![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
digestion
|
mechanical breakdown of food into particles followed by chemical cleavage into small molecules that can be taken by the transport epithelium.
|
|
|
two major digestion questions
|
How do we digest different substances that we eat?\
How the entire process is regulated and coordinated? |
|
|
evolutionarily, developmentally and anatomically talk about the lumen of GI tract....
|
Evolutionarily, developmentally and anatomically, the lumen of GI is an external compartment (no strict homeostatic control)
|
|
|
relate a chemical plant to the GI system in 5 ways
|
lecture 38
1c |
|
|
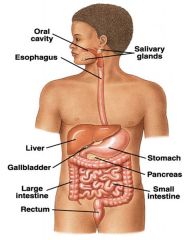
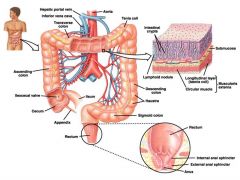
go over anatomy highlights of GI system
|
Pharynx, larynx, glottis (vocal folds) and epiglottis
Esophagus, upper* and lower esophageal sphincters Stomach: fundus, body, antrum, pyloric sphincter Small intestine: duodenum, jejunum, ileum, minor papilla, major papilla (openings that discharge bile and pancreatic juices into the duodenum) Ileocecal sphincter (valve) Large intestine (colon): ascending, transverse, descending, sigmoidal and rectum Internal and external* anal sphincters * the sphincters under voluntary control |
|
|
what kind of control are the internal and external anal sphincters under?
|
voluntary control
|
|
|
major papilla
|
openings that discharge bile and pancreatic juices into the duodenum)
|
|
|
oral cavity and esophagus major points
|
chewing, swallowing, salivary secretions contain amylase and lipase, no real absorption takes place
|
|
|
stomach major points
|
mixing and propulsion, acidic secretion containing pepsinogen and gastric lipase. Proteins and fats are partially digested. No active absorption except alcohol, and lipophilic drugs.
|
|
|
small intestine major points
|
Small intestine: mixing and propulsion, basic secretions from the pancreas containing proteases, amylases and lipases, bile and nucleases. Carbohydrates, fats, polypeptides and nucleic acids are digested.
Peptides, amino acids, sugars, vitamins and ions are absorbed by primary and secondary active transport. Fats are taken up by simple diffusion. |
|
|
how are fats taken up in the small intestine?
|
simple diffusion
|
|
|
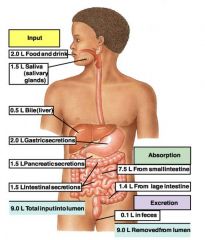
diagram of fluid input and fluid output in the digestive tract
|
|
|
|
picture of stomach
|
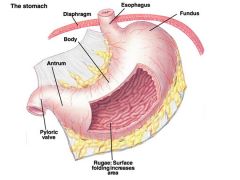
yellow stuff is mesentery
|
|
|
draw the stomach wall
|
also see lecture 38 3d
|
|
|
what is intestinal surface area enhanced by?
|
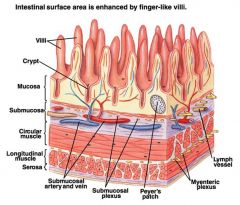
finger like villi
|
|
|
draw GI muscle membrane potential and how it relates to force of muscle contraction
|
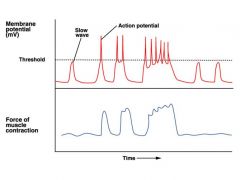
contraction depends on amplitude and frequency of action potentials
|
|
|
myenteric plexus
|
Peristalsis and ENS
Myenteric plexus = linear fibers that extend all the way through the GI tract. When stimulated: increase the tonic contraction on the wall increase the the intensity of rhythmic contractions increase the velocity of peristaltic waves releases VIP (inhibitory NT) which relaxes sphincters stimulation arrives from parasympathetic fibers sympathetic signals inhibit peristalsis |
|
|
Submucosal plexus
|
controls processes at the inner surface facing the lumen:
local secretion and absorption conduction of sensory signals from GI epithelium, where the afferent nerves terminate |
|
|
long reflexes
|
originate in the CNS, outside of the GI system. Also called cephalic reflexes. Anticipation of food, traveler’s constipation, psychologically induced diarrhea.
