![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
148 Cards in this Set
- Front
- Back
|
hyperplasia vs neoplasia
|
hyperplasia
- proliferation of cells in response to a stimuli - remove the stimuli and it goes back to normal neoplasia - proliferation of cells after cessation of stimuli - benign - malignant (characerized by invasion/ metastasis) |
|
|
define hemaatopoietic neoplasia
|
neoplasia of hematopoietic cell origin
|
|
|
define cancer
|
malignant neoplasia
characterized by invasion or metastasis |
|
|
define leukemia
|
malignant neoplasm arising from hematopoietic cells in the bone marrow (or spleen)
spleen is also a hematopoietic organ and a lymphoid organ, not just a bag of red cells typically with significant #s of neoplastic cells in circulation “Leukemia” is also sometimes used to describe any condition in which neoplastic cells are present in circulation |
|
|
define lymphoma
|
(aka malignant lymphoma, lymphosarcoma) – malignant solid tissue neoplasm arising in lymphoid tissue(s) outside the bone marrow (neoplasm of lymphocytes)
|
|
|
normal hematopoietic differentiation
|

|
|
|
lymphoid vs myeloid neoplasia
|
Lymphoid neoplasia
- Lymphoid (lymphocytic) leukemias - Lymphomas - Plasma cell tumors (secrete immunoglobulins) Myeloid neoplasia - Myeloid (myelogenous) leukemias - Myelodysplastic syndromes - Other myeloid neoplasms |
|
|
lymphoma
|
It is not one dz, it is a spectrum of diseases
Many different forms, depending on: - Anatomic location - Cell type (B v. T v. NK) - Cellular morphology (sometimes small or sometimes big) - Histologic pattern - Stage (how disseminated it is in terms of anatomic location) - Biologic behavior - Response to therapy |
|
|
how do you dx lymphoma
|
Diagnosis usually based on FNA cytology +/or biopsy and histopathology
Dx typically followed by clinical staging (how advanced is the disease?) and immunophenotyping (ID of cell type using antibodies) |
|
|
histopath vs cytology
|
Histopath
- Chunk of tissue - Tissue architecture is intact Cytology - Sample lesion - Fast, cheap, good cell morphology - No architecture (can be limiting) - Not limiting in lymphoma |
|
|
laboratory abnormalities assoc with lymphoma
|
Laboratory abnormalities are variable
Hematology – nonregenerative anemia is common Chemistry – some forms of LSA are associated with hypercalcemia |
|
|
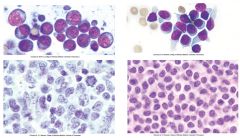
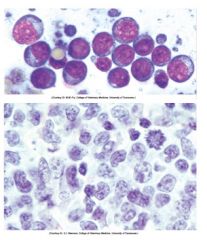
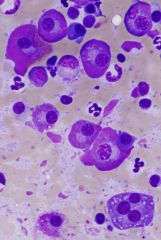
left = high grade lymphoma
- more aggressive - Big not well differented cells - More aggressive - Higher mitotic rate (notice mitotic figure) right = low grade lymphoma - less aggressive - Smaller cells - Lower mitotic rate - Less biologic aggressive behavior |
|
|
high grade lymphoma
notice mitotic figure/ lower cytoplasm : nucleus |
|
|
what is leukemia
|
malignant neoplasm arising from hematopoietic cells in the bone marrow (or spleen) typically with significant numbers of neoplastic cells in circulation
|
|
|
basic classification of leukemias (what cells they arise from)
|
lymphoid or myeloid
chronic or acute lymphoid leukemias - B or T cell origin myeloid leukemias - erythroid - granulocytic - monocytic - megakaryocytic |
|
|
what is a blast crisis
|
when a chronic leukemia transforms into a more acute form (some additional mutation)
|
|
|
Lymphoid vs Myeloid neoplasia *what cancers are included in each*
|
lymphoid
- lymphomas - lymphocytic leukemias - plasma cell tumors Myeoloid neoplasia - myeloid leukemias - myelodysplastic syndromes - other myeloid neoplasms |
|
|
what is lymphoma
what variables affect the form? how do you dx |
malignant solid tissue lymphoid neoplasm arising in lymphoid tissue(s) outside the bone marrow
variables include - anatomic distribution - immunophenotype (B or T vs. non B or T) - cellular morphology - histologic pattern - stage - biologic behavior - response to therapy initial dx - aspiration cytology +/or biopsy/ histopath - followed by clinical staging and immunophenotyping |
|
|
what laboratory values are assoc with lymphoma
|
hematology and chemisty are variable
|
|
|
what underlying factors are associated with lymphoma
|
cats
- FeLk cattle - BLV - persistent lymphocytosis - lymphoid neoplasia |
|
|
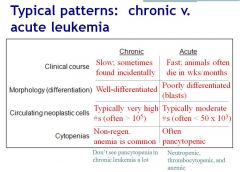
with _____ leukemias, the cell of origin is easy to identify.
