![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
What is the definition of Ischemic Heart Disease (IHD)?
|
Imbalance between supply and demand for oxygen and nutrients and removal of metabolites
|
|
|
What is the difference between ischemia and hypoxemia? Which is worse?
|
- Ischemia causes a lack of perfusion, prevents delivery of nutrients (in addition to oxygen) and removal of metabolites
- Hypoxemia is just a lack of delivery of oxygen - Ischemia is worse than hypoxemia |
|
|
What is the leading cause of death and disability in the USA?
|
Ischemic Heart Disease (IHD)
|
|
|
How has the death rate from Ischemic Heart Disease (IHD) changed over time? Why?
|
- Decreased since 1960s
- Preventative measures against development of atherosclerosis (smoking, cholesterol, HTN, lifestyle) - Therapeutic advances (medical and surgical) |
|
|
What is the cause of Ischemic Heart Disease (IHD)?
|
- ≥ 90% atherosclerotic narrowing
- Reduced coronary blood flow - Other causes: ↓ systolic BP, vasculitis, structural anomalies, severe HTN, diminished oxygenation, or diminished oxygen-carrying capacity |
|
|
What are some causes of decreased blood flow (leading to Ischemic Heart Disease (IHD))?
|
- Fixed atherosclerotic narrowing
- Acute plaque change - Thrombosis overlying ruptured plaque - Vasospasm |
|
|
What percentage of the lumen needs to be compromised to cause symptoms in Ischemic Heart Disease (IHD)?
|
- >70% narrowed → symptomatic ischemia w/ EXERCISE
- >90% stenosis → ischemia at REST |
|
|
What are the most commonly affected Coronary Arteries?
|
1. First several cm of Left Anterior Descending (LAD) = widow maker
2. Left Circumflex (LCX) 3. Entire length of R Coronary Artery (RCA) |
|
|
How is the effect of a fixed obstruction to blood flow modified?
|
Collateral circulation - if there is time to adapt, collaterals can help provide blood supply to heart, but if it is an acute obstruction, no help
|
|
|
What are the characteristics and outcomes of an acute plaque change in Ischemic Heart Disease (IHD)?
|
- Unpredictable, abrupt conversion of stable plaque to an unstable athero-thrombotic lesion
- E.g., Rupture / fissures / ulcerations - expose underlying thombogenic substances (leads to more clotting) - E.g., Hemorrhage into atheroma - expands plaque and narrows lumen - Results in acute coronary syndrome: MI, unstable angina, sudden cardiac death |
|
|
What intrinsic factors can contribute to an acute plaque change?
|
- Large areas of foam cells / lipid (lipid core)
- Thin fibrous cap - Most dangerous lesions are moderately stenotic, lipid rich atheromas (soft core) - Abundant inflammation - Few smooth muscle cells - Mechanical stress (at junction of fibrous cap and adjacent normal wall) |
|
|
What is the most dangerous size of lesion / stenosis for an acute plaque change? Why?
|
- Moderately stenotic (50-75%)
- They are getting beaten by turbulent blood flow which can predispose to an acute plaque change - A larger plaque would not be affected by turbulent flow because there is not room for turbulence - A smaller plaque is obviously less troublesome |
|
|
What extrinsic factors can contribute to an acute plaque change?
|
Adrenergic stimulation:
- Upon awakening - Emotional |
|
|
How does a coronary thrombosis cause a decrease in blood flow?
|
Thrombosis can partially or totally superimpose on a partially stenotic plaque
|
|
|
What are the possible outcomes of a coronary thrombosis?
|
- Total occlusion → Acute Transmural MI or Sudden Death
- Incomplete occlusion → Mural Thrombus → Unstable Angina, acute subendocardial infarction, sudden death or may emboli into more distal coronary artery |
|
|
How does vasoconstriction cause a decrease in blood flow? Outcomes?
|
- Compromises lumen size and increases mechanical forces that contribute to plaque rupture
- Leads to severe but transient reduction in coronary blood flow |
|
|
What stimulates vasoconstriction of coronary arteries?
|
- Adrenergic agonists in circulation
- Locally released platelet contents - Endothelial dysfunction leading to impaired secretion of endothelial relaxing factors - Mediators released from mast cells |
|
|
What is the progression of acute coronary syndromes?
|

1. Normal
2. Atherosclerosis → fixed coronary obstruction → Typical Angina 3. Plaque Disruption → healing leads to larger / severe fixed coronary obstruction → Chronic Ischemic Heart Disease 4. Thrombus (either mural or occlusive) - Mural: variable obstruction → Unstable Angina, Acute Subendocardial MI, or Sudden Death - Occlusive: complete obstruction → Acute Transmural MI or Sudden Death |
|
|
What are the clinical syndromes / outcomes of Ischemic Heart Disease (IHD)?
