![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
176 Cards in this Set
- Front
- Back
|
What are the three general principles of tooth preparation?
|
- biologic
- mechanical - esthetic |
|
|
What are the BIOLOGIC considerations for tooth preparation?
|
1) Prevention of damage during tooth prep
- adjacent teeth - soft tissues - pulp (tempt, chemical, bacterial) 2) Conservation of Tooth Structure - thickness of dentin inversely proportional to pulp response 3) Considerations affecting future dental health - axial reduction - overcontoured margins lead to ging. inflammation - max overcontour is 1mm - margin placement (supragingival best) - margin adaptation (junction vulnerable to recurrent decay - cement dissolution, inherent roughness) - occlusal reduction consideration (functional cusp bevel, 1.5 mm clearance, parallels triangular ridges) - preventing tooth fractures / cuspal protection |
|
|
What are the justifications for placing a margin SUBGINGIVALLY?
|
- caries
- restorations - retention - esthetics - root sensitivity - alteration of axial contour - fracture - erosion / abrasion |
|
|
What is the approximate height of the BIOLOGIC WIDTH?
|
2.0 mm
|
|
|
What is the height of the JUNCTIONAL EPITHELIUM?
|
0.97mm
|
|
|
What is the height of the CONNECTIVE TISSUE ATTACHMENT TO BONE?
|
1.07mm
|
|
|
BIOLOGIC WIDTH = ?
|
Junctional epithelium + connective tissue attachment to bone
|
|
|
What is the width of explorer tip?
|
0.230 mm
|
|
|
What is the average gap between CROWN and TOOTH?
|
0.070mm
|
|
|
What factors affect marginal adaptation?
|
- marginal design
- cement thickness - impression accuracy and lab procedures |
|
|
What is the regular range of cement thickness?
|
25-50 microns
|
|
|
What is the thickness of ZINC PHOSPHATE cement?
|
25 microns
|
|
|
What is the thickness of ZINC POLYCARBONATE and GIC cement?
|
< 25 microns
|
|
|
What is the thickness of COMPOSITE / ADHESIVE resins?
|
> 25 microns
|
|
|
What are the MECHANICAL CONSIDERATIONS for tooth preparation?
|
RESISTANCE FORM - lateral forces displace restoration by rotation around gingival margin
RETENTION FORM - length, taper, circumference FACTORS AFFECTING RETENTION - magnitude of the dislodging forces/ geometry |
|
|
What are the factors that affect RETENTION of a restoration?
|
- magnitude of the dislodging forces (sticky foods, bruxer habits)
- Geometry of tooth preparation - most cements non-adhesive |
|
|
What is the IDEAL taper?
|
6-10 degrees TOC
|
|
|
What is the ACTUAL TAPER that is usually achieved?
|
12.2 - 27 degrees
10-20' practically |
|
|
What is the minimum height of prepared tooth for PREMOLAR?
|
3mm minimum
|
|
|
What is the minimum height of prepared tooth structure for MOLARS?
|
4mm minimum
|
|
|
What can be done for teeth that do not meet minimum prepared tooth height criteria?
|
Modified with grooves / boxes
|
|
|
What are some importants things in ESTHETIC CONSIDERATIONS?
|
- Restoration type (metal, all ceramic, PFM)
- Margin design and location |
|
|
What is ANTE'S RULE?
|
The combined pericemental area of the abutment teeth should be equal to or greater than the pericemental area of the teeth being replaced
|
|
|
What are the two major problems that seriously impede fabrication of sound restorations?
|
- poor impressions of the gingival margins (primarily due to lack of hemorrhage control)
- inadequate reduction of tooth structure |
|
|
PROBLEM: Poor impressions and hemorrhage.
|
SOLUTION:
Poor impressions: Proper injecting technique should be learned. Hemorrhage: Achieve hemostasis PRIOR to final packing. |
|
|
PROBLEM: Inadequate tooth reduction.
|
Conservative treatment has already failed by the time a tooth requires a crown. If it's indicated it should be FULLY REDCUED consistent with the restoration being provided.
SOLUTION: - determine amount of tooth reduction required for intended restoration - use some form of depth guide to ensure sufficient reduction - work in a prescribed logical sequence |
|
|
Describe the procedure of PACKING RETRACTION CORD:
|
1) Remove all pre-packed cords prior to using infuser tip
2) Select diameter of cord that you estimate will fill the smallest most delicate area of the sulcus (usually #1) 3) Use one long cord for each prep 4) place the cord in a dappen dish/medicine cup containing Astringident solution 5) Allow to soak 6) Use infuser tip as directed - angle tip towards GINGIVA (not tooth) and gently rub sulcus while expressing solution 7) when bleeding stops, wash all coagulum off the tooth and out of sulcus 8) continue to use syringe and Astringident until sulcus can be vigorously washed with three-way syringe w/o bleeding =============================== DO NOT PACK CORD UNTIL THIS DEGREE OF HEMORRHAGE CONTROL HAS BEEN ESTABLISHED =============================== 9) Begin packing where sulcular tissue is LEAST likely area to damaged i.e. palatal aspect of max. preps or deepest part of sulcus 10) Start packing at the end of the cord (not in the middle) 11) Pack the soaked cord once around the tooth in a deliberate manner so that ALL (not just portions) of the sulcus receives and is displaced by cord. *CRITICAL* 12) Use the extra length of cord to DOUBLE PACK and displace those areas of the sulcus not adequately displaced while avoiding those areas already adequately displaced by the single first layer of cord 13) Cut off any remaining excess length of cord leaving an unpacked tag at the end to aid removal 14) Wait approx. 5 min 15) Obtain bite records or allow the patient to take a break 16) Obtain bite records or allow the patient to take a break |
|
|
What are the steps for removing packing cord for PARTIAL COVERAGE RESTORATIONS?
