![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
211 Cards in this Set
- Front
- Back
|
What are causes of microcytic anemia: |
-Iron deficiency
-Thalassemia -Anemia of chronic disease -Lead poisoning -Sideroblastic anemia |
|
|
Causes of leukocytosis:
|
-Pertusses
-Infectious mononucleosis |
|
|
Causes of eosinophilia:
|
-Allergies
-Neoplasia -Parasitic disease -Collagen vascular disease -Neoplasia |
|
|
When you find basophilia what disease should you think up?
|
Think CML leukemia
|
|
|
Causes of macrocytosis:
|
-B12 and folate deficiency
-Ethanol abuse -AZT use -Hemolytic anemia |
|
|
what are megaloblastosis (hypersegmented neutrophils) a sign for?
|
-B 12 deficiency
-Folate deficiency -Pernicious anemia |
|
|
Target shaped RBCs represent:
|
Thalassemias
|
|
|
Heinz bodies RBCs represent:
|
Sideroblastic
|
|
|
What is the amount of iron given with intravenous iron (Ferrlecit)?
|
250 mg intravenous Q day times four days.
|
|
|
Sources of Von Willebrand factor:
|
-Cryoprecipitate
-Desmopressin |
|
|
How does tPA work?
|
TPA or tissue plasminogen activator activates plasminogen. Plasminogen ultimately degrades fibrin clots.
|
|
|
What does HLA stand for?
|
Human leukocyte antigen
|
|
|
Medications that cause leukopenia:
|
-Bactrim
-Semisynthetic penicillin -Dilantin -Carbamazepine -Clozapine |
|
|
What is normal retic count?
|
0.5 to 1.5% of RBCs
|
|
|
What to think about when you see spooning of nails?
|
Iron deficiency anemia
|
|
|
What is normal MCV?
|
80 to 100
|
|
|
What is the name of the storage form of iron?
|
Ferritin
|
|
|
What is the test dose of iron dextran?
|
0.5 mL. To test for rare side effect of anaphylaxis.
|
|
|
What condition should iron dextran be avoided in?
|
Rheumatoid arthritis since free radical iron may precipitate RA flares.
|
|
|
Causes of anemia of chronic disease:
|
Any chronic inflammatory state such as:
-CKD -Autoimmune diseases -Etc. |
|
|
What are the two categories of hemolytic anemias:
|
1. Intravascular
2. Extravascular (in the spleen) |
|
|
What type of hemolytic anemia do you see normal haptoglobin levels and no heme or hemosiderin in the urine?
|
In extravascular or splenic hemolysis
|
|
|
The hemosiderin found in the urine in a hemolytic process comes from what?
|
Hemoglobin is absorbed into the proximal renal tubul's where it is degraded ultimately into hemosiderin.
|
|
|
Lab values to expect in intravascular hemolytic anemia:
|
-Retic count elevated
-Indirect Bili elevated -LDH elevated -haptoglobin reduced or absent -Positive hemosiderin in urine |
|
|
Treatment of hemolytic anemia?
|
-Steroids
-Intravenous immunoglobulin -Splenectomy if above ineffective and process extravascular |
|
|
What is the pathophysiology and hereditary Sperocytosis?
|
The RBC shape change lead to a decrease in deformability and thus splenic sequestration. This is why there is splenomegaly along with jaundice condition. Typically there is also a personal lifetime history of episodic episode of hemolysis.
|
|
|
Test to diagnose hereditary Sperocytosis?
|
Osmotic fragility test
|
|
|
What is the function of glucose-6-phosphate dehydrogenase?
|
G6PD protects RBCs from membrane oxidation
|
|
|
If peripheral smear shows Heinz bodies what condition should you think of?
|
-G6PD deficiency
-Also seems sometimes with thalassemia |
|
|
What condition to consider when you see a triad of: chronic hemolytic anemia, cytopenia or pancytopenia, recurrent venus thrombosis:
|
Proximal nocturnal hemoglobinuria. This is a rare intravascular hemolytic anemia. The disease process renders RBCs sensitive to complement mediated hemolysis. This condition is frequently fatal.
|
|
|
What is the difference in warm and cold autoimmune hemolytic anemias?
|
Warm hemolytic anemia is not a complement mediated process like cold. Steroids work in warm but not cold.
|
|
|
What should you be aware of if giving ceftriaxone to a sickle cell patient?
|
Massive hemolysis
|
|
|
Indications for exchange transfusion in sickle cell disease:
|
-Acute chest syndrome
-Priapism -CVA -Debilitating painful crises |
|
|
What is the leading cause of death in adults with sickle cell disease?
