![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
|
What is the function of RBCs
|
RBCs serve to transport 02 from the alveoli to tissues via the blood stream and to transport CO2 from tissue to lungs
|
|
|
What is the most likely cause of aortic stenosis in a 50yo pt?
|
Congenital bicuspid aortic valve
|
|
|
What is the function of Normal hemoglobin (Hgb) A
|
serves as a binding protein for 02 and CO2, and its affinity for 02 follows the Hgb-02 dissociation curve
|
|
|
What is the mcc of aortic regurgitation in a 70yo pt?
|
Senile or degenerative calcification
|
|
|
If a patient presents
with carbon monoxide poisoning carbon monoxide displaces 02 on Hgb, leading to insufficient delivery of 02 to tissues,what is the treatment? |
administer 100% 02 via face mask to increase the alveolar concentration of 02 and decrease the opportunities for carbon monoxide to bind to Hgb.
|
|
|
What is the classic (but rare) EKG finding in a pt with a pulmonary embolism?
|
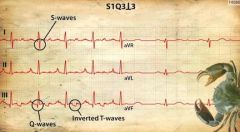
Wide S in Lead 1
Large Q & inverted T waves in lead 3 |
|
|
Normal hemoglobin and hematocrit for males and females
|
Male: 14-18 g/dL and 42%-52%
female:12-16 g/dL and 37%-47% |
|
|
What is the most likely cause of 2° hypertension if pt has:
HTN measures in arms but low BP in lower extremities |
Aortic Coarctation
|
|
|
What does low Hgb and Hct cause?
|
Low Hgb and Hct (i.e., anemia) result in insufficient supply of 02 to tissues and cause ischemia
|
|
|
What is the most likely cause of 2° hypertension if pt has proteinuria?
|
renal disease
|
|
|
What are signs of carbon monoxide poisoning
|
mental status changes
cherry-red lips, hypoxia despite normal pulse oximetry readings. |
|
|
What is the most likely cause of 2° hypertension if pt has hypokalemia?
|
hyperaldosteronism
|
|
|
Lifespan of RBCs
|
120 days.
|
|
|
What is the most likely cause of 2° hypertension if pt has tachycardia, diarrhea, heat intolerance?
|
hyperthyroidism
|
|
|
What is hemolytic anemia
|
Anemia that results when RBC lifespan is shortened and marrow production of RBCs is not capable of meeting demand for new cells
|
|
|
What is the most likely cause of 2° hypertension if pt has hyperkalemia?
|
renal failure or renal artery stenosis
|
|
|
Causes of hemolytic anemia
|
defects in RBC membrane
RBC enzyme defects hemoglobinopathies extracellular effects |
|
|
What is the most likely cause of 2° hypertension if pt has periodic sweating, tachycardia
|
pheochromocytoma
|
|
|
Symptoms of hemolytic anemia
|
possibly asymptomatic; weakness
fatigue dyspnea on exertion pallor tachycardia tachypnea increased pulse pressure possible systolic murmur jaundice severe cases may have palpitations, syncope, mental status changes, angina, chills, abdominal pain, hepatosplenomegaly, and brownish discoloration of urine |
|
|
• An elderly F with h/o cholelithiasis presents with 5 day h/o vague, recurrent abdominal pain & vomiting. What diagnosis do you immediately suspect?
|
Gallstone ileus
|
|
|
A pt presents to the ER with a very painful irreducible inguinal mass. What is the next step in management of this pt?
|
OR for surgical correction
|
|
|
What shifts Hgb-O2 dissociation curve to left
|
Metabolic alkalosis
decreased body temperature increased Hgb F |
|
|
A 4mo old child presents with nonbilious vomiting despite changing formulas from milk-based to soy-based. What is the most likely etiology?
|
Congenital pyloric stenosis
|
|
|
What shifts Hgb-O2 dissociation curve to right
|
metabolic acidosis
increased body temperature high altitude exercise |
|
|
A pt presents to the clinic for follow-up and is found to have a BP of 150/85. You note in the chart that during his last visit 1 mo ago, his BP was 145/90. What is the next step in management of this pt?
|
Recheck the BP in 2-4 wks (need 3 elevated BPs to make dx)
|
|
|
What labs in seen in hemolytic anemia
|
increased
reticulocyte ct indirect bilirubin LDH decreased Hgb Hct haptoglobin normal MCV |
|
|
What are the characteristic findings of hereditary spherocytosis?
|
1) Jaundice & gallstones
2) Splenomegaly 3) Higher incidence of pseudohyperkalemia as RBCs lyse after blood draw and intracellular potassium leaks 4) Peripheral smear reveals spherocytes 5) (+) osmotic fragility test |
|
|
What are the characteristic findings of hereditary spherocytosis?
|
Jaundice & gallstones
Splenomegaly Anemia with reticulocytosis and ↑MCHC Higher incidence of pseudohyperkalemia as RBCs lyse after blood draw and intracellular potassium leaks Peripheral smear reveals spherocytes (+) osmotic fragility test |
|
|
What is haptoglobin
|
blood plasma, haptoglobin binds free hemoglobin (Hb) released from erythrocytes with high affinity and thereby inhibits its oxidative activity. The haptoglobin-hemoglobin complex will then be removed by the reticuloendothelial system (mostly the spleen)