|
- Angina pectoris (chest pain)
- Myocardial infarction - Chronic ischemic heart disease - Sudden cardiac death |
|
|
What is the definition of Angina Pectoris?
|
- Manifestation of Ischemic Heart Disease (IHD)
- Paroxysmal (sudden) and recurrent attacks of chest pain caused by transient MI - Lasts 15 seconds to 15 minutes - No cellular necrosis (no lasting damage) |
|
|
What are the three patterns of Angina Pectoris?
|
- Stable
- Prinzmetal - Unstable |
|
|
What are the characteristics of Stable Angina Pectoris?
|
- Produced by physical activity or emotional excitement
- Attributed to chronic stenosing coronary artery syndrome - Demand for O2 and nutrients exceeds supply |
|
|
What are the characteristics of Prinzmetal Angina Pectoris?
|
Due to coronary artery spasm at rest
|
|
|
What are the characteristics of Unstable Angina Pectoris?
|
- Occurs w/ progressively increasing frequency and progressively less effort
- Often at rest and of prolonged duration - Induced by disruption of plaque w/ superimposed partial thrombosis - Often prodrome (early symptom) of acute MI |
|
|
What happens in a Myocardial Infarction (MI)?
|
Death of cardiac muscle d/t ischemia
- 90%: acute plaque change results in thrombus and occlusion of coronary artery - 10%: vasospasm, emboli, or unexplained |
|
|
What are the risk factors for a Myocardial Infarction (MI)?
|
- Increasing age
- M > F (premenopausal) - HTN - Cigarettes - DM - Increased cholesterol and/or lipids |
|
|
What are the two types of Myocardial Infarctions (MI)?
|
- Transmural
- Subendocardial |
|
|
What are the characteristics of a Transmural Myocardial Infarction (MI)?
|
- Full thickness of ventricular wall
- Confined to distribution of one vessel - Fixed coronary obstruction with superimposed acute plaque change and complete obstructive thrombosis * Localized obstruction in flow * |
|
|
What are the characteristics of a Subendocardial Myocardial Infarction (MI)?
|
- Necrosis limited to inner 1/3
- May extend laterally beyond perfusion of one vessel - Fixed coronary obstruction w/ acute plaque change - Non-occlusive thrombus or lysis of thrombus or hypotension * Global decrease in flow * |
|
|
Which kind of MI causes a localized obstruction in flow as opposed to a global decrease in flow?
|
- Localized: Transmural
- Global: Subendocardial |
|
|
Which kind of MI causes necrosis limited to inner 1/3 and which causes a full thickness injury?
|
- Global: Subendocardial
- Full thickness: Transmural |
|
|
What is the response to a Myocardial Infarction (MI)? Timeline?
|
- Immediately: loss of blood supply (reversible damage in early stages)
- 60 sec of ischemia: loss of contractility (may precipitate acute heart failure) - 20-40 minutes: irreversible damage (coagulative necrosis) - 3-4 hours: early thrombolytic therapy → reperfusion and limiting of size of infarct - Later: arrhythmias (induced by myocardial irritability secondary to ischemia/infarction - ventricular fibrillation) → sudden death |
|
|
How much time of ischemia is necessary to cause loss of contractility in a Myocardial Infarction (MI)?
|
60 seconds
|
|
|
How much time does it take to cause irreversible damage (coagulative necrosis) in a Myocardial Infarction (MI)?
|
20-40 minutes
|
|
|
How soon should early thrombolytic therapy occur? Benefits?
|
- Hopefully within 3-4 hours
- Reperfusion - Limits size of infarct |
|
|
What are some outcomes that can be caused by myocardial irritability secondary to ischemia and infarction?
|
- Arrhythmias (eg ventricular fibrillation)
- Can lead to sudden death |
|
|
How does the progression of necrosis occur in a Myocardial Infarction (MI)?
|

- Endocardium is furthest from coronary artery so is first to necrose
- Last epicardium (closest to coronary artery) - Occurs in zone / area supplied by coronary artery |
|
|
Which coronary arteries are involved in Myocardial Infarctions (MI)? How frequently?
|
- LAD: most often (40-50%)
- RCA: next most often (30-40%) - LCA: least common (15-20%) |
|
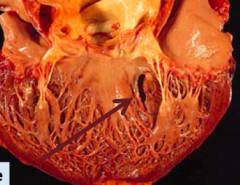
What kind of infarct is this? Cause?
|
- Regional sub-endocardial infarct
- Non-transmural infarct - Cause: Transient / partial obstruction |
|
What kind of infarct is this?