|
- rinse, dry, isolate, and take impression with cord in place
- remove cord after inspecting impression for accuracy |
|
|
What are the steps for removing packing cord for MULTIPLE PREPARATIONS?
|
TECHNIQUE 1
------------------- Pull cord, rinse, dry, isolate. If any bleeding occurs when cord is pulled, reenter sulcus with syringe and infuser tip until hemorrhage is controlled, then rinse, dry, isolate, and take impression TECHNIQUE 2 ---------------------- Prior to pulling the retraction cord, wash and thoroughly dry the ENTIRE ARHC, re-isolate the preparation area, and specifically dry the sulci of the prepared tooth (including cord). |
|
|
What are the steps for removing packing cord for MULTIPLE ADJACENT RESTORATIONS?
|
- easier to pull all of the cords prior to injeting the impression material
|
|
|
What tooth should you start injecting impression material into if you were working on multiple restorations?
|
Disto-lingual line angle of the most distal preparation, into or just barely above the sulcus touching both prepared tooth and distal approximating tooth.
|
|
|
TRUE or FALSE: Impression material should be expressed into the sulcus AHEAD of the injection tip.
|
TRUE: always keep impression material flowing ahead of tip
|
|
![Identify the type of margin that [1] is:](https://images.cram.com/images/upload-flashcards/871012/1373054_m.jpg)
Identify the type of margin that [1] is:
|
FEATHER EDGE
|
|
![Identify the type of margin that [2] is:](https://images.cram.com/images/upload-flashcards/871012/1373057_m.jpg)
Identify the type of margin that [2] is:
|
CHISEL / KNIFE EDGE
|
|
![Identify the type of margin that [3] is:](https://images.cram.com/images/upload-flashcards/871012/1373060_m.jpg)
Identify the type of margin that [3] is:
|
BEVEL SLOPED SHOULDER
(X) DEGREE SHOULDER |
|
![Identify the type of margin that [4] is:](https://images.cram.com/images/upload-flashcards/871012/1373063_m.jpg)
Identify the type of margin that [4] is:
|
CHAMFER
|
|
![Identify the type of margin that [5] is:](https://images.cram.com/images/upload-flashcards/871012/1373066_m.jpg)
Identify the type of margin that [5] is:
|
DEEP CHAMFER
|
|
![Identify the type of margin that [6] is:](https://images.cram.com/images/upload-flashcards/871012/1373069_m.jpg)
Identify the type of margin that [6] is:
|
SHALLOW/LONG CHAMFER
|
|
![Identify the type of margin that [7] is:](https://images.cram.com/images/upload-flashcards/871012/1373072_m.jpg)
Identify the type of margin that [7] is:
|
ROUNDED SHOULDER
|
|
![Identify the type of margin that [8] is:](https://images.cram.com/images/upload-flashcards/871012/1373075_m.jpg)
Identify the type of margin that [8] is:
|
SQUARE SHOULDER
|
|
![Identify the type of margin that [9] and [10] is:](https://images.cram.com/images/upload-flashcards/871012/1373078_m.jpg)
Identify the type of margin that [9] and [10] is:
|
BEVELED CHAMFER and BEVELED SHOULDER
|
|
|
Which margin has the BEST closing angle configuration?
|
Feather edge
|
|
|
What are generally the most advocated margin designs?
|
- Deep chamfer
- Shoulder - Beveled shoulder |
|
|
What are some "tests" to check whether a margin can be metal or whether it should be all-porcelain?
|
- probe the sulcus and see if metal of probe is visible through tissue, awkward to inset, or causing noticeable blanching
|
|
|
What depth of sulcus will easily allow a metal collar?
|
3mm sulcus
|
|
|
OUTLINE THE ACCEPTABLENESS FOR A PFM TOOTH PREPARATION:
|
INCISAL REDUCTION
------------------------------- straight and uniform, 2.0mm may be bevelled lingually LINGUAL REDUCTION ------------------------------ Clearance with lower incisors, 1.0 - 1.5 mm Lingual fossa slightly concave Lingual axial wall, 1.5 mm tall AXIAL REDUCTION --------------------------- Follows contour of original tooth 1.25 mm gingival Lingual 0.3-0.7mm at gingival Proximal 1.25mm (as viewed from facial) DRAW AND TAPER -------------------------- 10 degrees mesiodistal / 20 degrees acceptable Able to visualize all walls Draw follows long axis of tooth GINGIVAL EXTENSIONS --------------------------------- 0.2-0.5mm above tissue PROXIMAL GINGIVAL CLEARANCE -------------------------------------------- 0.5mm clearance MARGIN DEPTH / FORM ------------------------------------ Deep Chamfer (1.0-1.25mm wide) Interproximal transitions Chamfer on lingual (0.3-0.7mm) |
|
|
What are the biologic requirements for a PROVISIONAL?
|
PULPAL PROTECTION - must seal and insulate the prepared tooth
MAINTAIN PERIO HEALTH - facilitate plaque removal, marginal fit, contour, and smooth OCCLUSAL STABILITY - maintain proper contacts with adjacent and opposing teeth PREVENTION OF ENAMEL FRACTURE - esp partial coverage REMOVAL FOR RE-USE DISPLACEMENT - prevented by proper tooth prep and well adapted internal aspects ESTHETIC - diagnostic provisional |
|
|
What materials are available for making provisionals?
