![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
- 3rd side (hint)
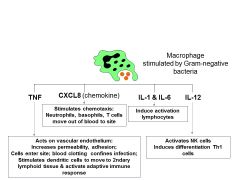
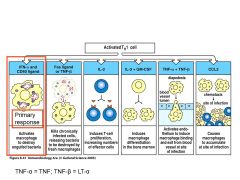
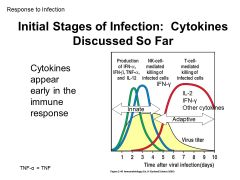
LOOK CLOSELY: This group of cytokines have a major role in what process of the body? |
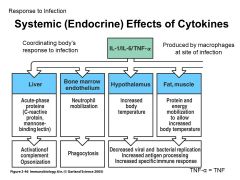
Pro-inflammatory cytokines! (early reponses to infection)
Can also cause SYSTEMIC effects as seen here! Mobilize to get an immune response |
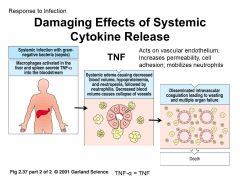
MASSIVE MASSIVE INFLAMMATION |
|
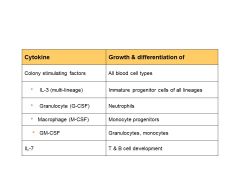
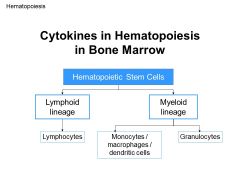
LOOK CLOSELY: This group of cytokines have a major role in what process of the body? |
CYTOKINES FOR HEMATOPOESIS in immune cells differentiation |
|
|
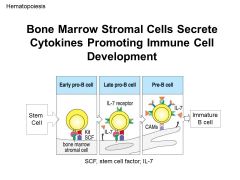
LOOK CLOSELY: What do all these cytokines have in common? This group of cytokines have a major role in what process of the body? |
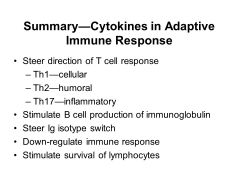
ADAPTIVE IMMUNE RESPONSE... helps with T1 and T2 helper cells |
|
|
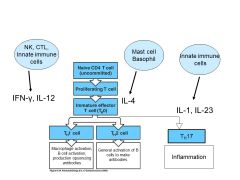
LOOK CLOSELY: Whats the theme here? What do all these cytokines have in common? |
Cytokines synthesed by TH1 cells... focused on activation of macrophages to kill intracellular pathogens. |
|
|
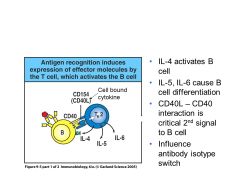
LOOK CLOSELY: What do all these cytokines have in common? |
Cytokines secreted by TH2 helper cell help ANTYIBODY production... increases B cell proliferation. Fun fact: Cytokines secreted by Th2 cells known as "ANTI-INFLAMMITORY CYTOKINES" |
|
|
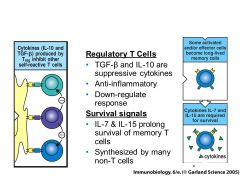
LOOK CLOSELY: What do all these cytokines have in common? What process in the body makes them so important |
Important for IMMUNE REGULATION IL-10 and TGF-beta= STOP SIGNS IL-7 and IL-15= Long Term memory key for turning off immune response |
|
|
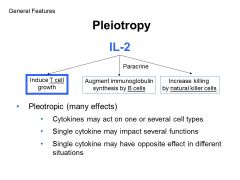
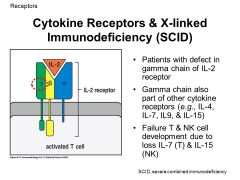
One cytokine can have many different effects... so what sort of chaos might happen if the IL-2 receptor were somehow mutated? |
So FCuked!! cant mount a sufficient immune response |
Mutation of the gamma chain of IL-2 receptor also affects receptors for IL-4, IL-7, IL-9, IL-15. The gene for this “common gamma chain” is encoded on the X chromosome so males are most commonly affected. The result is a decrease in NK and T cells and nonfunctional B cells due to lack of T cell help. The deficiency is more severe than an IL-2 deficiency because multiple cytokines are affected. |
|
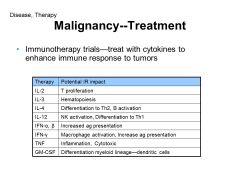
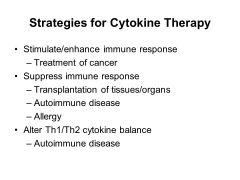
Looking at this list, which cytokines therapies could be used for treatment of malignancy, autoimmune diease, allergy and transplantation?