Why is it sometimes difficult to dx. |
chronic leukemia
- b/c well differentiated cells sometims hard to tell if cells are neoplastic or reactive dx often one of exclusion |
|
|
______ are characterized high numbers of blasts in the bone marrow
why is it sometimes difficult to dx |
acute leukemias (> 20-30% of neucleated cells)
the specific lineage usually cant be determined by routine micro exam b/c poorly differentiated ID by immunophenotyping and/or cytochemical staining |
|
|
what is MDS
|
myelodysplastic syndrome
clonal myeloid proliferation characterized by ineffective hematopoiesis doesn't meet traditional definition for acute leukemia - MDS is characterixed by increased apoptosis compared to AML clasically dx by findings of - < 20-30% of blasts in bone marrow - cytopenia of > 1 cell line - morphological evidence of dyshematopoiesis |
|
|
how do you differentiate lymphoma from lymphocytic leukemia
|
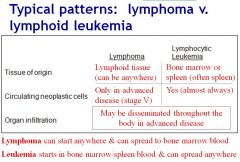
|
|
|
how do you differentiate b/w chronic and acute leukemias
|
|
|
|
where does lymphoma start & where can it spread?
leukemia? |
Lymphoma
- start anywhere - spread to bone marrow/blood leukemia - starts in bone marrow/spleen/blood and can spread anywhere |
|
|
Which leukemia is often characterized by neutropenia, thrombocytopenia, and anemia
|
acute
|
|
|
which leukemia is often characterized by non-regenerative animea but not pancytopenia
|
chronic
|
|
|
2 main forms of plasma cell tumors
|
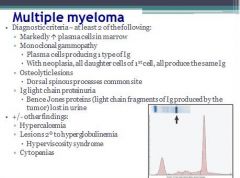
plasmacytoma
- solid tumors that typically involve skin or mm - usually benign - excision normally curative mult myeloma - typically arise from bone marrow - secrete large amts of Ig leading to hyperglobulinemia - dx based on finding at least 2 of the following 1) markedly increased numbers of plasma cells in bone marrow, esp in aggregates (plasma cells must be at least 30% of nucleated cells in the marrow) 2) monoclonal gammopathy 3) radiographic evidence of osteolysis (osteoclasts support growth of myeloma cells) 4) light chain proteinuria (don't react with dipstick protein indicators, require electrophoresis and immunoprecipitation) - may also see hypercalcemia, lesions assoc with hyperglobulinemia (hemorrhage due to secondary platelet dysfxn, renal amyloidosis, hyperviscosity syndrome), cytopenias due to high numbers of neoplastic cells in bone marrow |
|
|
immunophenotyping
|
use of antibodies to recognize specific molecules expressed on different cell types to determine identity of cell population
immunohistochemistry immunocytochemistry flow cytometry |
|
|
clonality assays
|
PCR for lymphocyte antigen receptor gene arrangements
exploits the fact that neoplastic cells are monoclonal whereas reactive cells are polyclonal highly sensitive and specific test valuabe for dx lymphoid neoplasia most useful in distinguishing lymphoid neoplasia (lymphoma or lymphocytic leukemia from non-neoplastic lymphoid proliferations |
|
|
plasma cell neoplasia
Multiple myeloma – malignancy of plasma cells, usually arises in bone marrow Plasmacytoma – solid tumors - Cutaneous - Extra-cutaneous (often @ mucous membranes) - Variable biologic behavior |