|
Acute chest syndrome which is cause sickling and vasoocclusion in the pulmonary vessel beds with resultant infarction.
|
|
|
What is the basic genetic pathophysiology of sickle cell anemia?
|
And amino acid transposition of valine for glutamic acid.
|
|
|
What is the basic pathophysiology of thalassemias?
|
Inherited disorders of alpha or beta globin, where the rate of production of hemoglobin molecule is reduced. Decreased hemoglobin synthesis causes microcytosis, and unbalance synthesis of alpha and beta globins lead to ineffective erythropoiesis and hemolysis.
|
|
|
What prominent lab value do you see with thalassemias?
|
-Disproportionately low MCV (microcytic and hypochromic)
-Target cells -Possible Heinz bodies |
|
|
General causes of bone marrow suppression:
|
-Nutritional deficiencies: B12 and folate
-Infections: TB, HIV, parvovirus, CMV, EBV -Malignant infiltration -Medication induced: Bactrim, chloramphenicol (An anabiotic) -Aplastic: due to stem cell injury |
|
|
What is the basic pathophysiology and myelodysplastic syndromes?
|
Basically the bone marrow is hypocellular.
|
|
|
What is the difference between myeloproliferative disease versus myelodysplastic syndrome?
|
The bone marrow is hypercellular in myeloproliferative disease as the neoplastic cells can't get out of the bone marrow. The bone marrow is hypocellular in myelodysplasia.
|
|
|
What are three common types of myeloproliferative diseases?
|
1. Chronic myelogenous leukemia (CML)
2. Polycythemia Vera 3. Essential thrombocytosis |
|
|
In what condition is a translocation of chromosome 9 and 22, Philadelphia chromosome seen?
|
Chronic myelogenous leukemia or CML
|
|
|
Hematocrit definition of polycythemia vera?
|
Hematocrit greater than 54 men or greater than 49 in women
|
|
|
Conditions that can cause secondary or reactive thrombocytosis:
|
-Iron deficiency anemia
-Chronic inflammatory condition -Malignancy |
|
|
Platelet definition of essential thrombocytosis?
|
Platelets greater than 600,000. Most patients actually experience hemorrhage due to platelet dysfunction particularly when platelets are greater than 2 million. Symptoms are often relieved with aspirin.
|
|
|
What conditioned to think of when abnormal bleeding is seen in an otherwise healthy person?
|
Idiopathic immune thrombocytopenia Purpura (ITP) until proven otherwise. Remember that this diagnosis is a diagnosis of exclusion of any other possible causes of thrombocytopenia.
|
|
|
NOTE: Gestational thrombocytopenia is not associated with adverse maternal or fetal outcomes. Generally requires no specific intervention. Typically develops in the third trimester.
|
X
|
|
|
List of low molecular weight heparins:
|
-Enoxaparin/Lovenox
-Fondaparinux/Arixtra -Dalteparin/Fragmin |
|
|
Direct factor Xa inhibitors:
|
-Rivaroxaban/Xarelto
-Apixaban/Eliquis -Edixaban/Lixiana |
|
|
Difference in type 1 and type 2 HIT:
|
Type one is not an autoimmune and only causes a transient drop in platelets after starting heparin. It occurs right after starting heparin.
Type two is autoimmune base and typically occurs 5 to 15 days of heparin exposure. typically there is a 50% drop in platelet count. With HIT all heparins including LMWH must be stop including Lovenox, Arixtra and fragmin. |
|
|
Which is safe in renal insufficiency: Lepirudin or Argatroban?
|
Argatroban
|
|
|
What should be thought about in reference to warfarin in the setting of acute HIT?
|
Warfarin should be avoided in early HIT due to associated syndrome of venous limb gangrene and necrosis reflecting it's propensity to decrease protein C levels precipitously in the context of underlying hypercoagulable state/HIT.
|
|
|
What is the most common inherited autosomal dominant bleeding disorder?
|
Von Willebrand disease. Which is due to a dysfunction in primary hemostasis.
|
|
|
Best test to test for von Willebrand disease?
|
VWB factor activity essay. Best tested for when condition clinically silent.
|
|
|
How long to wait after completing a course of anticoagulation to test for hypercoagulable states:
|
Two weeks.
|
|
|
What effect does lupus anticoagulant have on coags?