|
- Circumferential sub-endocardial infarct
- Non-transmural infarct - Cause: Global hypotension |
|
What kind of infarct is this?
|
- Micro-infarcts
- Non-transmural infacts - Cause: small intramural vessel occlusions |
|
|
Morphologically, what happens in the first 12 hours of a Myocardial Infarction?
|
- Not apparent
- Tetrazolium stain shows pale areas 2-3 hours post-occurrence |
|
|
Morphologically, what happens 12-24 hours after a Myocardial Infarction?
|
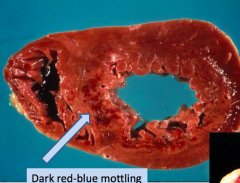
Dark red-blue mottling (due to stagnant blood)
|
|
|
Morphologically, what happens 1-14 days after a Myocardial Infarction?
|
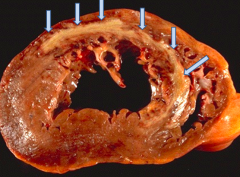
- Early: sharply defined yellow-tan area
- Late: still yellow-tan centrally but with hyperemic peripheral zone |
|
|
Morphologically, what happens >2 weeks after a Myocardial Infarction?
|
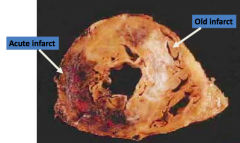
Gray-white scar begins to form
|
|
|
Histologically, what happens in the first 24 hours of a Myocardial Infarction?
|
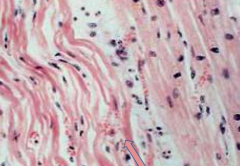
- Presence of wavy fibers
- Coagulative necrosis |
|
|
Histologically, what happens 12 hours - 7 days after a Myocardial Infarction?
|
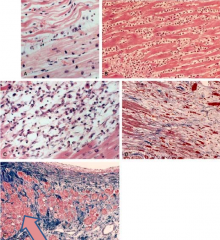
- Coagulative necrosis becomes well-established and ongoing
- Initially pyknotic nuclei, hyper-eosinophilic myocytes - Followed by neutrophils (max 1-3 days), loss of nuclei and striations - By 7 days, macrophages are at border |
|
|
Histologically, what happens 7-14 days after a Myocardial Infarction?
|
- Granulation tissue well-established
- Collagen begins to deposit |
|
|
Histologically, what happens >14 days after a Myocardial Infarction?
|
- Progressively more collagen deposition
- Eventually dense fibrous scar |
|
|
When does reperfusion injury occur?
|
After thrombolysis, balloon angioplasty, or bypass grafts
|
|
|
How soon does reperfusion need to occur to prevent necrosis from an MI?
|
Within 20 minutes
|
|
|
What is the microscopic evidence of reperfusion injury? Why?
|
Microscopically: necrosis with contraction bands - permanent (due to influx of Ca2+)
|
|
|
What is the cause of reperfusion injury?
|
- Oxygen free radicals released from leukocytes
- Microvascular injury causes hemorrhage and endothelial swelling that occludes capillaries (no flow) - Platelet and complement activation |
|
|
What are the clinical features of MI?
|
- Chest pain (severe, crushing, substernal)
- Pain may radiate into left arm, neck, jaw, epigastrium - Lasts several minutes to hours - No relief by nitroglycerin or rest - Rapid weak pulse - Diaphoresis (sweating) - Dyspnea d/t pulmonary edema - 10-15% without symptoms |
|
|
What are the diagnostic features for evaluating a possible MI?
|
- ECG patterns
- Elevated cardiac enzymes (MB-CK and Troponins), C-reactive protein |
|
|
How does nitroglycerin and rest help someone having an MI?
|
No relief
|
|
|
What are the complications of an MI?
|
- Contractile dysfunction (proportionate to damage)
- Cardiogenic shock (pump failure) - Arrhythmia (early, may lead to sudden death) - Myocardial rupture (3-7 days) - Pericarditis (2-3 days) - Mural thrombus and thromboembolism - Ventricular aneurysm (late) - Papillary muscle dysfunction (secondary to scarring/fibrosis) - Progressive heart failure (late) |
|
|
How common is cardiogenic shock (pump failure) in an MI? What is it associated with?
|
- 10-15%
- Associated with damage to 40% or more of LV - Correlates w/ size of infarct |
|
|
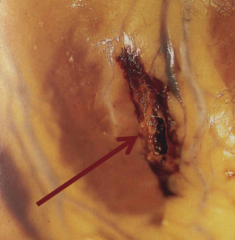
When does myocardial rupture occur after an MI? Where can it occur and what are the outcomes of those locations?