|
|
diagnostic criteria for multiple myeloma
|
|
|
|
what are some tumors of hematopoietic but not considered hematopoietic neoplasms
|
Mast cell tumors
Histiocytic tumors - Macrophages - Dendritic cells |
|
|
1. With _____ leukemia, ou will see a high lymphocyte count.
2. With _____ leukemia, where neoplastic cells are blasts, you may get errors b/c machine doesn't know how to count them. |
1. chronic
2. acute |
|
|
Immunophenotyping LSA
|
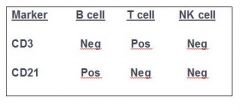
|
|
|
mechanisms of dz in the bone marrow
|
hypoplasia
hyperplasia dysplasia (messed up somehow making cells look wrong) aplasia neoplasia myelophthisis infection |
|
|
indications for bone marrow exam
|
unexplained cytopenias of one or more of the major hematopoietic lineages
- anemia - thrombocytopenia - neutropenia *help determine the mechanism of cytopenia* unexplained presence of abnormal cells in circulation - blasts - other immature cells (nRBC, immature granulocytes) - cells of abnormal morphology - well differentiated cells not normally found in circulation (ex mast cells) *helps determine mechanism causing presence of abnormal cells* cancer staging or monitoring - staging most commonly for lymphoma reasonable suspicion of neopolasia or infection in bone marrow - ex mult myeloma (esp in pt with monoclonal gammopathy), tick borne dz, fungal dz |
|
|
contraindications and complications of bone marrow
|
main contraindication = unnecessary bx
anesthesia is usually a greater risk than the collection procedure thrombocytopenia isn't a contraindication complications rare - iatrogenic infection - iatrogenic frx |
|
|
what do you do with the bone marrow sample
|
cytology & histopathology
if only 1 choice, cytology is the better choice (esp if highly cellular sample) cytology - faster - less expensive - excellent cellular morphologic detail - no tissue architecture - less reliable measure of marrow cellularity histopath - preservation of tissue architecture - more reliable assessment of marrow cellularity - slower - more expensive - inferior cellular morphologic detail |
|
|
preferred sites of bone marrow sample collection
|
crest of ilium
proximal humerus (cats/ small dogs) trochanteric fossa of femur sternum, tuber coxae (horses) |
|
|
bone marrow aspirate sample collection.
what do you need to put in syringe before attaching syringe to needle how much sample do you need |
0.3 ml EDTA
small amt (<0.5 ml) of marrow |
|
|
marrow cytologic interpretation
|
microscopic evaluation
- cell #'s, types, morphology - iron stores - +/- organisms need CBC (and preferrably a blood smear from same day as marrow collection) and thorough clinical work-up to fully interpret bone marrow findings |
|
|
what do you need to interpret bone marrow findings
|
a concurrent CBC and thorough clinical work up
|
|
|
marrow cytology interpretation
what do you look at under low power? high power? |
low power
- overall cellularity - megakaryocyte #s - iron stores - initial impression of M:E ratio high power - detailed evaluation of M:E ratio - #'s of minor cell populations (lymphocytes, plasma cells, macrophages, +/- others such as mast cells, osteoclasts, neoplastic cells) - cellular detail (maturation morphology) - +/- organisms |
|
|
normal marrow cellularity
|
age dependent
juvenile = 75% adult = 25% remaining non-hematopoietic is mostly fat |
|
|
how do you assess marrow cellularity (cytologic preparations)
|
on the basis of unit particles (small chunks of tissue)
how much of the unit particles consist of hematopoietic tissue instead of fat to a lesser degree on the density of individual hematopoietic cells in the monolayer of the slide |
|
|
causes of increased marrow cellularity
decreased marrow cellualrity |
increased