|
- PMMA self cure (Alike)
- PMMA light cure (Unifast) - BisGMA composite (ProTemp, Integrity) - PEMA - Radica |
|
|
What are the ADVANTAGES / DISADVANTAGES of PMMA materials?
|
ALIKE
--------- ADV: cost, strength, easy to repair/modify DIS: odour, exothermic, shrinkage |
|
|
What are the ADVANTAGES / DIS of INTEGRITY?
|
ADV: no shrinkage, easy of use, esthetic
DIS: cost, difficult to repair or add to, brittle |
|
|
What are the different methods for making a provisional?
|
DIRECT TECHNIQUE
INDIRECT TECHNIQUE INDIRECT-DIRECT TECHNIQUE (shell-reline: multiple teeth/bridges) |
|
|
What are the ADV/DIS of DIRECT PROVISIONAL TECHNIQUE?
|
ADV:
- quick and easy for single restoration - less laboratory preparation DIS: - potential thermal trauma - potential chemical trauma - potential for marginal distortion with shrinkage - more chairside time |
|
|
What are some methods of MINIMIZING HEAT TRANSFER to the pulp when making a DIRECT PROVISIONAL?
|
1) In Situ
- complete polymerization occurs intraorally on the prepared tooth. Upon initial polymerization the acrylic is cooled with air/water syringe. ADV: less distortion, best marginal fit, DIS: high potential to lock into adjacent proximal undercuts 2) REMOVAL - upon initial polymer, remove temp, and place into WARM water to complete polymerization ADV: no potential to lock on; DIS: decreases marginal fit if removed early 3) ON/OFF - upon initial polym, lift provisional, flush with A/W, replace, and repeat until fully polymerized. ADV: no potential to lock on; DIS: most distortion and highest marginal discrepancy |
|
|
What is DR.T's preferred sequence of tooth prep?
|
- occlusal bulk reduction
- buccal bulk - lingual bulk - proximal - smooth axial surfaces and margins - extend margins if needed |
|
|
What are some COMMON ERRORS in tooth preparation?
|
- not using new diamonds
- insufficient reduction - insufficient margin depth / geometry - lip at margin- check with explorer - grazing adjacent tooth |
|
|
What are some COMMON ERRORS in provisionalization?
|
- starting too late
- under-contoured facially/ lingually - short margins - over-contoured - under-polished (rough surface) |
|
|
Who said "The goal of prosthodontics is not only the meticulous replacement of that which is missing, but the preservation of that which remains."?
|
M.M. Devan
|
|
|
What are some patient assessment tools used in treatment planning?
|
- patient interview and history
- clinical examination - radiographic examination - mounted models |
|
|
What are some findings that may indicate the need for periodontal treatment in conjunction with or prior to fixed prosthodontic therapy?
|
- pocket depth excess of 3.0mm
- furcation involvement - deviation of normal colour, contour, texture of gingiva - marginal exudate - less than 2.0mm of attached gingiva present - muscle or frenal pulls - moderate-severe recession |
|
|
From a prostho standpoint, what are the goals of perio treatment of a full coverage restoration?
|
1) restoration of periodontium to optimal health
2) to create an environment that the patient can maintain |
|
|
What conditions can cause PDL irritatio?
|
- tooth movement due to prosthesis or occlusion
- tooth or restoration in traumatic occlusion - acute pulpitis - gingivitis or periodontitis - cracked tooth |
|
|
TRUE or FALSE: All endo treated posterior teeth should be crown?
|
TRUE
|
|
|
What are some important RADIOGRAPHIC SURVEY evaluations?
|
- Evaluate existing restorations (proximal contours, margins defective, recurrent decay)
- Endo teeth (adequacy of fill, radiolucency in apical areas) - root length, size, form - Crown/Root ratio |
|
|
What is the purpose of having MOUNTED CASTS?
|
- Allows superior visualization (extruded, rotated, malposed teeth, defective restorations, shape of tuberosities, location of frenal attachments, available interarch space)
- Allows for a detailed occlusal analysis - Patient education and in tx plan presentation - Diagnostic casts are permanent record (medico-legal) - essential for tx planning in prostho - Occlusion can be evaluated (traumatic, wear) - occlusal interferences - occlusal plane considerations - |
|
|
What is the purpose of a FACEBOW TRANSFER?
|
- to relate condylar components of articular to the patient in an anatomic manner
|
|
|
What are some methods of correcting occlusal plane disruptions?
|
- orthodontic repositioning
- enameloplasty ------------------ if a tooth requires more than 2mm of enameloplasty then a CROWN is indicated |
|
|
What are the INDICATIONS for treatment with a SINGLE FIXED FULL COVERAGE RESTORATION?
|
- extensively restored tooth
- fractured cusps or crowns - endo treated teeth (posterior mainly) - esthetics (colour, contour, etc) - Loss of tooth structure through erosion, abrasion - Tooth wear (evaluate VDO, habits) - Occlusal plane correction - Replacement of existing inadequate full coverage restorations - Implant prosthodontics |
|
|
What are some options for PARTIALLY EDENTULOUS patients?
|
- fixed partial denture
- removeable partial denture - implant supported or retained restoration - complete denture - removeable partial denture - complete overdenture |
|
|
What should be presented to a patient?
|
- Present no more than 3 options
- Cost/Time - Expected prognosis - Adv/Disadvantages |
|
|
What are the features of an ACCEPTABLE IMPRESSION?
|
1. Prepared tooth and margins recorded
2. TOoth structure BEYOND MARGINS recorded 3. Adjacent teeth/tissues recorded 4. No bubbles, tears, imperfections |
|
|
What are the different types of cords?