|
- 3-7 days post-MI
- Free wall: hemopericardium, tamponade, aneurysm - Ventricular septum: L → R shunt - Papillary muscle: mitral regurgitation |
|
|
What are the possible outcomes of a myocardial rupture of the free wall? When does this occur?
|
- Hemopericardium (blood in the pericardial sac of the heart)
- Tamponade (compression of the heart by an accumulation of fluid in the pericardial sac) - Aneurysm (excessive, localized enlargement) - 3-7 days post-MI |
|
|
What are the possible outcomes of a myocardial rupture of the ventricular septum? When does this occur?
|
- Left → Right shunt
- 3-7 days post-MI |
|
|
What are the possible outcomes of a myocardial rupture of the papillary muscle? When does this occur?
|
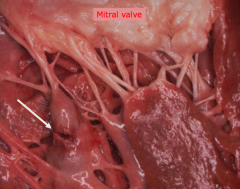
- Mitral Regurgitation
- 3-7 days post-MI |
|
|
When does pericarditis occur? What is it?
|
- 2-3 days post-MI
- Inflammation of the pericardium of the heart |
|
|
What are some late complications of MI?
|
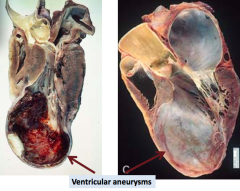
- Ventricular aneurysm
- Progressive heart failure |
|
|
What is a mural thrombus?
|
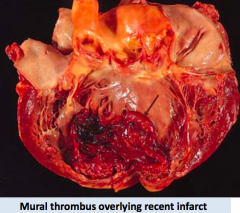
- Mural thrombi are thrombi adherent to the vessel wall
- They are not occlusive and affect large vessels, such as heart and aorta |
|
|
What is the prognosis of acute MI?
|
- Depends on infarct size, site, and transmural extent
- Long-term prognosis depends on quality of LV function and extent of vascular obstruction |
|
|
What are the morphological characteristics of Chronic Ischemic Heart Disease?
|
- Enlarged heavy heart
- LV hypertrophy and dilation (blood back up leads to dilation) - Coronary AS - Scars - Subendocardial myocyte vacuolization |
|
|
What kind of patient gets chronic ischemic heart disease?
|
Elderly patient w/ progressive heart failure d/t ischemic myocardial damage
|
|
|
What are the two causes of Chronic Ischemic Heart Disease?
|
- Post-infarction cardiac decomposition (exhausts remaining hypertrophic fibers)
- Severe coronary artery disease w/o infarction but w/ myocardial dysfunction |
|
|
What happens in Sudden Cardiac Death?
|
- Unexpected death from cardiac causes, early after or without onset of symptoms
- Caused by lethal arrhythmia (asystole or V fib) |
|
|
What is the most common cause of Sudden Cardiac Death?
|
- Lethal arrhythmia (asystole or V fib)
- Most often d/t ischemic heart disease |
|
|
What percentage of people who die from sudden cardiac death had ischemic heart disease?
|
80-90%
|
|
|
What are the non-atherosclerotic causes of Sudden Cardiac Death?
|
- Hypertrophy
- Cardiac conduction system abnormality - Mitral valve prolapse - Congenital abnormality - Myocarditis - Cardiomyopathy - Pulmonary HTN |
|
|
What are the morphological characteristics of Sudden Cardiac Death?
|
- Coronary atherosclerosis
- Acute plaque change - MI - Scars from old MIs - Pathology associated with non-atherosclerotic causes |
|
|
What are the potential outcomes of coronary artery disease progression?
|
- Immediate myocardial ischemia
- Acute plaque change → coronary artery thrombosis → myocardial ischemia of increased severity and duration |
|
|
What can precipitate a myocardial infarction?
|
- Coronary Artery Disease →
- Acute plaque change; coronary artery thrombosis → - Myocardial ischemia of increased severity and duration → - Myocardial Infarction (MI) |
|
|
What are the outcomes of a Myocardial Infarction?
|
- Infarct healing
- Ventricular remodeling - Hypertrophy, dilation of viable muscle All progress to chronic ischemic heart disease |
|
|
What events precipitate chronic ischemic heart disease?
|
- Myocardial ischemia progression
- MI followed by infarct healing, ventricular remodeling, or hypertrophy / dilation of viable muscle |
|
|
What are the outcomes of chronic ischemic heart disease?
|
- Immediate sudden cardiac death
- Congestive heart failure → sudden cardiac death |
|
|
What can precipitate sudden cardiac death?
|
- Myocardial ischemia
- Congestive heart failure - Chronic ischemic heart disease - Myocardial ischemia of increased severity and duration - Myocardial infarction |

