![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
129 Cards in this Set
- Front
- Back
|
Define Epidemiology |
The study of patterns of health and disease in populations and the factors that influence these patterns. - includes dead, sick and healthy of both populations, individuals, and body systems |
|
|
What are the uses of epidemiology? |
- investigation and control of a disease (cause known or unknown) - identification of the cause of a disease and its risk factors - determine the origin of a disease - study the possible outcomes of disease - plan and assess control programs - assess the magnitude of impact of a disease - analyze the costs and benefits of alternative control programs |
|
|
How does epidemiology interact with other medical disciplines? |
it complements other disciplines by providing the means to describe disease patterns, which helps plan effective treatments and control strategies |
|
|
What are the different approaches to epidemiology? |
- descriptive - experimental - analytic - theoretical
|
|
|
Describe descriptive epidemilogy |
Observations are used to describe patterns of disease occurrence and hypothesize what are the determinants of the disease |
|
|
What questions does descriptive epidemiology attempt to answer |
- What is the disease? - Who is affected? - where does it occur? - When does it occur? |
|
|
What is experimental epidemiology? |
Designs experiments to test they hypotheses developed by descriptive epidemiology |
|
|
What is analytic epidemiology? |
Collects and analyzes data used to test the hypotheses of descriptive epidemiology |
|
|
What question(s) does analytic epidemiology attempt to answer? |
Why is the disease occurring? How does the disease occur/spread? |
|
|
Describe theoretical epidemiology |
investigates patterns of disease occurrence using mathematical models |
|
|
What 3 things make up the epidemiological triad? |
-environment - agent - host |
|
|
Define determinants of disease |
factors that when altered produce a change in the frequency or characteristics of disease |
|
|
What are the 3 types of determinants of disease? |
- primary and secondary - intrinsic and extrinsic - determinants associated with host, environment, and agent |
|
|
Differentiate between primary and secondary determinants of disease. |
-primary: factors whose variations have major effects on inducing disease
- secondary: predisposing, enabling, or reinforcing factors |
|
|
Differentiate between intrinsic and extrinsic determinants of disease |
intrinsic: internal factors of the host (genetics)
extrinsic: external to the host (trauma, climate) |
|
|
What is the significance of the web of causation? |
- there is no single cause for a disease - many different factors interact to cause a disease and the web of causation shows how these factors interact |
|
|
What is herd immunity? |
a form of immunity that occurs when the vaccination of a significant portion of a population provides a measure of protection for individuals who have not developed immunity |
|
|
infection |
entry and development or multiplication of an infectious agent in the body |
|
|
contamination |
the presence of infectious agents on the exterior (or interior) surface of the body |
|
|
pollution |
presence of offensive, but not infectious, matter in the environment |
|
|
incubation period |
the time between exposure to a pathogenic organism and when symptoms are first apparent |
|
|
induction period |
interval between exposure to a harmful chemical and resultant disease |
|
|
reservoir |
any living organism or inanimate matter in which an infectious agent normally lives and multiplies, where it maintains and perpetuates itself, and form which it can be transmitted |
|
|
vector |
an organism or object that facilitates the transfer of disease
|
|
|
differentiate between a biological and mechanical vector |
- biological- part of the agents life cycle occurs within the vector -mechanical- the vector serves only as physical transport of the pathogen |
|
|
pathogenicity |
the power of an agent to produce clinical disease |
|
|
virulence |
the severity of disease produced by an agent (# of deaths/ # infected) |
|
|
horizontal transmission |
from one member of a population to another |
|
|
direct transmission |
disease is spread through physical contact with another infected individual or fluid from an infected individual (while on the individual) |
|
|
Indirect transmission |
disease is spread through contact with infected intermediate vehicles |
|
|
Determine if each of the following is an example of direct or indirect transmission: - airborne - shared water source - kissing - contaminated food - STD |
- airborne: indirect - water source: indirect - kissing: direct - contaminated food: indirect - STD: direct |
|
|
vertical transmission |
transmission from mother to offspring |
|
|
What are the 3 types of biological vectors? |
- propagative - developmental - cyclopropagative |
|
|
propagative biological vector |
multiplication of agent occurs in vector |
|
|
developmental vector |
an essential phase of the development of the agent occurs in the vector |
|
|
cyclopropagative |
both development and propagations occur in the vector |
|
|
Endemic |
a disease that occurs constant at a constant frequency in a certain population |
|
|
epidemic |
a disease occurring at a higher than normal frequency in a population |
|
|
pandemic |
epidemic that crosses international boundaries |
|
|