|
TWISTED: plain cotton, multiple strands, easily compressed, can fray
BRAIDED: keep shape, not compressed, little adhesion to tissue, do not fray KNITTED: absorb more chemicals, tend to rebound in sulcus, adheres to tissue RINGS: no cutting required, need multiple sizes - ring form |
|
|
What are the two most commonly used medicaments?
|
HEMODENT (Aluminum chloride 5%, 25%)
ASTRINGIDENT (Ferric sulfate 13.3%) |
|
|
What are the signs of EPINEPHRINE SYNDROME?
|
SIGNS:
- increased HR - increased BP - increased RESP SYMPTOMS: - headache - dizziness - tremor - fear - nervousness |
|
|
What are the properties of HEMODENT (5% AlCl)
|
- minimal tissue damage
- 10 minutes - routine use - no systemic effects - milder - does not stain tooth |
|
|
What are the properties of FERRIC SULFATE?
|
- minimal tissue damage
- 3 minutes recommended - with epinephrine - directly against cut tissue - temporary discoloration of tissues |
|
|
How long does discoloration of tissues from ASTRINGIDENT last?
|
1-2 days
|
|
|
Why is VISCOSTAT preferred?
|
20% Ferric sulfate
- less acidic - does not remove smear layer from prepared tooth |
|
|
How much recession generally occurs from retraction cord use?
|
Minimal - 0.1mm
|
|
|
What are the INDICATIONS for TWO CORD TECHNIQUE?
|
- deep sulcus
- multiple teeth - hemostasis - fibrous gingiva - can be used routinely |
|
|
What are the general choices for FIRST and 2nd CORD in 2-cord technique?
|
FIRST: #000 or 00
SECOND: #0, 1, 2 cord |
|
|
TRUE or FALSE: First cord in 2-CORD tEchnique should be soaked in hemostatic agent of choice.
|
FALSE - soak in water
|
|
|
What are the indications for LESS RETRACTION TIME?
|
- shallow sulcus
- thin fragile marginal tissue - critically esthetic zones - larger cords - more cords - more aggressive medicaments - traumatized tissue - 2nd/ 3rd retraction |
|
|
What are the indications for MORE RETRACTION TIME?
|
- deep preparation
- hemorrhage prone - fibrous resistant gingival tissue - non-esthetic zones - smaller cords - fewer cords - milder medicaments (hemodent) |
|
|
What are the requirements of an impression?
|
- Contours of the prepared teeth, including all cavosurface margins and some submarginal area should be recorded
- occlusal surfaces of all unprepared teeth should be accurately recorded - soft tissues of edentulous areas should be recorded to aid in developing pontic contours - impression material should be free of voids in critical areas, no air trapped between injection material and tray material |
|
|
What should be checked PRIOR to restoration try-in appointment?
|
EVALUATED ON ARTICULATOR FOR:
- marginal adaptation - proximal / occlusal contours - occlusal form - axial contours - tissue relationship / contact of pontics - stability on die - surface finish - porcelain shades verified against tab - gross deficiencies should be corrected prior to appt. |
|
|
What is the sequence of steps to TRY-IN / ADJUST fixed restorations?
|
1) LOCAL ANAESTHESIA
2) Remove provisional 3) Tissue management 4) Seat restoration fully 5) Confirm marginal accuracy 6) Check proximal contacts 7) Assess stability 8) Adjust occlusion 9) Assess axial contours 10) Finish and polish restoration |
|
|
You are trying in a crown but it does not seat completely, what do you do now?
|
- Check interior of restoration or the preparation surface for cement or other debris
- if no debris present, then check the interior of the restoration for positive blebs that may prevent seating - remove blebs with HS ROUND BUR - re-seat - check proximal contacts for excessive pressure with floss while seating restoration with finger pressure (patient may inform you of tightness) - adjust proximal contacts with diamond and/or green stone - evaluate for axial wall bindind - use FitChecker placed in restoration and seated onto prep, binding shows of axial walls - adjust tight areas with HS Round bur (occlusal) or diamond (axial) - at this stage call instructor. May need to be remade |
|
|
How does one correct UNDEREXTENDED or OPEN MARGINAL DISCREPANCIES?
|
- must be re-made as these types can't be corrected
- |
|
|
What is the thickness of BLUE MYNOL?
|
60-90 microns
|
|
|
What is the thickness of ARTICULATING FOIL?
|
8 microns
|
|
|
What is the thickness of SHIMSTOCK FOIL?
|
8 microns
|
|
|
Where should CENTRIC CONTACTS be located?
|
- Centric fossae
- Marginal ridges - Cusp tips ELIMINATE ANY CONTACTS ON INCLINES |
|
|
TRUE or FALSE: There should be no eccentric contacts present on posterior restorations.
|
TRUE
|
|
|
No overcontouring should be apparent in the gingival 1/3 of the restoration.
|
t
|
|
|
TRUE or FALSE: Core may serve as an interim restoration prior to crown fabrication.
|
TRUE
|
|
|
What are the ADVANTAGES of a TWO STEP APPROACH to RESTORATION OF ENDO TREATED TEETH?
|
1) Post-core foundation restores the integrity of the pulpless tooth as a single unit, rendering it independent of the restoration that covers it
2) Changes can be made in the restoration without disturbing the main body of the tooth, such as removal of a single unit restoration for the purpose utilizing it as an abutment for a fixed bridge 3) The fit of the margins of the coronal restoration is independent of the post-core and its fit 4) It is possible to parallel abutment teeth in a fixed bridge more effectively |
|
|
What are the FOUR FUNDAMENTAL FACTORS INFLUENCING THE CHOICE OF FOUNDATION?