|
-Prolong PTT
-Mixing study will show presence of factor inhibitors by failure of coagulation profile to correct by the addition of normal plasma. -Russell viper venom test positive. |
|
|
Treatment for disseminated intravascular coagulation (DIC)
|
-FFP if bleeding until significant bleeding has stopped and fibrinogen greater than 100 or
-Low-dose heparin if clotting predominates. |
|
|
Types of congenital Thrombophilias?
|
-Factor V leiden defect/mutation (Most common type)
-Antithrombin III deficiency -Prothrombin factor II gene mutation -Protein C deficiency -Protein S deficiency -Hyperhomocystinemia (only one with primarily arterial thrombosis) |
|
|
Normal homocysteine levels?
|
2 to 9 while fasting. This condition is usually due to B12, folate, or B6 deficiencies.
|
|
|
Describe a DIRECT Coombs' test:
|
The patients RBCs are mixed with laboratory anti-IgE to see if agglutination occurs. If agglutination does NOT occur then the test is positive because the antigens on the patients RBCs surface are already occupied by autoimmune antibodies.
|
|
|
Describe a INDIRECT Coombs' test:
|
The patients sera is mixed in the laboratory with a panel of normal RBCs expressing different unoccupied antigens.
|
|
|
What is monoclonal gammopathy of uncertain significance?
|
Basically it is high total protein with normal or low albumin. This is due to the presence of monoclonal proteins. This condition is defined by the presence of monoclonal proteins in excess in a patient who does not possess clinical or laboratory features of multiple myeloma.
|
|
|
Other test to check for if suspecting B12 deficiency but B12 levels normal?
|
Methylmalonic acid level which should be high, not low if B12 deficient. Note homocystine levels can be elevated in both folate and B12 deficiencies while methylmalonic acid is only elevated and B12 deficiency.
|
|
|
Pernicious anemia causes what?
|
B 12 deficiency. It is an autoimmune process with antibodies against gastric parietal cells and intrinsic factor leading to vitamin B 12 malabsorption.
|
|
|
What is the biggest viral threat with blood transfusion?
|
Hepatitis B over HIV and hepatitis C because PCR is only available for HIV and hepatitis C, not hepatitis B.
|
|
|
What is the pathophysiology of blood group transfusion issues?
|
You basically produce antibodies to the blood group you don't have. So if your blood type is A you will produce antibodies to type B.
|
|
|
Universal blood type donor of RBCs:
|
Blood group O
|
|
|
Universal donor of plasma:
|
Blood group or blood type AB.
|
|
|
Common complications of RBC transfusion:
|
-Thrombocytopenia. There is approximately 50% reduction in platelet count with massive transfusion.
-Hypocalcemia. Due to calcium fixation with basic components of transfusion. -Metabolic alkalosis. |
|
|
What are the types of RBC antigens:
|
Major: ABO
Minor: Rh Unlike ABO system, patients do not have naturally occurring anti-Rh antibodies. |
|
|
How much should one unit of platelets increased platelet count by?
|
10,000
|
|
|
Causes of falsely positive fecal occult blood test:
|
-Consumption of red meat
-Foods high in perioxidase (turnips, pineapple, banana, horseradish) -Vitamin C -Aspirin, nonsteroidals due to G.I. bleed |
|
|
What conditioned to think about with elevated PSA in a female?
|
Think malignancy of Skene's gland. It is the female counterpart to the male prostate.
|
|
|
What conditioned to think about with signs of: face plethora, shortness of breath, facial edema, JVD, strider, and engorged collaterals on the chest wall?
|
Superior vena cava syndrome. First step is stable mediastinoscopy with biopsy to decide on form of treatment.
|
|
|
ANC count that defines neutropenia:
|
Absolute neutrophil count less than 1000 but clinically significant with absolute neutrophil count lesson 500.
|
|
|
How to calculate absolute neutrophil count:
|
Multiply neutrophil % by WBC count
|
|
|
What conditioned to think about if multiple meningiomas found?
|
Neurofibromatosis type 2
|
|
|
Three common types of melanomas:
|
1. Superficial spreading. Most common type accounting for 70% of melanomas. Initial growth phase is horizontal.
2. Nodular melanoma -accounting for 15%. It's initial growth phase is vertical, therefore more events that diagnosis. 3. Acral lentiginous - accounting for a percent. Most common and blacks and persons of color. Occurring on digits, nailbed and feet. |
|
|
Types of non-melanoma skin cancer:
|
1. Basal cell. Accounting for 80%. These cancersrRely metastasize. Waxy, semitranslucent nodule with central depression.
2. Squamous cell. Counting for 20%. Mets occur in 2-5% of cases. |
|
|
Which long cancer type is more sensitive to chemotherapy and radiation?