- hyperplasia of one or more hematopoietic lineages - neoplasia decreased - hypoplasia of one or more hematopoietic lilneages - fibrosis |
|
|
what do you look at in marrow cytology for cellular composition
|
evaluating 3 main marrow hematopoietic lineages (megakaryocytic, erythroid, granulocytic) as well as other cell types normally found in lower #s (lymphocytes, plasma cells, and macrophages)
mature megakaryocytes large with abundant slightly eosinophilic cytoplasm immature megakaryocytes smaller with less abundant more basophilic cytoplasm |
|
|
marrow hyperplasia witih increased M:E is
|
myeloid hyperplasia
|
|
|
marrow hypoplasia with increased M:E is
|
erythroid hypoplasia
|
|
|
bone marrow exam
What is the M:E ratio |
Rough estimate (subjective)
Quantitative assessment 100- v. 500- v. 1000-cell count The M:E in most normal dogs and cats is apx. 1:1 to 2:1. |
|
|
causes of increased marrow cellularity
|
hyperplasia of one or more hematopoietic lineages
neoplasia |
|
|
causes of decreased marrow cellularity
|
hypoplasia of one or more hematopoietic lineages
fibrosis |
|
|
bone marrow exam
what do you look at on low power (4x-10x) |
overall cellularity
megakaryocyte numbers iron stores inital impression of M:E ratio |
|
|
bone marrow exam
what do you look at on high power (50x-100x) |
detailed evaluation of M:E ratio
numbers of minor cell populations - lymphocytes - plasma cells - macrophages - +/- others (mast cells, osteoclasts, neoplastic cells) cellular detail (maturation/ morphology) +/- organisms |
|
|
normal marrow cellularity based on age
|
juvenile = 75% hematopoietic tissue
adult = 25% hematopoietic tissue |
|
|
bone marrow exam
in cytologic preparations, cellularity is assessed mainly on the basis of |
unit particles (small chunks of tissue)
how much of the tissue chunks consist of hematopoietic tissue instead of fat and to a lesser degree, the density of individual hematopoietic cells in the monolayer of the slide |
|
|
The M:E in most normal dogs and cats is approximately
|
1:1 or 2:1
|
|
|
what are the main cell types/ lineages assessed in the marrow evaluation
|
hematopoietic lineages
- megakaryocytic - erythroid - granulocytic other cell types normally found in lower numbers - lymphocytes - plasma cells - macrophages |
|
|
What is the M:E in most normal cats
|
1:1 or 2:1
|
|
|
What is the M:E in most normal dogs?
|
1:1 or 2:1
|
|
|
bone marrow exam
in cytologic preparations, cellularity is assessed mainly on the basis of |
unit particles (small chunks of tissue)
how much of the tissue chunks consist of hematopoietic tissue instead of fat and to a lesser degree, the density of individual hematopoietic cells in the monolayer of the slide |
|
|
The M:E in most normal dogs and cats is approximately
|
1:1 or 2:1
|
|
|
what are the main cell types/ lineages assessed in the marrow evaluation
|
hematopoietic lineages
- megakaryocytic - erythroid - granulocytic other cell types normally found in lower numbers - lymphocytes - plasma cells - macrophages |
|
|
What is the M:E in most normal cats
|
1:1 or 2:1
|
|
|
What is the M:E in most normal dogs?
|
1:1 or 2:1
|
|
|
bone marrow exam of megakaryocytes
|
majority are normally very large with abundant, slightly eosinophilic cytoplasm
immature ones are smaller and have less abundant, more basophilic cytoplasm |
|
|
bone marrow exam of erythroid and granulocytic cell numbers
|
assessed on the basis of overall marrow cellularity and myeloid:erythroid ratio
|
|
|
bone marrow exam
assessment of maturation of each lineage |
complete (maturation through segmented neutrophils and polychromatophilic erythrocytes)
synchronous (normal proportions of early and late stage cells |
|
|
how much of the population of nucleated cells is normally comprised of lymphocytes?