sporadic occurrence of disease |
disease occurs irregularly and haphazardly |
|
|
point source epidemic |
a common source for infection where the period of exposure is brief |
|
|
propagated epidemic |
an epidemic caused by an infectious agent in which initial cases spread the agent and infect susceptible individuals. - depends on both agent and host factors |
|
|
hyperendemic |
disease is constantly present at a high level |
|
|
hypoendemic |
disease is constantly present at a low level |
|
|
holoendemic |
disease is present at a high level in young and a low level in old due to immunity that developed due to high exposure when young |
|
|
What are the steps to construct an epidemic curve? |
1. identify the date of onset 2. set the time interval (1/3 or less of incubation period) 3. create x axis lead and end periods (2x the incubation period) 4. draw tick marks and label time intervals 5. plot cases 6. mark critical events |
|
|
What is the importance of having lead and end periods on an epidemic curve? |
the show that the disease truly was not present before the index case and that it has been completely resolved |
|
|
What are some examples of critical events that should be marked on an epidemic curve? |
- introduction of new animals - new food - major weather events - transport/travel - new medications or vaccines |
|
|
outbreak |
an epidemic that is limited to a localized increase in the incidence of disease |
|
|
Outbreak investigation |
Systemic procedure to identify causes and sources of epidemics. |
|
|
What things does an outbreak investigation attempt to identify? |
- the problem - steps to deal with the problem - how to prevent the problem happening again |
|
|
What are the steps involved in an outbreak investigation? |
1. determine the existence of an outbreak and if any action should be taken 2. confirm the diagnosis 3. define a "case" and count the "cases" 4. describe the patterns in terms of time, place, and individual to determine who is at risk 5. determine the magnitude of the problem 6. develop and test hypothesis and make recommendations for corrective action 7. compare results with established rates
once outbreak has been resolved 8. plan a more detailed and systematic study 9. prepare a written report 10. execute control and prevention measures |
|
|
In an outbreak investigation what should you consider when determining if action should be taken? |
- severity of the illness - potential for spread - politcal considerations - public relations - availability of resources |
|
|
In an outbreak investigation how can you determine if an outbreak really exists? |
compare the number of cases now to the number during a different period of time.
- you must take into consideration any changes that might have occurred involving diagnosis or disease reporting |
|
|
What would you use to describe patterns of time in an outbreak investigation? |
an epidemic curve |
|
|
What would you use to describe patterns of place in an outbreak investigation? |
a distribution map |
|
|
In an outbreak investigation, how would you determine the magnitude of the problem? |
calculate crude and factor specific attack rates |
|
|
How do you determine an attack rate? |
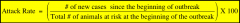
build an attack rate table then calculate the rate using this formula (click it to see bigger) |
|
|
What should your hypothesis during an outbreak investigation address? |
- the kind of epidemic (point vs propagated) - the source of the epidemic - the possible mode of spread - the exposure that caused the disease |
|
|
prevention |
employing techniques to prevent the occurrence of a disease or limit its progression and/or severity |
|
|
control |
reduction of disease prevalence to a level that is no longer a major health and/or economic problem |
|
|
Eradication |
total elimination of a disease due to the removal of its cause |
|
|
what are the 3 types of prevention? |
- primary: prevent exposure or development of disease - secondary: detect disease as early as possible before clinical disease occurs - tertiary- administer treatment following clinical signs to stop further spread |
|
|
What are the methods of disease control? |
slaughter quarantine reduction of contact chemical use modifications of host resistance environment/management control education biological control |
|
|
slaughter |
the deliberate killing of infected animals or those suspected of being infected in order to top the spread of disease
|
|
|
differentiate between selective and complete depopulation |
selective- test and cull, good to prevent slow spreading disease
complete depopulation- culling of entire population in order to prevent rapidly spreading diseases or disease with serious consequences
|
|
|
quarantine |
physical separation of infected or potentially infected animals from the healthy population
- used to detect disease |
|
|
Reduction of contact |
prevent contact between infected and between infected and non-infected animals - spacial or temporal |
|
|
chemical use for control |
-disinfectants: reduce transmission of infectious agents
- insecticides: vector control
- antimicrobials: treat or prevent disease |
|
|
how can host resistance be modified to control disease? |
- acquired- vaccination - innate- colostrum |
|
|
What are 3 methods of strategic vaccine control? |
- ring - barrier - suppressive |
|
|
What is ring vaccination? |
vaccinate all susceptible individuals in the areas surrounding an outbreak to prevent the further spread of the disease |