|
THE CONDITION OF THE TOOTH
- amount of intact coronal tooth structure is most influential factor determining the foundation type - much or all coronal structure is missing then foundation with max resistance and retention recommended THE PURPOSE FOR WHICH THE TOOTH IS USED - single unit vs bridge abutment? OCCLUSION / OCCLUSAL HABITS - no occlusal contact, potential for function low, minimal restorative needed - if subject to much occlusal loading, bruxism, etc then it should be protected THE ROOT/CANAL MORPHOLOGY - tooth with narrow tortuous canals may not be possible to negotiate and may be treated conservatively with a short post, auxillary pins, or bonded core |
|
|
What are the THREE MAIN TYPES OF FOUNDATIONS and what are they used for?
|
CUSTOM CAST POST-CORE
-------------------------------------- - incisors, canines, bicuspids become extremely weakened from access opening for endo, almost always require replacement of coronal tooth structure with a cast post-core. - for most single rooted teeth because of increased strength of the one-piece castings and its resistance to rotation - direct / indirect pattern of internal anatomy of the tooth - preparation limited to removal of undercuts and placement of anti-rotational device PREFABRICATED POST AND DIRECT CORE ---------------------------------------------------------- - direct restorative material is adapted to the post and tooth to form the core - lower time involved - lower cost - potential to perforate the lateral walls of the apical portion of the root ALL AMALGAM FOUNDATION ------------------------------------------ - coronal/radicular foundation technique using amalgam only is advocated for use in multi-rooted teeth - |
|
|
What is the method of choice for CAST-POST CORES of POSTERIOR TEETH?
|
Single cast core portion with imbedded "sliding" parallel sided posts
|
|
|
What is the general guideline for whether you decide to do PARA-POST-CORE on posterior tooth?
|
- one post for every missing 1/3 of total pulp chamber axial wall surface to a maximum of 2 posts
- molars missing greater than 2/3 of pulp chamber should be treated with CPC |
|
|
In general, endo treated teeth should have a post in what situations?
|
- when tooth requires a crown
- when tooth has had previous caries - restorations or fractures which have weakened remaining tooth structure - greater functional demands are required of the tooth - large canals / thin walls present in young teeth |
|
|
What are the steps for TAPERED CAST-POST-CORE PREPARATION?
|
1) RCT must be properly done (Radiograph) and asymptomatic
2) Remove all previous restorations, caries, pulp chamber fill 3) Prepare margins on sound tooth structure to proper depth of reduction for crown 4) Remove all liable (unsound) tooth structure. Require 1/2mm minimum between internal and external preparation 5) Need 2mm minimum O-G clearance for bulk of core. This is in addition to occlusal reduction requirements for the crown. 6) Prepare positive occlusal seat. No bibevel. 7) Goal is to prepare maximum length of canal (desired 10mm) but must not disturb apical 4-5 mm of fill and seal 8) initially remove GP to within 1-2 mm of desired length 9) Start GP removal with #4 Gates-Glidden bur for the first 3mm, #3 GG for the next 3mm, and #2 GG for the remainder. Smaller canals may require smaller Gate-Glidden or shorter steps. 10) Verify the preparation length and remaining fill with radiograph 11) Adjust for remaining post length to desired length 12) Smooth lateral walls and impart gentle taper with tapered diamond in slow speed friction grip contra-angle 13) Moderate to large undercuts are to be blocked out. Smaller undercuts can be removed by preparation, but remember we should preserve as much tooth structure as possible 14) If canal preparation is near round include an anti-rotational notch in the widest axial wall 15) Round sharp line angles (canal-occlusal seat) |
|
|
What are the steps for PARAPOST PREPARATION?
|
1) RCT must be properly done (radiograph) and asymptomatic
2) Remove all previous restorations, caries, pulp chamber fill 3) Prepare margins on sound tooth structure to proper depth of reduction for crown 4) remove all liable (unsound) tooth structure. Require 1/2mm min between external and internal preparation 5) Need 2mm minimum O-G clearance for bulk of core. This is in addition to occlusal reduction requirements for the crown. 6) Prepare positive occlusal seat. No bibevel. 7) Goal is prepare maximum length of canal (desire 10mm) but must not disturb apical 4-5mm of fill and seal 8) Initially remove GP to within 1-2mm of desired length 9) Start GP removal with #4 Gates-Glidden bur for the first 3mm, #3 GG for the next 3 mm and #2 GG for the remainder. Smaller canals may require smaller Gates-Glidden or shorter steps. 10) Start canal preparation with smallest Peeso-Reemer and/or pre-fabricated drill size and prepare to 1-2mm of desired length 11) Verify the preparation length and remaining fill with radiograph with post in place 12) Adjust for remaining post length to desired 13) Proper width of preparation has been achieved when 1/2-2/3 the apical length of the post has been prepared parallel and the post is relatively stable. Increase drill diameter and post diameter until stability is achieved, but be aware of remaining tooth structure and possibility of perforation. 14) Leave all undercuts 15) Place anti-rotational notch in the widest axial wall if coronal portion of canal is circular 16) Round sharp line angles (canal-occlusal seat) |
|
|
What are the steps of making PARALLEL PREFAB POST and DIRECT CORE?