|
Small cell. But cure rate is nevertheless lower than non-small cell. almost all have disseminated disease on initial presentation. These cancers metastasize early to bone marrow, liver, and brain.
|
|
|
Paraneoplastic syndromes associated with small cell lung cancer:
|
1. SIADH
2. Eaten Lambert syndrome: Diffuse muscle weakness with sparing a facial and ocular muscles. Unlike myasthenia gratis, motor strength improves with repetitive muscle stimulation. 3. Cushing syndromedue to ACTH production. |
|
|
Paraneoplastic syndrome seen in none small cell lung cancer:
|
1. Pancoast syndrome: tumor is evolving the upper lobes with infiltration of brachioplexus producing sensory/motor findings in the upper extremities (Lower brachial plexopathy and Horner's)
2. Superior vena cava syndrome 3. Hypercalcemia due to PTH like hormone production. Remember endogenous PTH will be suppressed. |
|
|
Cancers that produce PTH like hormone:
|
1. Squamous cell lung cancer
2. Renal cell carcinoma |
|
|
Health risks associated with tamoxifen therapy:
|
Uterine cancer and DVT. Patients on this medication should have routine pelvic exams to screen for uterine cancer.
|
|
|
Describe normal and abnormal PSA values:
|
0-4: okay
4-10: can be seen in both BPH and cancer Greater than 10: usually indicates cancer Patient should be referred to urologist when PSA greater than 4. |
|
|
How is staging done in ovarian carcinoma?
|
Through an exploratory laparotomy with bilateral oophorectomy, hysterectomy, and omentectomy.
|
|
|
At what age should in large lymph nodes be biopsied?
|
Over 40 biopsy, below 40 observation unless convincing risk factors.
|
|
|
What are the five types of lymphoid tumors:
|
1. Chronic leukemia
2. Acute leukemia 3. Lymphoma 4. Hodgkin's disease 5. Myeloma |
|
|
Which virus is related to lymphoma?
|
EBV
|
|
|
What is the primary difference between Hodgkins and non-Hodgkin's lymphoma?
|
The main difference is method of spread.
-Hotchkins spreads contiguous from one lymph node to another -Non-Hodgkin spreads hematogenously |
|
|
Origin of most Hodgkin's lymphoma?
|
Cervical lymph nodes and then's spreading contiguously two other lymph nodes. Non-Hodgkin's is a more diffuse disease. Because of his motives
|
|
|
Which lymphoma: non-Hodgkin's or hodgkin's is most sensitive to radiation?
|
Non-Hodgkin's is very radio sensitive.
|
|
|
Most common type of leukemia:
|
CLL -chronic lymphocytic leukemia
|
|
|
Which leukemia is seen in children?
|
ALL. ALL seen in adults has poor prognosis.
|
|
|
Auer rods are seen in which onc condition?
|
Acute myelogenous leukemia (AML)
|
|
|
What condition has the triad of: monoclonal gammopathy, lytic bone lesions, greater than 10% marrow plasma cells
|
Multiple myeloma.
Also you find elevated total serum protein with normal or low albumin. |
|
|
What are the three main types of amyloidosis:
|
1. AL amloid: The L stands for light chain. This is considered primary Amyloid. Seen in multiple myeloma.
2. Secondary Amyloid: seeing with chronic inflammatory conditions such as rheumatoid arthritis and ankylosing spondylitis. 3. HD associated Amyloid: Where beta-2 microglobulin accumulates |
|
|
Which immunoglobulin deficiency should be considered in any patient with a history of anaphylaxis during blood transfusion?
|
IgA deficiency. If this patient receives blood transfusions in the future they should be washed erythrocytes.
|
|
|
All-trans-retinoic acid is a treatment for what type of leukemia?
|
Acute promyelocytic leukemia (APL)
|
|
|
Treatment of extensive and/or progressive superficial venous thrombosis?
|
Anticoagulation with INR goal of 2 to 3. If clot mild or moderate considerations of anticoagulation versus nonsteroidals for superficial venous DVTs should be made.
|
|
|
Principal laboratory findings in antiphospholipid antibody syndrome:
|
Positive dilute Russell viper venom time.
|
|
|
Heparin or Coumadin is a contraindication during pregnancy?
|
Only Coumadin. Heparins including low molecular weight heparins is acceptable during pregnancy.