When would you want to ENHANCE immune response and when would you want to SUPRESS immune response? How could you do this? |
|
|
|
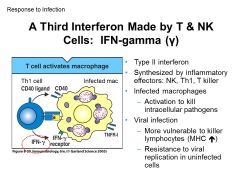
Interferons (IFN) help protect against viral infections. Type 1 = alpha and beta Type 2= gamma Which one is part of innate repsonse (made by most cells) and which one is more adaptive response (made by NK, Th1, and killer Tcells)? |
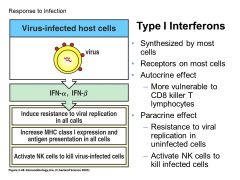
Type I (alpha/beta)= Innate Type II (gamma)= KILLER/ adaptive |
|
|
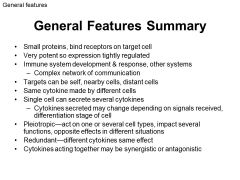
What makes cytokines so AWESOME?!?! Can you think of examples of each? |
different cells, same cytokine= TGF-beta [monocytes, tcells, chondrocytes] same cell, different cytokines= macrophages [TNF, CXCL8, IL1,IL6,IL12)] Autocrine- T cell secreting IL2 Paracrine- INFgamma from Tcell activates macrpophage pleiotropy - IL-2 [Tcell growth, Bcell antibody synthesis, increase NK cells] Redundancy- IL-2, IL4, IL7, IL15 all T cell growth factors Synergy- CD40 and INFgamma activating macrophage Antagonisim- IL2 promotes growth... TGFbeta inhibits T cell growth |
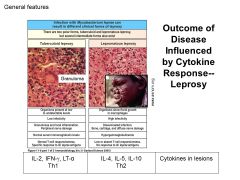
Low yield, but just cool what a difference cytokines can make |
|
|
What about the JAK/STAT pathway is so snazzy for cytokines? |
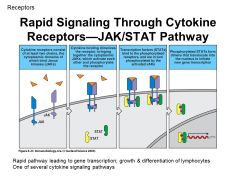
RAPID RESPONSE TO CYTOKINES |
|
|
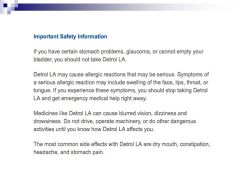
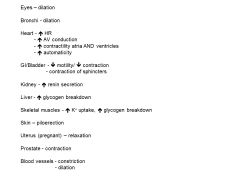
What should these side effects SCREAM to you? |
CNS drugs= ANTI-muscarinic ACTIVITY
(aka anti-cholinergic side effects) |

|
|
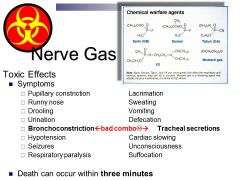
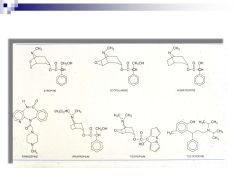
Might save life during apocalypse... why is ATROPINE and PRALIDOXIME work as an antidote for nerve gas/ chemical warefare? (also works for poising from insecticides/ organophosphates?) |
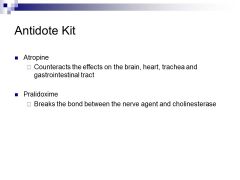
These drugs are really POWERFUL Acholinestgerase inhibitors (meaning they UP and exacerbate the cholinergic effects (PNS) on the body)
Atropine is a powerful (ANTI-CHOLINERGIC) so it will help remove side effects (via comp. inhibition/ anatagonist) of a system overwhelmed with acetylecholine
pralidoxime- breaks up [nearly] irreversible bond between nerve agent phosphate and cholinesterase |
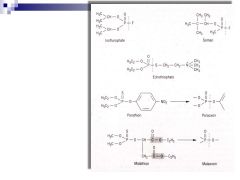
Other irreversible Ach inhibitors (indirect cholinergics) |
|
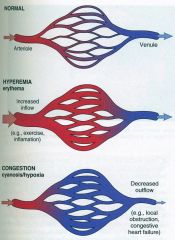
Whats the difference between HYPEREMIA and CONJESTION? |
HYPEREMIA
CONGESTION
|
|
|
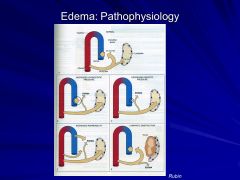
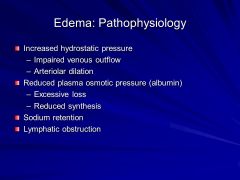
What are 4 conditions that can cause edema? |
|
|