|
1) Prepare post space as in PARAPOST
2) Shorten prefabricated post from apical end prior to cementation so that retentive portion of coronal portion of post remains within core contours 3) Cement post 4) Keep cement out of anti-rotational notch and coronal 2mm of canal prep 5) Place core material into 2mm of canal prep and adapt to post 6) Prepare core |
|
|
WHat are the steps in TEMPORARY FABRICATION FOR CAST POST CORE?
|
1) Place cotton pellet so coronal 5mm of canal available
2) Lubricate canal slightly (saliva, die-sep, vaseline) 3) Bead brush temporary acrylic into canal to occlusal seat 4) Fill vacuum template matrix, polycarboxylate crown, shell form with acrylic 5) Seat matrix onto preparation 6) Allow to fully seat 7) Remove, inspect for detail 8) Reseat, adjust to remove functional contacts (keep CO) 9) Trim and polish 10) Replace cotton pellet (cement barrier) 11) Cement temporary |
|
|
Whats the rationale for TEMPORARY?
|
- prevent drifting and over-eruption of teeth
- esthetics - function |
|
|
What are the INDICATIONS for DIRECT PATTERN TECHNIQUE for CPC?
|
- difficult core contours
- custom fabrication to previous crown |
|
|
What are the ADVANTAGES of DIRECT PATTERN TECHNIQUE FOR CPC?
|
- less laboratory time
- cost - full control of core shape and size |
|
|
What are the INDICATIONS for INDIRECT (IMPRESSION) TECHNIQUE for CAST POST CORE?
|
- large undercuts, undercuts which can't be blocked out
- multiple preparations - divergent canals ADV: Less chairside time |
|
|
What must be determied to ensure that an endodontically treated tooth is ready for subsequent restorative treatment?
|
- good apical seal
- no sensitivity to pressure - no exudate - no fistula - no apical sensitivity - no active inflammation |
|
|
What six features must be incorporated into the tooth preparation for a CAST POST CORE?
|
- apical seal
- minimal enlargement - length - stop - anti-rotation - margin extension |
|
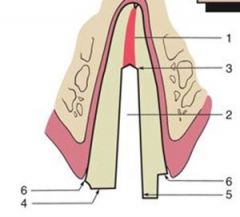
Label the following:
|
1. Apical seal (4-5mm)
2. Minimum canal enlargement (no undercuts remaining) 3. adequate post length 4. positive horizontal stop (to minimize wedging) 5. vertical wall to prevent rotation 6. externsion of the final restoration margin onto sound tooth structure |
|
|
Discuss 5 variables that have an impact on retention form for CPC's?
|
1. Preparation geometry
2. Post length - should be as long as possible without jeopardizing the apical seal or strength or integrity of remaining tooth structure - or 2/3 root length 3. Post diameter - increase diameter increase retention - do not exceed ONE THIRD of cross-sectional root diameter 4. Post-surface texture - serrated or roughened are more retentive 5. Luting agent |
|
|
How is an interim restoration fabricated for a mandibular second premolar that has been prepared for a CPC?
|
1. Place piece of wire in the post space, to avoid root fracture it must extend passively to end of post space. Mounted stone can be used to taper the wire if binding occurs
2. Mark wire with pencil at the mouth of post space, then at point slightly occlusal to this mark use the pliers to make a 180-degree wire bend 3. Lubricate the tooth and surrounding soft tissues with petroleum. Paper points are convenient for this. 4. Fill the ESF with interim resin (poly methacylate recommended) 5. When the resin loses its surface gloss, place wire in the post space and seat the ESF over it. Precautions must be taken to protect the patient from swallowing or aspirating the wire. 6. Remove the ESF while the resin is still rubbery (after about 2-2.5 min. Stage of polym should be monitored. If resin is allowed to become rigid and lock into undercut surfaces within the post preparation, removing it and wire will be time consuming and risk restorability of the tooth. 7. Mark the margins with a pencil and trim and contour the restoration with disks or straight handpiece carbide burs 8. Evaluate the restoration in the mouth. Adjust as necessary 9. Polish, clean, and cement restoration |
|
|
What would be the outcome of placing the maring too deep in the sulcus?
|
Possibility of biologic width violation, chronic gingival inflammation
|
|
|
Prepared cervical margin should follow what?
|
Scalloped anatomy of alveolar bone, attachment, and gingival tissues
|
|
|
What is the CRITERIA FOR MARGIN SELECTION?
|
1) Selected margin must provide a predictable level of marginal integrity
2) minimize plaque accumulation and selected margin must present smooth materials to the gingival sulcus 3) in some situations must provide acceptable aesthetics |
|
|
What are some problems that can result from improper preparation and placement of cervical margins?
|
- biologic width violation
- metal margins showing through thin gingiva - recession exposing tooth/rest surface - opacity in cervical third of restoration - roughness of cervical margin: contributes to plaque accumulation |
|
|
List all of the margins that are acceptable for METAL CERAMIC CROWNS:
|
- knife-edge
- chamfer - shoulder - buttjoint - beveled shoulder - slant shoulder - disappearing margin |
|
|
What is the IDEAL margin for a PFM?
|
SHOULDER and any variation of it
|
|
|
How wide should the collar of a shoulder for PFM be?
|
1mm or more
|
|
|
What is the IDEAL margin for a PFM with metal collar/disappearing margin?
|
SLANTED SHOULDER
|
|
|
Why is a bevel margin better for PFMs?
|
Substantial metal collar which provides best initial fit before firing porcelain, this fit is maintained over all ceramic firing cycles.