plasma cells? macrophages? |
lymphocytes: < 5% (dogs) or < 20% (cats)
plasma cells: < 2% macrophages: < 2% |
|
|
dysplasia
|
abnormal morphology
|
|
|
canine bone marrow iron stores
|
normally has small to moderate amts of hemosiderin
absence of bone marrow hemosiderin in dogs is an abnormality consistent with iron deficiency |
|
|
feline bone marrow iron stores
|
normally doesn't have detectable hemosiderin
presence of bone marrow hemosiderin in cats is consistent with iron overload |
|
|
what organisms can occasionally be detected in the bone marrow
|
bacteria
rickettsia fungi protozoa |
|
|
indications for bone marrow exam
|
Unexplained cytopenia(s):
- Anemia - Thrombocytopenia - Neutropenia Unexplained presence of abnormal cells in circulation: - Blasts - Other immature cells (e.g., nRBCs, immature granulocytes) - Cells of abnormal morphology - Well-differentiated cells not normally found in circulation (e.g., mast cells) Cancer staging or monitoring - e.g., Lymphoma Look for occult disease – especially if there is reasonable suspicion of neoplasia or infection in the bone marrow - e.g., Multiple myeloma - High globulins without evidence of infection response can be indicative of multiple myeloma |
|
|
what is the main contraindication for bone marrow exam
|
unnecessary bx
|
|
|
interpretation of M:E ratio in context of overall marrow cellularity
|
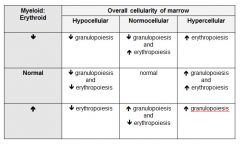
|
|
|
Interpretation of bone marrow results for patient with nonregenerative anemia
|
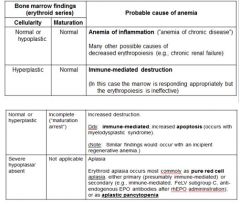
|
|
|
bone marrow hypoplasia indicates that cytopenia is probably due to
|
decreased production
|
|
|
bone marrow hyperplasia with unexplained non-regenerative anemia indicates that cytopenia is probably due to
|
increased destruction (usually immune mediated)
|
|
|
bone marrow maturation arrest indicates that a persistent cytopenia is probably due to
|
increased destruction (consistent with immune mediated disease of myelodysplastic syndrome)
|
|
|
bone marrow aplasia may occur in one or more lineages and main ddx are
|
immune mediated dz
toxic insult infectious dz idiopathic |
|
|
bone marrow microscopic interpretation of hypoplasia, hyperplasia, maturation arrest, aplasia
|
Hypoplasia: cytopenia is due to decreased production
Hyperplasia: cytopenia is due to increased destruction (usually immune-mediated) Maturation arrest: persistent cytopenia is due to increased destruction (consistent with immune-mediated disease or MDS). Aplasia may occur in one or more lineages Ddx include immune-mediated disease, toxic insult, infectious disease, idiopathic |
|
|
blood types
|
inherited antigens (alloantigens on RBC)
various RBC membrane proteins impt in transfusion medicine |
|
|
transfusion medicine
sensitization |
acquired alloantibodies
prior transfusion pregnancy certain vaccines |
|
|
which blood types are impt in dogs
|
DEA 1.1
|
|
|
what is the ideal canine donor?
|
DEA 1.1 neg
|
|
|
cat blood types
naturally occurring alloantibodies |
Type A
- weak anti-B antibody - transfuse type A cat with type B blood and get small transfusion rxn Type B - strong anti-A antibody - give small amt of type A blood, and will get life threatening transfusion rxn Type AB - not anti-A or anti-B |
|
|
canine blood types
|
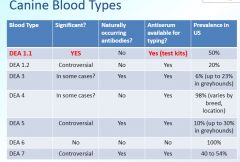
|
|
|
feline blood types
|
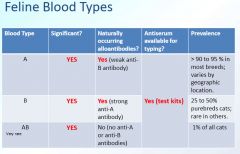
|
|
|
equine blood types
|
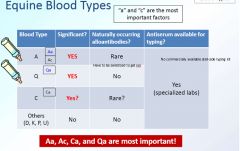
|
|
|
Have type AB cat, that is anemic and needs trx
1. Have type B blood sitting around, can you give it? 2.What about type A blood? |
1. No b/c type B blood has strong anti-A antibody
2. May still have rxn but won't be life threatening |
|
|
What type of blood should you give a Type AB cat?