|
|
|
If "blister or bite cells" or seen on peripheral smear what conditioned to think of?
|
Glucose 6 phosphate dehydrogenase deficiency
|
|
|
Hemophilia A causes what clotting factors to be prolonged?
|
PTT
|
|
|
Treatment of ITP if platelet count less than 30,000 or active bleeding:
|
Steroids or thrombopoietin-mimetic agent therapy.
|
|
|
What should be done if a patient previously therapeutic on Coumadin within the first month of a clot become subtherapeutic?
|
Reinitiate low molecular weight heparin and an increased dose of warfarin. The risk of recurrence during subtherapeutic state is 40% in the first month.
|
|
|
Itching often worse after bathing suggest what condition:
|
Polycythemia vera
|
|
|
General treatment for polycythemia vera:
|
-Therapeutic phlebotomy and low dose aspirin
-Hydroxyurea for older patients who are symptomatic cannot tolerate phlebotomy or aspirin |
|
|
Gamma radiation of RBCs prevents what?
|
Graft versus host disease
|
|
|
Folate deficiency causes methylmalonic acid elevation and or homocystine elevation?
|
Only homocysteine elevation. Also no neurological deficits as seen in B12 deficiency.
|
|
|
What causes pseudo-thrombocytopenia?
|
Platelet clumping which can be seen on peripheral smear. this is a laboratory artifact. This can be confirmed by repeating the platelet count in a tube containing citrate or Heparin as the anticoagulant.
|
|
|
Microcytic anemia associated with normal or slightly increased erythrocyte count is characteristic of what condition:
|
Beta-thalassemia.
Iron deficiency anemia typically has reduce erythrocyte counts. |
|
|
Test to diagnose chronic myeloid leukemia (CML)?
|
FISH assay for t(9;22): florescence in situ hybridization
|
|
|
Abdominal fat pad aspirate is a test for what condition?
|
AL Amyloidosis
|
|
|
Percent of clonal plasma cells on the bone marrow biopsy which defines multiple myeloma:
|
10% or more. Less than 10% would be consistent with monoclonal gammopathy of unknown significance.
|
|
|
Characteristics of parvovirus B19 infection:
|
-Recent sick contacts
-Fever and arthralgia -very low retic count |
|
|
What conditioned to think of when you see: scallop tongue/macroglossia, hepatomegaly, nephrotic syndrome, and peripheral neuropathy?
|
AL Amyloidosis
|
|
|
Is there a positive or negative Coombs' test in warm autoimmune hemolytic anemia?
|
Positive
|
|
|
Blood test to diagnose polycythemia vera?
|
JAK2 V617F analysis
|
|
|
BCR-ABL gene analysis is a test for what condition?
|
Philadelphia chromosome. Chronic myelogenous leukemia.
|
|
|
Blood type to be give in an emergent transfusion if ABO incompatibility issues cannot be worked out?
|
O negative
|
|
|
What can cause hypocalcemia with plasma exchange?
|
The Citrate which is used as an anticoagulant.
|
|
|
What factor deficiency is hemophilia A?
|
Factor VIII (8) deficiency |
|
|
What factor deficiency is hemophilia B?
|
IX (9) deficiency
|
|
|
Does factor V Leiden require life long anticoagulation?
|
No. This condition is associated with a significant risk for initial VTE but it is not associated with a significant risk of recurrent VTE.
|
|
|
What multiple myeloma medication is associated with DVT and PE?
|
Revlimid (Lenalidomide)
|
|
|
How is unfractionated heparin cleared from the body?
|
The reticuloendothelial system
|
|
|
What is the definition of gestational thrombocytopenia?
|
Thrombocytopenia with platelet counts higher than 50,000 and typically occurring in the third trimester. There are no maternal or fetal complications when platelet count equal to or greater than 50,000.
|
|
|
What is the absolute neutrophil count seen in congenital asymptomatic neutropenia?
|
Between 1000 and 1500. This condition is seen and certain ethnic populations including blacks, Jews, and a Arabs.
|
|
|
Highly oxidizing medications which can trigger G6PD hemolysis:
|
-Bactrim
-Dapsone -Primaquine |
|
|
What conditioned to think about when you see on peripheral smear agglutination of erythrocytes and unusually high MCV?
|
Cold agglutination disease
|
|
|
What disease to think about when you see: unprovoked venus thrombosis at unusual locations, hemolytic anemia, and mild to moderate pancytopenia?
|
Paroxysmal nocturnal hemoglobinuria. It is diagnosed with flow cytometry.
