Macrophages and T cells
|
|
|
what cells produce IL-12?
|
Macrophages
|
|
|
where does the production of blood cells first occure?
|
in blood islands in the wall of the yolk sac
|
|
|
during what week of development does blood production begin?
|
after 2 weeks
|
|
|
from the 2nd to the 6th month of intrauterine life, what are the main hematopoietic organs?
|
liver and spleen
|
|
|
where are most bone marrow aspirate and biopsies taken from?
|
anterior or posterior illiac crests
|
|
|
extramedullary hematopoiesis and myeloid metaplasia are examples of what?
|
when the fetal organs for blood formation become active in that role during adulthood
|