|
type A or B packed, washed RBC
|
|
|
Type B cat given washed packed type A blood
|
will not stop the blood from being type A so you will still have the host response against the new cells (just not the response from the type A blood)
|
|
|
true or false
a cat with type AB blood is the universal recipient of whole blood |
false
it is the universal recipient of A or B packed, washed RBC |
|
|
will there be a rxn if give type B donor blood to a type AB cat
|
yes
whole blood of type B, plasma components have strong anti-A antibodies |
|
|
what equine blood types are the most impt
|
Aa
Ac Ca Qa |
|
|
do equine blood types have naturally occurring alloantibodies?
|
rare (Aa and Ac)
poss in Ca no for Qa |
|
|
do K9 blood types have naturally occurring alloantibodies
|
yes
- DEA 3 - DEA 5 - DEA 7 no - DEA 1.1 - DEA 1.2 - DEA 4 - DEA 6 |
|
|
do feline blood types have naturally occurring alloantibodies
|
yes
- A has weak anti-B - B has strong anti-A no - AB |
|
|
true or false
DEA 6 can be associated with NI |
false
its prevalance in the US is 100% |
|
|
cattle blood groups
|
Cattle have 11 blood groups with over 70 identified factors
Not many of them are clinically significant |
|
|
clinically most impt blood types
|
Dogs
- DEA 1.1 Cats - A - B - AB Horses - Aa - Ac - Ca - Qa |
|
|
which blood types are most impt in NI (hint: they are both equine)
|
Aa & Qa
|
|
|
when do you see NI in dogs, cats, and horses
|
dog
- DEA 1.1+ pup born to DEA 1.1- bitch - rare unless prior sensitization cats - type A or type AB born to type B queen horses - Aa+ foals born to Aa- mare - Qa+ foals born to Qa- mare - mule born to a mare bred to a jack |
|
|
what is the ideal donor for foal in NI crisis
|
Qa- blood from horse that was never sensitized
or packed, washed RBC from mare don't give blood from sire |
|
|
pretransfusion testing
|
blood typing
- confirm blood type cross matching - determine donor-patient compatibility |
|
|
agglutination testing
|
can be performed in test tube, on glass slide, or in gel
positive = RBC agglutination patient RBC and test kit reagents RBC & plasma from patient and donor |
|
|
hemolytic testing
|
positive = RBC hemolysis
some blood typing of cattle, pigs, and camelids has hemolysis as an end point |
|
|
blood typing for dogs/ cats
|
card
- test kit reagents contain either antiserum or lectins - reagent is mixed with patient blood (EDTA) - look for agglutination gel - neg = pellet - pos = line at the top of the gel - agglutinated RBC (pos) do not migrate through the gel and form a band at the top of the gel column - non-agglutinated cells (neg test result) DO migrate through gel and form a button at bottom of the gel column |
|
|
major cross-match
|
washed donor RBC + recipient plasma
takes 1-1.5 hrs if agglutination = don't use - person doing test must know their shit can be done in test tube, on slide, with gel kit |
|
|
major vs minor incompatibility
|
maj
- not safe to give minor - not ideal but could be okay with minor rxn |
|
|
minor cross match
|
donor plasma + recipient RBC
look for agglutination |
|
|
when can you not do a crossmatch
|
with IMHA
|
|
|
cross matching compatibility
|

|
|
|
in clinical small animal practice you will perform ______ (blood typing/ cross matching/ both)
|
blood typing
|
|
|
in small animal clinical practice, what species can get transfusion without typing/ cross-matching
|
dogs (1 time)
cats need typing and cross-matching prior to transfusion |
|
|
true or false
a patient could still have an adverse reaction despite typing and cross-matching |
true
|
|
|
true or false
i am sick of making clin path flashcards |
true
|
|
|
how do animals get sensitized to blood group antigens
|
transfusion of whole blood or packed RBC
pregnancy (exposure of antigen neg dam to her fetus' antigen pos blood via transplacental hemorrhage) vaccination with certain vaccines - ex Anaplasma vaccines that contain RBC membranes |
|
|
neonatal isoerythrolysis refers to
|
hemolytic anemia occurring in a neonate that acquired antibodies against its own RBC from its dam (via colostrum ingestion)
|
|
|
pathogenesis of NI
|
antigen neg dam bred to antigen pos sire
fetus expresses sire's antigen dam exposed to fetal blood during gestation dam makes antibodies to antigen she doesn't have neonate is born neonate ingests colostrum containing those antibodies neonate develops hemolytic anemia |