|
|
what is barrier vaccination? |
vaccinating all individuals surrounding an area that is free of disease to prevent entry of disease into that area |
|
|
What is suppressive vaccination technique? |
vaccinating enough animals to achieve herd immunity |
|
|
What is environmental/management control of disease? |
altering one of the causal web factors to limit disease spread |
|
|
What is biosecurity? |
the use of management practices to reduce spread of infectious agents within food animal units |
|
|
what are some biosecurity techniques? |
-cleanliness - disinfection - reduction of exposure - limiting visitors - adequate training - tracing animals |
|
|
What is the difference between quarantine and isolation? |
isolation separates clinically ill animals to prevent the spread of disease while quarantine separates potentially ill animals to diagnose disease |
|
|
What is host immunity? |
the ability of individual animals to resist infection, or resist disease if infected |
|
|
What is contact rate? How does this affect the spread of infection? |
contact rate is the frequency of contact between susceptible individuals and the causative agent. the higher the contact rate the more easily the disease will spread but if contact rate is low enough it may fail to become established |
|
|
Determinants of disease: What are some agent factors |
1. host range 2. infectivity 3. infectious dose 4. viability 5. pathogenicity 6. virulence 7. immunogenicity |
|
|
determinants of disease: host factors |
1. genotype 2. age 3. sex 4. species and breed 5. immunological status 6. occupation 7. size and conformation 8. social and ethological 9. coat color |
|
|
Determinants of disease: environmental factors |
1. location 2. climate (micro and macro) 3. husbandry (housing, nutrition, management) |
|
|
What is the beginning and end of the information cycle? |
the clinical veterinary practice - it raises the questions to be answered by experimentation and uses the information from this research to practice |
|
|
What are the common information resources available in veterinary medicine? Which is the best option? |
- lecture notes- good for mechanisms and facts, but can be out of date - expert opinion- biased and may not be backed up by empirical evidence - textbooks- like expert opinion but more out of date - scientific journals- best option because they are peer review and contain evidence based research |
|
|
What is evidence based veterinary medicine? |
combining clinical experience, relevant scientific, evidence, and individual patient situations to make the best clinical decisions possible |
|
|
What are the 5 steps of EBVM? |
1. ask an answerable question 2. find the best available evidence 3. critically appraise the evidence 4. apply the evidence 5. implement and evaluate the outcomes |
|
|
What is the difference between "just in case" and "just in time" knowledge? |
- just in case is the traditional approach to continuing education where research is done about topics that might be relevant in the future and information is hopefully stored where you can later access it
- just in time knowledge is using EBM to research relevant information about a clinical question when you need it. This results in more up to date information being found and less time trying to remember what you learned previously |
|
|
In each of the following pairs, decide which characteristic best fits evidence based medicine: - subjective or clinical judgement - reliance on authority or quality resources - empirically supported or pathophysiological rationale |
clinical judgement reliance on quality resources empirically supported rationale |
|
|
What does PICO stand for? When is it used? |
Patient/population intervention comparison outcome
used to formulate a clinical question that can be researched |
|
|
Hierarchy of evidence |
a spectrum of potential sources with the sources that most likely provide the best evidence at the top |
|
|
What are the criteria for good evidence? |
- scientific soundness - clinical usefulness |
|
|
internal validity |
the extent to which the design and conduct of an experiment eliminates the possibility of systemic errors |
|
|
external validity |
the extent to which the results of a study apply to your patient |
|
|
Host immunity is dependent on what? |
nature of agent challenge dose environmental factors |
|
|
rate of infections disease spread in a population depends on what? |
- characteristics of infectious agent - host immunity of the animals int eh population - population structure - population dynamics - contact rate |
|
|
What are the sub disciplines of epidemiology? |
- clinical: focuses on diagnosis and prognosis - computational: uses computer science to study epidemiology - genetic: study of disease in related individuals - field: involves visiting the field to study diseases that require rapid action - participatory: uses local knowledge to help in the study of disease - molecular: uses molecular techniques to study disease causing agents |
|
|
What are 3 categories of genetic diseases? |
- mendelian- totally genetic - chromosomal- totally genetic - multifactoral- partially genetic |
|
|
Sex -linked inheritance |
DNA responsible for the disease is carried on either the X or Y chromosome
- hemophilia A |
|
|
Sex-limited inheritance |
DNA does not occur on sex chromosome but disease only occurs in one sex due to other factors.