|

How would you describe the difference between petichiae and purpura? what causes difference b/w these two |
- Defects in primary hemostasis (platelet defects) often present with petechiae in the skin or mucosal surfaces. |
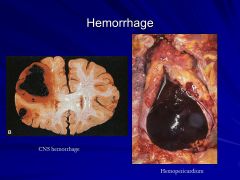
o Hematoma: Accumulation of blood within a tissue |
|
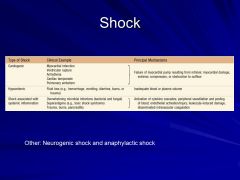
Be careful... burns can cause both hypovolemic shock or shock associated with systemic inflammation (formerly "septic shock"). What is the difference between these two types? |
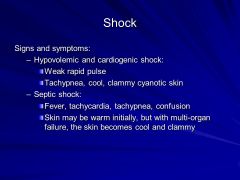
|
What do they have in common. |
|
|
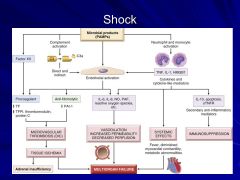
What are some complications of shock? |

|
|
|

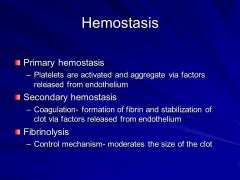
3 things make up hemostasis (vascular wall, platelets, and coag cascade) What are the events of normal hemnostasis after injury? |
1. Vasoconstriction: 2. Platelet activation 3. platelet aggregation 4. activation of coag cascade 5. stabilization of platelet plug |
|
|
|
Endothelium very important. What are some ANTITHROMBITIC PROPERTIES, and what are PROTHROMBITIC PROPERTIES? WHy do we give t-PA to people that are having a stroke? |
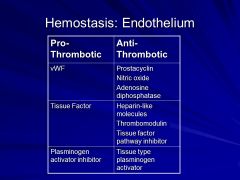
Antiplatelet- (1hemostasis) Anticoagulant- (2dary hemostasis) Fibrinolytic effects |
Antithrombotic Properties |
|
|
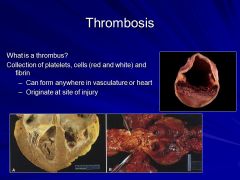
Thrombus: Formation of a blood clot in uninjured vasculature or in a vessel with minor injury (or a pathologic disease).
What are the three things that can lead to a thrombus? (VIRCHOWS TRIAD) |
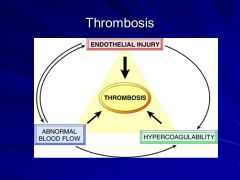
Factors involved in thrombosis: VIRCHOW TRIAD |
Endothelial Injury
|
|
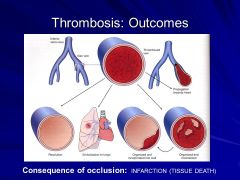
What is the difference between venous, arterial and mural thrombi.... what are complications of each? |
Arterial Thrombus Venous Thrombus Mural Thrombus |
|
|
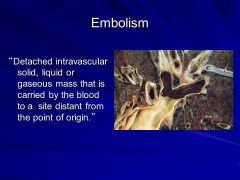
The 5 different types of embolisims: Thromboembolisim--> pulmonary embolus, systemic thromboembolisim, air, fat, amniotic fluid. Which ones are the scariest? What are the complications of each? What is most common? Which one can happen with SEVERE ortho trauma? Which ones could cause a stroke? |
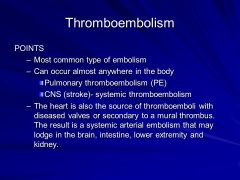
difference in stoke... one may be athlerosclerosis... one may be from the heart (embolisim breaking off) |
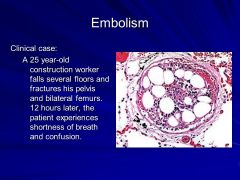
Thromboembolism: Pulmonary Embolus Systemic thromboembolism Fat Embolus Air Embolus Amniotic Fluid Embolus |
|

What are classic examples of RED infarcts? White infarcts? |
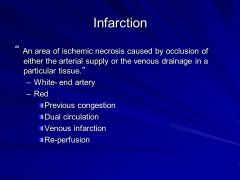