|
|
NI can occur in
|
type A and type AB kittens born to type B queens
Type Qa foals born to Type Qa neg mare (or Aa foal to Aa neg mare) only occurs in puppies born to bitch that was transfused prior to whelping in cattle occurs only in calves born to a cow that was previously given a RBC membrane containing vaccine |
|
|
DEA refers to
|
dog erythrocyte antigen system used to classify canine blood groups
|
|
|
canine blood transfusion med
|
dogs can develop antibodies against any blood group antigen but only DEA 1.1 is impt
b/c most antigenic and most critical often positive for mult DEA antigens |
|
|
where to alloantibodies come from
|
naturally occurring
acquired (sensitized) |
|
|
blood groups are impt in
|
transfusion med
pathogenesis of NI verify parentage for pedigree records and breeding registries |
|
|
what is a universal blood donor
|
individual having minimallly antigenic blood that could (in theory) be given to any individual of the same spp with low risk of adverse effects (O- humans)
universal donors highly desirable |
|
|
what is a universal recipient
|
an individual with mult blood group antigens that could (in theory) receive blood from any other individual of the same spp with low risk of adverse effects (type AB+ humans)
these guys lucky |
|
|
animals having antibodies to a particular blood group antigen may experience an adverse rxn (such as ______) if exposed to that antigen
|
hemolysis and/or anaphylaxis
|
|
|
which blood type is unable to be tested for (canine)
|
DEA 6
|
|
|
type AB cats can be considered universal recipients of
|
type A, B or AB packed RBC
not universal recipients for whole blood ro plasma |
|
|
in equine what are the most antigenic blood types (most resp for NI)
which are impt in transfusion med |
NI
- Aa - Qa transfusion med - Aa - Ac - Ca - Qa |
|
|
pretransfusion testing is most relevant to _____
|
RBC
the transfusion of whole blood or packed RBC |
|
|
goals of pretransfusion testing are
|
confirm blood type (blood typing)
determine donor and recipient compatibility (cross-matching) |
|
|
the end point (positive result) of blood typing is
cross matching |
endpoint of both is macroscopically visible agglutination of RBCs w/in seconds to minutes after reagents are mixed
no agglutination = neg in blood typing - RBC agglutination is caused by interactions b/w patients RBC and test kit reagents (antiserum or lectins that react w/ blood group) cross matching - agglutination is caused by antigen-antibody interactions b/w RBC and plasma (or serum) |
|
|
blood typing is performed using what sample
cross matching? |
typing
- EDTA anticoagulated blood matching - EDTA blood sample from patient and bag of whole blood or packed RBC from donor |
|
|
how do you store blood samples for transfusion use
|
4C
|
|
|
what diseases cause difficulties in blood typing/ crossmatching and why
|
pt with marked RBC rouleaux (some animals with systemic inflammation)
agglutination due to dz (IMHA) leavve this to laboratories with specially trained med techs |
|
|
2 types of commonly used commercially available blood typing test kits in the US
|
DEA 1.1 antigen (dogs)
type A & B (cats) in the form of cards and gels |
|
|
typing cards accurately identify (dogs)
|
DEA 1.1 +
DEA 1.2 pos may have weak pos rxns (can misclassify as DEA 1.1+) |
|
|
typing cards accurately ID (cats)
|
A and B cats
cats that are B or AB should undergo confirmatory testing |
|
|
gel typing accurately IDs
|
reliable in dogs and cats
|
|
|
which is better gel or card typing
|
gel is better b/c
- results easier to interpret - gel fixes agglutination rxn (so can view over a longer period of time) - gels can be photocopies and photocopy placed in medical record (thus can be archived) |
|
|
why do you use cross matching
|
confirm compatibility
investigate cause of adverse transfusion rxn |
|
|
what is impt about cross matching
|
it does not guarantee normal donor RBC survival in recipient and do not complete eliminate risk of adverse transfusion rxn
focuses on RBC so doesn't prevent adverse leukocyte or platelet rxns |
|
|
know the tranfusion blood components and their indications (whole blood vs packed RBC vs fresh frozen plasma, etc.)
|

|