|
|
|
short reflexes
|
originate in the GI system via sensory endings in the submucosal plexus. Direct connection of submucosal neurons to myenteric motor neurons.
|
|
|
GI peptides
|
released by some cells in the GI tract act as hormones or paracrines.
|
|
|
draw the digestive CNS and ENS connection
|
ENS: enteric nervous system: the little brain
see scheme on lecture 38 on page 6a |
|
|
salivary glands
|
parotid
sublingual submaxillary: provide the majority of secretion |
|
|
Acinar Vs. Duct cells
p what does ps stim cause? saliva rich in what? |
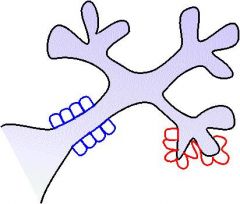
duct cells are blue
salivary gland Acinar cells: secrete fluid that is close to the plasma in its composition (Na+, K+, Cl-, HCO3-) Duct cells :modify the ionic contents by extracting Na+ and Cl- ..... As a result, saliva is rich with K+, HCO3- and hypotonic Contains: Salivary Amylase, Lingual Lipase, Lysozyme, Mucin Prasympathetic stimulation increases the release of watery saliva |
|
|
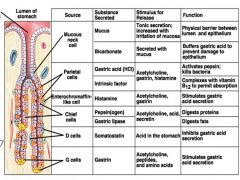
Cell types in the gastric mucosa
source substance secreted stimulus for release function |
|
|
|
2 safety measures and picture
|
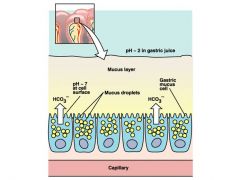
Safety measure #1
Most of the digestive enzymes are secreted in the form of inactive precursors and get activated only in the lumen by other secreted factors Safety measure #2 The intestinal wall is separated from the active digestive enzymes with the mucous layer |
|
|
picture of acid secretion by parietal cells
p |
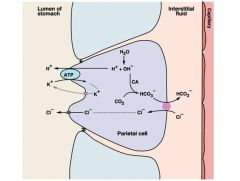
cl- channel is a CLC channel
|
|
|
Gastric acid
|
gastric secretion
(HCl) secreted by parietal cells the same cells secrete the Intrinsic Factor, a protein that binds Vitamin B12 and transports it across the epithelium |
|
|
Pepsin
|
gastric secretion
protease, most effective on collagen, released by chief sells as a precursor, Pepsinogen. Pepsinogen is converted into Pepsin in the presence of HCl |
|
|
Gastric Lipase
|
gastric secretion
Secreted by chief cells |
|
|
trypsinogen
|
pancreatic secretion (exocrine)
Trypsinogen, converted to Trypsin by Enteropeptidase secreted by intestinal wall 8.5-8.8 ph optimum |
|
|
chymotrypsinogen
|
pancreatic secretion (exocrine).....into small intestine
(converted to Chymotrypsin by Trypsin) 7.5-8.5ph optimum |
|
|
procolipase and prophospolipase
|
pancreatic secretion (exocrine) into small intestin
converted into colipase and phospolipase by trypsin....colipase displaces bile from surface of fat so that pancreatic lipase can break it down. |
|
|
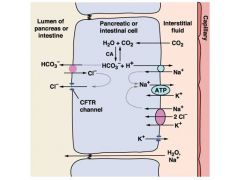
HCO3-
|
pancreatic exocrine secretion
neutralizes gastric acid |
|
|
water
|
pancreatic secretion (exocrine)
|
|
|
endocrine pancrease secretions
|
Endocrine pancreas (Islets of Langerhans) secretes:
Glucagon (a cells), Insulin (b cells), Somatostatin (D cells) |
|
|
summary of pancreatic secretion (exocrine)
|
Trypsinogen, converted to Trypsin by Enteropeptidase secreted by intestinal wall
Chymotrypsinogen (converted to Chymotrypsin by Trypsin) Procolipase and Prophospholipase are converted into Colipase and Phospholipase by Trypsin HCO3- - neutralizes gastric acid Water |
|
|
summary of gastric secretion
|
Gastric acid (HCl) secreted by parietal cells
the same cells secrete the Intrinsic Factor, a protein that binds Vitamin B12 and transports it across the epithelium Pepsin – protease, most effective on collagen, released by chief sells as a precursor, Pepsinogen. Pepsinogen is converted into Pepsin in the presence of HCl Gastric Lipase is also secreted by chief cells |
|
|
draw bicarbonate secretion in the pacrease
|
|
|
|
enterokinase
|
intestinal secretions:
also called entropeptidase, activates trypsin |
|
|
peptidases
|
intestinal secretions
Endopeptidase: break inner peptide bonds Exopeptidase: break outer end peptide bonds |
|
|
disacharidases
|
intestinal secretions:
Sucrase, Maltase, Lactase Sucrose = Glucose-Fructose, Maltose = Glucose-Glucose Lactose = Glucose-Galactose MN: SML is sweet |
|
|
intestinal secretions overview
|
disacharidases.....