Red: So-called because they are hemorrhagic and typically occur in the following settings. White: Occur in organs with end-artery circulation (heart, spleen, kidney) *Most infarcts (either type) tend to be wedge-shaped with a hyperemic border and slightly irregular outlines. |
dominant feature is necrosis- in all areas this is COAGULATIVE NECROSIS... [EXPECT FOR THE BRAIN!!!! BRAIN IS LIQUIFACTIVE NECROSIS] |
|
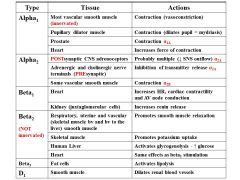
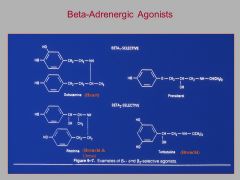
Which drug (norepi or epi) are selective for everything EXCEPT B2 RECEPTORS!! ? What does this mean for the body clinically |
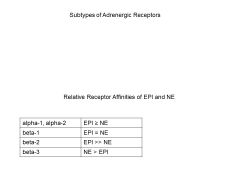
Low does of epi, get relaxation |
|
|
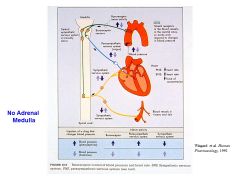
WHat the eff is going on here? |
no idea |
|
|
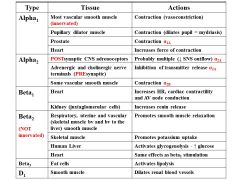
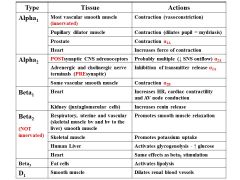
What types of G proteins do all of these receptors have.... what is the ultimate result? |

|
|
|
|
Why are catecholamines ineffective as an oral dose? Why is it always with a needle?? ow |
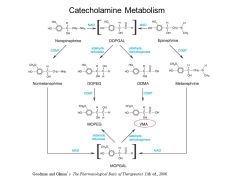
The location of COMT is mainly extraneuronal, (gut, liver, kidney, brain) this renders catecholamines ineffective oraly, since they are METABOLIZED before absorption even occurs |
|
|
|
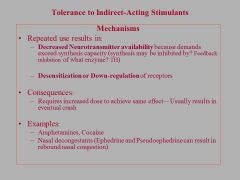
Why is Adderall (amphetamines) so powerful in increasing release of catcecholamines? What does it do extra? |
|
|
|
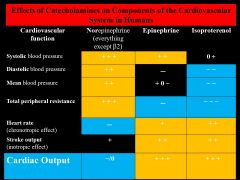
Why is NOREPINEPHRINE the only drug where total peripheral resistance goes UP instead of down? |
norepi (at physiologic levels) can't activate beta-2 receptors in the body! |
|
|
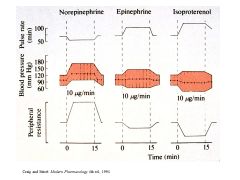
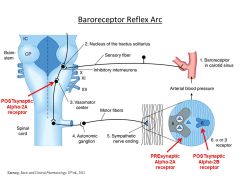
What the hell is going on at norepi here? |
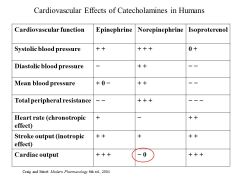
Increase in CONTRACTABILITY of heart, INCREASE in SV but causes HR to go DOWN so NO CHANGE IN CARDIAC OUTPUT
(Does not involve medulla, all neurally mediated compensation mechanisims happen, baroreceptor reflex engaged) |
|
|
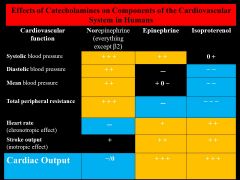
In the above table, would the presence of ATROPINE change the effects of NE on cardiac output? How? By what mechanisim? |
Yes! By blocking muscarinic receptors, atropine would block baro-receptor induced vagus stimulation and would therefore increase the heart rate, therefore cardiac output would increase. What about with epi? |
Norepinephrine – stimulates alpha-1, alpha-2 and beta-1>>> beta2) |
|
What are therapeutic effects of direct adrenergenic agonists? When would this be useful? |
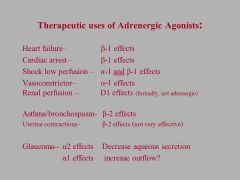
|
|