Can be highly polished (smoothness for biocompatibility) Problem is aesthetics |
|
|
What is important when choosing SHOULDER BEVEL margin?
|
- metal display inherent
- patient should sign consent prior to utilizing this margin design |
|
|
If AESTHETICS are important what are some design options for a crown?
|
1) USE ALL CERAMIC CROWN
- shoulder margin with rounded internal line angle - 90 degrees to external angle of labial/buccal surface - 1.2-1.5 mm depth for optimum aesthetics - if SLANT in margin is present, tensile forces occur in function, HALF-MOON fractures in the cervical area 2) METAL-CERAMIC RESTORATION - Porcelain labial margin (shoulder) - disappearing margin - inherent roughness of disappearing margin - patients with low smile line, slant shoulder with metal collar should be considered - if smile exposes cervical portion of restoration, disappearing is the choice - shoulder margin carried INTERPROXIMALLY to proximal lingual line angle.. 1.2 mm - 3) EXTEND METAL FRAMEWORK TO AXIO-GINGIVAL LINE ANGLE - shorten metal framework and terminate it 1mm from shoulder margin (metal cutback) |
|
|
What is the MOST COMMONLY used shade matching method?
|
VISUAL- vitapan,
|
|
|
ALL CERAMIC crown usually has what layers?
|
- core material
- body porcelain - incisal porcelain |
|
|
TRUE or FALSE: Veneer preparation was initially done with minimal or no preparation.
|
TRUE
|
|
|
What is the main reason for VENEER PREPARATION?
|
- exposure of enamel rods for superior bond strengths
|
|
|
What are the three types of INCISAL PREP for veneer?
|
- window
- overlapped incisal edge - feathered incisal |
|
|
What can one do during VENEER IMPRESSION to help with die separation?
|
Place clear matrices interproximall
|
|
|
What materials are used for VENEER?
|
FELDSPATHIC PORCELAIN
- platinum foil tech - refractory die technique EMPRESS/E-MAX - CAD or pressed |
|
|
What is the IDEAL preparation for bonding VENEER?
|
- etching inner surface with HYDROFLUORIC ACID and SILANATION = higher bond strength of luting composite to porcelain than bond strength of luting composite to enamel
|
|
|
If there is contamination of the surface with saliva during bonding a VENEER what should you do?
|
Re-etch with 37% phosphoric acid
|
|
|
What is the preferred method for LUTING veneer?
|
- light curing composite
- longer working time - color stability is superior - Thickness of greater than 0.7mm may require DUAL CURE cement - place clear matrices / wedges during cementation |
|
|
What is the typical failure rate of VENEER (porcelain)?
|
5% after 5 years
|
|
|
What are the ADV / DISADV of CERAMIC INLAYS/ONLAYS?
|
ADVANTAGES:
- improved aesthetics - good durability and strength - eliminates any shrinkage during curing DISADVANTAGES - possible wear of luting agent - possible wear of opposing teeth - luting gaps are often wider than ideal |
|
|
Generally, what is the 10 year survival rate of CERAMIC ONLAYS/INLAYS?
|
90%
|
|
|
The tooth gets its colour primarily from what?
|
DENTIN
|
|
|
What are the three components of colour?
|
HUE
CHROMA VALUE |
|
|
Arrange which 1/3 of the tooth has MOST to LEAST amount of colourL
|
MIDDLE THIRD > cervical third > incisal
|
|
|
Define METAMERISM:
|
two colours that appear to be a match under a given lighting condition but have differenet spectral reflectance are called metamers
|
|
|
How can the problem of metamerism be avoided?
|
- selecting a shade and confirming it under a variety of lighting conditions
- providing sufficient bulk of porcelain over opaque - minimizing surface modifications with external stains |
|
|
What is the SEQUENCE of shade selection?
|
HUE -> chroma -> value -> metameric effect
|
|
|
What HUE is in the ABCD shade guide?
|
A- brownish
B- yellowish C- grey D- reddish |
|
|
Which tooth is the most saturated in colour?
|
CANINE - use it to determine HUE
|
|
|
The SQUINT test is useful for what?
|
Determining VALUE!
|
|
|
How does one use the SQUINT test?
|
Squint until whichever disappears from sight first - tooth or shade tab. One that fades FIRST has lower value.
|
|
|
How can one DECREASE brightness of a restoration?
|
- increasing depth of translucency
- surface modification |
|
|
Which light is the most important for revealing metameric changes in colours?
|
SUBDUED TUNGSTEN LIGHT
|
|
|
What are the GENERAL PRINCIPLES in shade guide selection?
|
1. Use the shade guide that matches the type of porcelain to be used.
2. Patient should be viewed at eye level 3. Shade comparison should be made under different lighting conditions. Use full spectrum light if possible 4. Should be made at the START of the appointment 5. Teeth should be clean, remove dry calculus and stain by prophylaxis 6. Distracting, brightly coloured lipstick should be removed. Brightly coloured clothing should be draped. 7. Make shade selection initially with tooth and guide dry, then finally confirm under wet conditions. Place guide under lip, close to, and with same illumination as the tooth 8. Shade selections should be made QUICKLY to avoid fatigue of eyes. Rest eyes on grey surface to balance colour receptors. 9. Concentrate on MIDDLE THIRD of the tooth 10. Match the value, ideally use separate guide for this 11. MAKE A DRAWING of tooth for prescription 12. |
|
|
What happens to tooth colour when they get dry?
|
value INCREASES
|
|
|
Which receptors in the eyes allow us to see colour?
|
CONES
|
|
|
What are the principle goals of DENTAL CEMENTS?
|
- retention
- sealing (elimination of microleakage) |
|
|
What are the ideal properties of DENTAL CEMENTS?