|
|
|
Name a cytoreductive agent:
|
Hydroxyurea
|
|
|
What does red blood cell distribution width (RDW) measure?
|
It measures variation in size of Rbcs.
|
|
|
Who gets IM or IV iron?
|
Reserved for patients:
-Receiving dialysis -For patients who cannot absorb or tolerate oral iron |
|
|
Viral infections which can cause aplastic anemia:
|
-Parvovirus B 19
-EBV -CMV |
|
|
Reversal agent for heparins:
|
Protamine. Note low molecular weight heparin and such as Lovenox is only 60% reversible were Protamine. Arixtra is not reversed and all my protamine.
|
|
|
What condition to consider with: mild anemia, microcytosis, hypochromia, target cells, and normal hemoglobin electrophoresis?
|
Alpha thalassemia trait. No treatment is necessary for this condition.
|
|
|
What is the pathophysiology thalassemia disease?
|
-Ineffective erythropoiesis
-Intravascular hemolysis caused by precipitation of excess insoluble globin chain -Decreased hemoglobin production |
|
|
What is the beta thalassemia minor and alpha thalassemia trait?
|
Normal hemoglobin electrophoresis in Alpha thalassemia trait. Positive hemoglobin electrophoresis in beta thalassemia minor for Hb A2
|
|
|
Named the myeloproliferative disorders that test positive for JAK2 V617F gene mutation:
|
1. Polycythemia vera
2. Essential thrombocytosis |
|
|
Treatment of myelodysplastic syndrome:
|
Azacitidine
|
|
|
What's the problem with Meperidine?
|
Short half-life and tendency to redo seizure threshold secondary to accumulation of metabolites. additionally it is no more effective than morphine IV or Hydromorphone.
|
|
|
What is the long-term treatment of choice for VTE in patients with history of active cancer?
|
Low molecular weight heparin instead of Coumadin.
|
|
|
What conditioned to think about with these five findings: thrombocytopenia, microangiopathic hemolytic anemia (Schistocytes on peripheral smear), neurological deficits, kidney impairment, and fever?
|
Thrombotic thrombocytopenic Purpura (TTP). Peripheral smear is key to look for evidence of microangiopathic hemolytic anemia showing schistocytes. Treat TTP with plasma exchange.
|
|
|
When to start patients on the chemotherapy (Docetaxel) with Prostate cancer?
|
In patients with hormone refractory metastatic prostate cancer.
|
|
|
What is the treatment for prostate cancer with the Gleason score less than 8 and a PSA less than 20?
|
Usually radiation alone. |
|
|
When should the patient get prophylactic brain radiation and small cell lung cancer?
|
Obviously if your initial staging was negative for brain Mets and they have responded positively to chemo/radiation.
|
|
|
Treatment of hormone receptor positive breast cancer with history of DVT?
|
Ovarian ablation. Tamoxifen is contraindicated because of history of previous DVT.
|
|
|
What is the mechanism of action of tamoxifen?
|
Estrogen receptor inhibitor.
|
|
|
NOTE: aromatase inhibitors are only indicated in postmenopausal patients because they cause ovarian stimulation.
|
X
|
|
|
Which colon cancer chemotherapeutic agent is known to cause intestinal perforation?
|
Bevacizumab. This medication is also well known to cause hypertension.
|
|
|
The type of lymphoma usually presenting with advanced stage disease involving extranodal sites including: bowel, peripheral blood, and bone marrow.
|
Mantle cell lymphoma. Diagnosis confirmed by over expression of cyclin D1.
|
|
|
What is the definition of cancer of unknown primary (CUP):
|
When a tumor is detected at one more typical metastatic sites and routine evaluation fails to define a primary site. The tumor should be treated exactly how you would treat the tumor if you knew primary site.
|
|
|
What test should you order in patients with metastatic adenocarcinoma, non-small cell lung cancer before initiating palliative chemotherapy?
|
Epidermal growth factor receptor (EGFR) gene mutation tumor analysis. If positive for this mutation medications that target the EGFR receptor may dramatically improve response rate and median survival.
|
|
|
What is the best preparation of RBCs for transfusion to be given to patients with sickle cell disease?
|
RBCs that are phenotypically matched. |
|
|
When to do brachytherapy (radioactive seed implants) in prostate cancer:
|
It is an option for patients at low or average risk: Gleason score less than 8 and PSA less than 20
|
|
|
What is considered a high Gleason score?
|
8 to 10
|
|
|
What syndrome to consider with the symptoms of the: diarrhea, Flushing, and wheezing?