intestinal secretions: Sucrase, Maltase, Lactase Sucrose = Glucose-Fructose, Maltose = Glucose-Glucose Lactose = Glucose-Galactose Enterokinase or enteropeptidase: activates Trypsin from trypsinogen Peptidases Endopeptidase Exopeptidases (Amino- and Carboxypeptidases) |
|
|
picture of large intestine
|
|
|
|
draw and talk about large intestine secretions
|
lecture 39 4a
|
|
|
pH ranges of following
pepsin trypsin chymotrypsin |
pepsin: 2-4
trypsin: 8.5-8.8 chymotrypsin: 7.5-8.5 |
|
|
types of fat
|
Phospholipids
Triglycerides Fatty acids Cholesterol Lipid-soluble vitamins |
|
|
talk about basics of bile salts
|
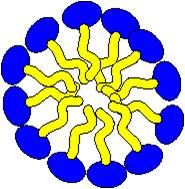
*picture shows a micelle that is a collection of bile
.....picture a bile yellow goo in the washing machine *bile is a natural detergent....has a polar head and a apolar tail *bile salts coat lipids to make emulsions (2 substances that can't be mixed, but are dispersed equally amongst one another) |
|
|
draw the bile pathway
|
|
|
|
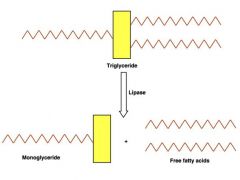
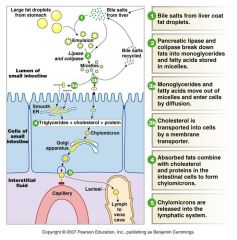
talk about summary of fat digestion
|
Bile stabilizes small fat droplets
Colipase displaces bile from the surface allowing the Pancreatic lipase to break down triglycerides into fatty acids and monoglycerides. These form small micelles and are partially water-soluble. They diffuse across the brushborder into the cytoplasm of epithelial cells. Cholesterol is actively transported. In the ER of enterocytes triglycerides are re-synthesized. Combined with cholesterol and proteins triglycerides form larger droplets called chylomicrons. Chylomicrons leave cells via exocytosis and enter the lymph. Bile is absorbed in ileum and recycled back into the liver. |
|
|
draw the hepatic portal system
|
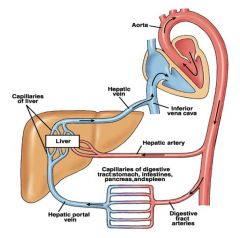
|
|
|
what do hepatocytes form?