|
|
|
what does a left shift indicates
|
increased Hgb affinity for O2 at a given concentration
|
|
|
What is the treatment for hereditary spherocytosis?
|
Folic acid 1mg daily
pRBC transfusion in cases of extreme anemia splenectomy in moderate to severe disease |
|
|
What is the treatment for hereditary spherocytosis?
|
Folic acid 1mg daily
pRBC transfusion in cases of extreme anemia splenectomy in moderate to severe disease |
|
|
Increased body temp, acidosis, and exercise shift the hemoglobin-oxygen dissociation curve in which direction? What effect does this have on oxygen delivery to the tissues?
|
Rightward shift
Enhances O2 delivery to peripheral tissues |
|
|
Increased body temp, acidosis, and exercise shift the hemoglobin-oxygen dissociation curve in which direction? What effect does this have on oxygen delivery to the tissues?
|
Rightward shift
Enhances O2 delivery to peripheral tissues |
|
|
what does right shift indicates
|
decreased Hgb affinity for O2 at a given concentration
|
|
|
An elderly man is seen in the ER with a chief complaint of headache. Further questioning reveals that since the weather has turned cold and he had to begin using his kerosene heater, he has felt fatigued and a little nauseated along with the headache. On exam the man’s lips seem remarkably red. What do you expect the pulse ox reading to be? How will you tx?
|
Dx: Carbon dioxide poisoning
Will have normal pulse oximeter reading Tx: 100% O2, hyperbaric oxygen chamber if available |
|
|
An elderly man is seen in the ER with a chief complaint of headache. Further questioning reveals that since the weather has turned cold and he had to begin using his kerosene heater, he has felt fatigued and a little nauseated along with the headache. On exam the man’s lips seem remarkably red. What do you expect the pulse ox reading to be? How will you tx?
|
Dx: Carbon dioxide poisoning
Will have normal pulse oximeter reading Tx: 100% O2, hyperbaric oxygen chamber if available |
|
|
What is the coomb's reagent for the Coomb's test
|
IgM directed against human IgG and complement mixed with RBCs
|
|
|
How is hemolytic anemia diagnosed
|
Coombs' test
Blood smear |
|
|
Will anemia of chronic disease give a microcytic or normocytic anemia?
|
Normally anemia of chronic disease is normocytic but can be microcytic
|
|
|
Will anemia of chronic disease give a microcytic or normocytic anemia?
|
Normally anemia of chronic disease is normocytic but can be microcytic
|
|
|
In hemolytic anemia, why is the serum haptoglobin level decreased? Why is the serum lactate dehydrogenase (LDH) increased?
|
Haptoglobin binds free Hg in the blood
LDH is found inside RBCs, so when cells lyse, free LDH is released |
|
|
In hemolytic anemia, why is the serum haptoglobin level decreased? Why is the serum lactate dehydrogenase (LDH) increased?
|
Haptoglobin binds free Hg in the blood
LDH is found inside RBCs, so when cells lyse, free LDH is released |
|
|
What is found on the blood smear for hemolytic anemia
|
schistocytes (RBC fragments) spherocytes
burr cells |
|
|
25yo F is seen in the clinic with c/o fatigue and chronic joint pain. Exam and routine labs reveal a malar rash, mildly elevated temperature, and anemia. It is unclear whether this woman’s anemia is caused by autoimmune hemolytic anemia or from her recent menstruation. What test can distinguish btw possible autoimmune mediated hemolytic anemia vs other causes of anemia including non-immune mediated hemolytic anemia?
|
Direct Coombs test
|
|
|
25yo F is seen in the clinic with c/o fatigue and chronic joint pain. Exam and routine labs reveal a malar rash, mildly elevated temperature, and anemia. It is unclear whether this woman’s anemia is caused by autoimmune hemolytic anemia or from her recent menstruation. What test can distinguish btw possible autoimmune mediated hemolytic anemia vs other causes of anemia including non-immune mediated hemolytic anemia?
|
Direct Coombs test
|
|
|
What is the difference direct and indirect Coomb's test
|
Indirect test: patient serum
Direct test: Coombs' reagent mixed with RBCs; agglutination indicates presenc)e of IgG and cmplement on RBC membranes (e.g., warm and cold agglutinin disease) Indirect test: patient serum mixed with type 0 RBCs which, in turn, are mixed with Coombs' reagent; agglutination indicates presence of anti-RBC antibodies in serum (e.g., Rh alloimmunization) |
|
|
What is the most common type of anemia
|
iron deficiency anemia
|
|

what is this?
|

sideroblast:nucleated RBC with rings of iron granules ("ring" sideroblasts) - seen in sideroblastic anemia
|
|

what is this?
|

sideroblast:nucleated RBC with rings of iron granules ("ring" sideroblasts) - seen in sideroblastic anemia
|