|
WORKING TIME - adequate to allow proper mixing, loading and seating of crown
SETTING TIME - rapid set once in mouth after proper positioning MANIPULATION - low technique sensitivity so that slight deviation of ideal condition or handling will not critically affect result, easy manipulation FILM THICKNESS - less than 30 microns so that it does not affect tolerance to which we can fit our restorations BONDING/ADHERENCE - bonding and/or adherence to tooth structure and restorative material SOLUBILITY - low solubility in water, resistance to acid attack HIGH COMPRESSIVE/TENSILE strength THERMAL INSULATION - when used as a base, film thickness when used as luting agent too thin for thermal insulation PULPAL RESPONSE - low, biocompatible, possible obtundant FLUORIDE RELEASE - thought to be anticariogenic COLOUR - tooth coloured and translucent cements desired for aesthetics with translucent restorations. Opaque easier for cleaning. EASE OF CLEANING - adherence to tooth, soft tissue, and restoration impedes cement cleaning |
|
|
What are the mechanisms of action of dental cements?
|
NON-ADHESIVE LUTING: retention to small undercuts on tooth/restoration surfaces from cutting
MICROMECHANICAL BONDING: retention to microscopic undercuts due to etching, hybridization, etc. |
|
|
What is the order of COMPRESSIVE/TENSILE STRENGTH (strongest to weakest) of dental cements?
|
RESIN > resin reinforced GIC > GIC > Zinc phosphate > polycarb
[ RIGZP ] |
|
|
What is the order of BOND STRENGTH (strongest to weakest) of dental cements?
|
RESIN > resin reinforced GIC > GIC > Polycarb > ZnP
[ RIGPZ ] |
|
|
What is the order of SOLUBILITY (LEAST to most) of dental cements?
|
RESIN > PolyC > Resin-reinforced GIC > ZnP > GIC
[ RPIZG ] |
|
|
What is the order of FILM THICKNESS (SMALLEST to largest) of dental cements?
|
RESIN REINFORCED GIC < GIC < ZnP < Resin
[ IGZR ] |
|
|
Post-cementation thermal sensitivity has been reported for which dental cements?
|
ZnP and GIC (low pH at initial mixing)
|
|
|
What is the composition of Zinc Phosphate cement?
|
Zinc oxide + MgO
Phosphoric acid |
|
|
What are the ADV/DIS of Zinc Phosphate cement?
|
ADV:
- long track record - good physical properties with proper mixing - predictable, high rigidity (MOE) - easy to remove set material DIS: - no bond to tooth/resto - incidence of tooth sensitivity - increased microleakage compared to other cements |
|
|
FUJI PLUS is what kind of cement?
|
Resin-modified GIC
|
|
|
What TEMPORARY CEMENTS are there?
|
ZINC OXIDE EUGENOL (TempBond)
- setting accelerated with moisture and temp - effective seal - decreased sensitivity - sensitive effect on pulp - dissolves when exposed in oral environment - inhibits resin polymerization - can decrease strength by mixing petroleum jelly (max 20%) NON-EUGENOL ZINC OXIDE (Fregenol) - no sedative effect on pulp - compatible with resin material - doesnt adhere to metal as well as ZOE RESIN (TempBond Clear) - good aesthetics - higher strength and retention - difficult to see excess - may be difficult to remove - use lubricant over comp cores/restorations ZINC POLYCARBOXYLATE - good for temp cementation of bridges, preps with poor retention, long term provisionals |
|
|
What is the purpose of QUARTZ in PFM?
|
- stability by forming refractory skeleton
|
|
|
What is the purpose of KOALIN in PFM?
|
- sticky: holds the porcelain particles together during firing
- strongly opaque - current porcelains use organic binders such as sugars/corn starch |
|
|
What is the composition fo DENTAL PORCELAINS?
|
1) Feldspar
2) Quartz 3) Koalin (binder) 4) Fluxes 5) Coloring agents |
|
|
What are the COLORING AGENTS in PFM?
|
Metallic oxides
|
|
|
What is the purpose of FLUXES in PFM?
|
- change in firing temperature or thermal coefficient of expansion
|
|
|
What are some important PRE-OP ASSESSMENTS that should be made before making PFM?
|
- level of incisal edge
- overlap / occlusion - facial contours with adjacent tooth - proximal contacts - lingual wall height - |
|
|
TRUE or FALSE: The amount of ferrule is more important than the length of post in reducing root?
|
TRUE
|
|
|
What are the two ways of removing GP from root canal?
|
1) warmed endodontic plugger - eliminates possibility of damaging dentin
2) rotatry instruments - if GP is old and lost its thermoplasticity |
|
|
In short teeth, what is the absolute minimum that the POST length into canal can be
|
3mm
|
|
|
What are the steps in TRIAL INSERTION / CEMENTATION of post?
|
1) inspect casting (blebs, ribbons)
2) Remove temporary, cement, cotton pellet, and debris from canal 3) Trial seat post, core casting w/o pressure 4) if binding first remove likely areas 5) reseat, if still binding, sandblasting and pressure area will appear burnished 6) passive seating with stability should be evident 7) longer parallel posts 8) clean and dry canal 9) Mix Zn Phosphate cement 10) Place cement into canal with lentula spiral 11) Place cement on post and insert into canal 12) Verify seating 13) Hold in place until cement is set |
|
|
What are the IDEAL core material properties?
|
- adequate compressive strength
- flexural strength - biocompatibility - resistance to leakage - ease of manipulation - bonds to tooth structure - thermal coefficient similar to tooth structure - dimensional stability - minimal water sorption - inhibition of caries - esthetics |