|
Carcinoid syndrome. Check blood serotonin levels.
|
|
|
What is the principal treatment for melanoma?
|
Surgery.
|
|
|
Poor prognostic features of melanoma:
|
-thickness greater Than 0.7 mm
-Positive deep margins (within 1 cm margin) -Lymphovascular invasion Do sentinel node biopsy if thickness greater than 1 mm. |
|
|
NOTE: squamous cell cancers of the head and neck can occur in patients without risk factors, presumably due to infection with EBV for HPV.
|
X
|
|
|
Next step/test if incidental mass seen on CT in kidney?
|
Renal ultrasound to evaluate for cyst or solid.
|
|
|
What is the first thing before treatment that needs to be done in superior vena cava syndrome?
|
Tissue biopsy typically by mediastinoscopy
|
|
|
How do spherocytes look? |
RBCs that have lost their central pallor. |
|
|
How do hypersegmented polymorphic nuclear cells look and what condition are they found in?
|
B 12 deficiency.
|
|
|
The best agent for quick warfarin reversal?
|
PCC: prothrombin complex concentrate. PCC is better than FFP because it can be reconstituted in minutes versus preparation of FFP taking several hours.
|
|
|
What is the treatment of asymptomatic follicular lymphoma?
|
Watchful waiting. Treatment is not starting until symptoms arise. Follicular lymphoma is the second most common type of non-Hodgkin's lymphoma.
|
|
|
When to start androgen deprivation hormonal therapy in prostate cancer?
|
Only in patients with high risk localized disease or patients with locally advanced disease.
|
|
|
What hemoglobin level should a patient with sickle cell disease be preoperatively transfused to to reduce risk of acute chest syndrome?
|
Hemoglobin of 10
|
|
|
What is the treatment for stage 4 non-small cell lung cancer?
|
Chemo alone
|
|
|
What is the treatment for stage 3 unresectable non-small cell lung cancer?
|
Chemo and radiation
|
|
|
Describe the bleeding patterns of bladder cancer versus kidney cancer:
|
Bladder cancer commonly presents with bleeding, typically throughout micturition.
Kidney cancer less commonly presents with bleeding. |
|
|
What is the sentinel lymph node?
|
It is the first draining lymph node which is a Denna five by injecting blue dye and radioactive colloid into the tumor site.
|
|
|
NOTE: Sentinel lymph node evaluation is now the standard of care with breast cancer instead of axillary node dissection.
|
X
|
|
|
What is the treatment for hairy cell leukemia?
|
Cladribine - a purine analog. Hairy cell leukemia is a rare form of leukemia that is highly curable if treated early enough. Often bone marrow aspirate is "dry" with hairy cells on pathology.
|
|
|
Is radiation commonly used in colon cancer or rectal cancer or both?
|
Radiation is not commonly used in colon cancer due to difficulty of distinguishing small bowel from radiation field. Radiation although is commonly used in rectal cancer particular stage 2 and stage 3 do
Ur to ease of distinguishing small bowel from radiation field. |
|
|
What tumor markers should be checked in all patients presenting with testicular mass?
|
-Alpha-fetoprotein: Elevation always indicates the tumor has nonseminomatous components -beta hCG: Elevation can represent seminomatous or nonseminomatous tumors
|
|
|
Treatment for diffuse large B cell lymphoma: |
R-CHOP for six cycles |
|
|
How do spherocytes look?
|
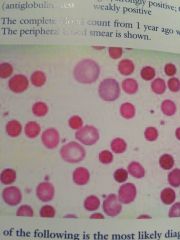
Rbcs that have lost their central pallor.
|
|
|
How do hypersegmented polymorphic nuclear cells look and what condition are they found in?
|
B 12 deficiency.
|
|
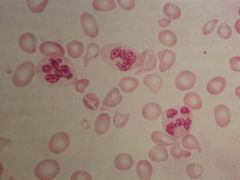
A picture of schistocytes
|
X
|
|
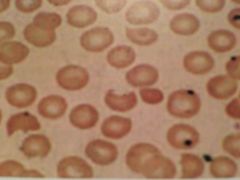
The picture of bite cells:
|
X
|
|

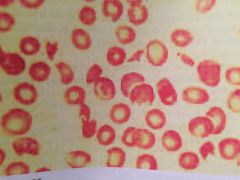
A picture of target cells:
|
X
|
|
|
What is the treatment for low-grade, stage 1 ovarian cancer?