- metritis only in females - orchitis only in males |
|
|
sex- influenced |
disease/condition can occur in either sex but is preferentially expressed in one sex over the other (the threshold for expression is lower in one sex)
- baldness |
|
|
associated factors of disease |
factor is related to the cause of disease but is not itself the case of disease
- rats were associated with the black plague because they harbored fleas which were the actual means of spread |
|
|
nidus |
a center in which infection settles and from which infection spreads
a localized reservoir or the environment in which the reservoir is found |
|
|
source of infection |
the person, animal, object, or substance from which an infectious agent passes directly to a susceptible host.
reservoirs are sources of infection but not all sources of infection are reservoirs (something my harbor and transmit and infectious agent but the agent may not be able to propagate there so is therefore not a reservoir) |
|
|
carrier |
an infected person or animal that sheds pathogenic or potentially pathogenic organisms in the absence of discernible clinical disease and serves as a source of infection |
|
|
healthy carriers |
shed agent but never develop disease |
|
|
inapparent infeciton |
infection that does not cause disease |
|
|
incubatory carriers |
shed the agent prior to showing clinical signs |
|
|
convalescent carriers |
shed agent for a short period of time following recovery from disease |
|
|
intermittent carriers |
intermittently shed agent for a moderate period following recovery from disease |
|
|
chronic carrier |
shed agent for an extended period following recovery |
|
|
differentiate between primary and secondary vehicles of disease transfer. |
primary vehicles are the tissues on which the infectious agent leaves one host and can infect another. (saliva, urine, blood)
secondary vehicles are intermediate inanimate objects that can become contaminated with primary vehicles and from which the disease can be transmitted (grass/ pasture, food, toys) |
|
|
What is the difference between a vehicle and fomite? |
they are both anything on which an infected individual can leave a residue of infectious/contagious pathogens and that can transfer the pathogen
Vehicles include food, water, and bodily secretions while fomites do not.
all fomites are vehicles but not all vehicles are fomites |
|
|
what are the 4 forms of airborne transmission? |
- dust (requires highly viable microbes and can travel long distances in wind) - expiratory droplets (require close contact) - droplet nuclei (can spread long distances) - vapors and gases (requires close contact) |
|
|
what are 3 methods of horizontal transmission? |
- direct - indirect - iatrogenic |
|
|
What are the methods of indirect transmission? |
- vehicles/fomites - airborne - ingestion (food or water) - vectors |
|
|
What are the methods of vertical transmission? |
- hereditary - acquired in utero - acquired during birth - through milk - through colostrum |
|
|
definitive host |
host in which organism undergoes its sexual phase of reproduction |
|
|
primary or maintenance host |
host that maintains infection in an endemic area of infection |
|
|
paratenic host |
a host in which an agent is transmitted mechanically (does not undergo any part of lifecycle) |
|
|
intermediate host |
host in which an infectious agent undergoes some development |
|
|
amplifier host |
host in which concentration of agent becomes high enough that it can be picked up and spread by vectors |
|
|
link host |
host at links two different host species |
|
|
effective contact |
the conditions under which infections will occur. Depends on: - stability of organism - portal of exit from reservoir - portal of entry into new host |
|
|
What are factors that affect the shape of an epidemic curve and how do they affect it? |
1. incubation period: longer= longer propagation period
2. infectivity of agent: affects amplitude
3. proportion of susceptible hosts: affects amplitude |
|
|
threshold level of disease |
minimum number of susceptible animals necessary for a disease to be spread and maintained in a population |
|
|
What are features of an epidemic curve of a point source epidemic? |
- rapidly ascending and descending limbs - compressed in time - approaches symmetry at average incubation period |
|
|
What are features of an epidemic curve of a propagating epidemic? |
- gradually ascending limb - tendency to plateau |
|
|
What are the trends in temporal distribution of disease? |
- short-term: epidemics - cyclical trends: repeating patterns of disease occurrence (e.g. seasonal) - secular: long term increases or decreases in disease occurrence in addition to small short term changes |