|
Surgical removal of the ovaries, uterus, momentum, and lymph node sampling. No indication for adjuvant chemotherapy.
|
|
|
Management of high-risk patients for breast cancer who have previously received radiation or BRCA positive:
|
Yearly mammography and breast MRI
|
|
|
Treatment of neutropenic fever:
|
-Start with broad-spectrum anabiotic such as Zosyn OR cefepime
-Add empiric antifungal if still febrile after 4 to 7 days of broad-spectrum anabiotic's -Viral infection not typical cause of infection in patients with the febrile neutropenia; therefore empiric therapy not indicated. |
|
|
What type of breast cancer is tamoxifen used for:
|
Estrogen receptor positive
|
|
|
The best treatment for metastatic melanoma to the brain?
|
Surgical resection if patient symptomatic. stereotactic radiosurgery can also work but not available in most centers.
|
|
|
What is the follow up on bladder cancer after resection?
|
Cystoscopy and urine cytology every three months.
|
|
|
What type of lymphoma is associated with tumor lysis syndrome?
|
Burkitt lymphoma
|
|
|
Standard treatment for Hodgkin's lymphoma:
|
Chemo (ABVD) and radiation. Radiation alone without chemo therapy can be used in localized disease. Note regardless of stage at presentation, Hodgkin's lymphoma is highly curable. Common findings include palpable lymphadenopathy or a mediastinal mass.
|
|
|
At what age does acute lymphoblastic leukemia (ALL) present in adults?
|
Highest incidence in the seventh decade of life.
|
|
|
What conditioned to think about with: lymphocytosis, neutropenia, anemia, thrombocytopenia, lymphadenopathy, and hepatosplenomegaly?
|
Acute leukemia
|
|
|
Beta-2-microglobin measurements are taken and what condition?
|
CLL
|
|
|
What type of breast cancer is chemotherapy not indicated in?
|
Ductile carcinoma in situ
|
|
|
What type of medication is Anadtrazole?
|
Aromatase inhibitor. And estrogen production blocker. Should only be using women post menopausal. They are associated with superior disease-free survival as compared to tamoxifen. Additionally they are not associated with DVT although osteopenia can be seen.
|
|
|
What is postoperative surveillance for stage III Colon cancer:
|
-Physical examination and CEA level every 3 to 6 months
-Chest/abdomen/pelvic CT annually for 3 to 5 years -Colonoscopy when you're after resection and then repeat at three to five-year intervals |
|
|
Clinical presentation of alpha-thalassemia minor (trait): |
Mild microcytosis without significant anemia or hemolysis. Normal electrophoresis. |
|
|
Clinical presentation of beta-thalessemia minor (trait): |
Mild anemia and mild hemolysis. Abnormal electrophoresis showing increase in Hb A2. |
|
|
Clinical presentation of beta-thalessemia major: |
Transfusion dependent. |
|
|
What are the inherited disorders of hemostasis: |
-Von Willebrand disease -Hemophilias (factor 8 & 9 deficiences) -ITP -TTP |
|
|
Pathophysiology of Von Wille dz: |
-The Von Wille factor attacheds platelets to blood walls -It is a carrier protein that delivers factor 8 to the site of clot formation (factor 8 can not circulate unless it is attached to VWB. |
|
|
Difference in Hemophilia A and VWB disease: |
They both have an impact on factor 8 but VWB factor activity assay is normal in hemophilia A. They both prolong PTT because of factor 8 involvement. |
|
|
List of hemolytic anemias: |
-Hereditary spherocytosis -G6PD deficiency -Paroxysmal nocturnal hemoglobinuria -Warm autoimmune anemia -Cold autoimmune hemolytic anemia -Drug-induced |
|
|
List hemoglobinopathy anemias: |
-Sickle-cell anemia -Thalassemias |
|
|
List of bone marrow based anemias: |
-Aplastic anemia -Myelodysplastic syndrome (MDS) -Siderplastic anemia |
|
|
List of myeloproliferative Diseases: |
-CML -Polycythmia vera -Essential thrombocytosis -Essential Myelofibrosis (teardrop cells) |
|
|
List of inherited disorders of hemostasis: |
-Von Willebrand disease -Hemophilia A -Hemophilia B |
|
|
List of thronbotic microangiopathies: |
-Henoch-Shonlein Purpura -Thrombotic thrombocytopenic purpura (TTP) -Hemolytic uremic syndrome (HUS) |
|
|
Lymph node based cancers: |
The lymphomas: -Hodgkin's -Non-Hodgkin's |