|
hexagonal lobules
|
|
|
scheme with functions of liver
....liver functions |
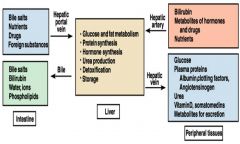
bilirubin is catabolic product of heme: a component of RBC
|
|
|
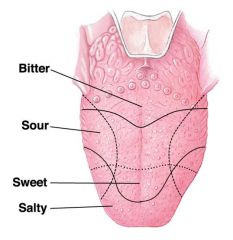
diagram with taste perception
|
|
|
|
5 types of taste
|
sweet
sour salty bitter umami |
|
|
draw the response that occurs in a taste bud cell and what receptors are responsible for what
|
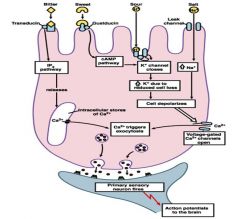
Bitter
(caffeine, strychnine) T2R GPCR Sweet GPCR T1R2+T1R3 Amino acids GPCR T1R1+T1R3 Umami (MSG) mGluR4 GPCR Salt ENaC Sour H+-gated K+ channels HCN Amino acid taste perception is greatly potentiated by purine nucleotides |
|
|
what is found in hot food
|
capsaicin
TRPV1 channel |
|
|
Phases of digestion
|
Cephalic phase: anticipation of a meal. Signals from medulla oblongata reach salivary glands and stomach ECL and G cells (through vagus). Secretions begin.
Mastication = chewing, mechanical preparation of the food in the mouth. Saliva dilutes the food. Amylase and Lipase begin their work. Lysozyme and antibodies guard from infections. The food mass turns into chyme. Deglutition = swallowing. Epiglottis directs the food into esophagus. Gastric phase: HCl kills microorganisms, denatures proteins; salivary amylase is inactivated by low pH; proteolysis by pepsin; about 10% of total fat is digested by gastric lipase. .....Regulation: parasympathetic stim. releases gastrin from G cells into the blood; gastrin promotes histamine and acid release; acid stimulates release of pepsinogen from chief cells; then acid triggers somatostatin release from D cells, which inhibits all gastric secretions Intestinal phase: chyme enters the small intestine; bile is added; HCO3- from pancreas neutralizes gastric acid; motility mixes chyme; proteins, sugars and lipids are digested; the products are absorbed by enterocytes and put into the portal vein; endocrine secretions from the intestine coordinate gastric emptying, HCO3- secretion and bile release from the galbladder. .....Regulation: hyperosmotic chyme blocks gastric motility; large amounts of carbohydrates block acid secretion via GIP; large amounts of fats release CCK, which also blocks acid secretion and motility, too much acid triggers release of secretin, which blocks gastric motility and secretion and stimulates release of HCO3- |
|
|
digestive hormones...name 5
|
Digestive hormones (16-39 amino acid peptides, all endocrine) Table 20-2
Gastrin (from G cells), stimulates secretion of gastric acid Cholecystokinin (CCK, from intestinal endocrine cells, neurons ) stimulates pancreatic secretion, bile release, inhibits gastric emptying Secretin (intestinal endocrine cells) stimulates pancreatic secretion, inhibits secretion of gastric aci d GIP (glucose-dependent insulinotropic peptide, from endocrine cells) releases insulin in a feed-forward fashion. Motilin (from endocrine cells) stimulates motility |
|
|
Talk about the following digestive disorders
1)swallowing 2)aerphagia 3)gastroesophagial reflux disease 4)peptic ulcers 5)gallstones 6)pancreatitis 7)malabsorption by small intestinal mucosa 8)intestinal colic 9)constipation 10)diarrhea 11)vomiting |
Swallowing disorders (muscular dystrophy, myasthenia gravis, botulism)
Aerphagia (causes belching and flatus) Gastroesophagial reflux disease (irritation of lower esophagus by gastric acid, causes ‘heart burns’) Peptic ulcers caused by imbalance of secretion of gastric juices and protective mucous coating a)Helicobacter pylori (disrupts the mucosa barrier) b)Aspirin (reduces protective prostaglandin production and mucosa secretion) c)excessive secretion of gastrin prolongs HCl secretion Gallstones (mostly cholesterol) may occlude the bile duct Pancreatitis = inflammation of pancreas predominantly due to gallstone occlusion of the ducts. Trypsinogen and chymotrypsinogen accumulate and may spontaneously convert into their active form causing self-digestion of the pancreas Malabsorption by the small intestinal mucosa = sprue, may result from poisoning by gluten or from some tropical infections) Intestinal colic (cramping pain in the event of mechanical obstruction) Constipation (atonic colon, usually due to inactivity of myenteric plexus) Diarrhea can result from infectious enteritis as well as may be phsychogenic from emotional stress Vomiting = reverse emptying of the upper GI tract. Chemoreceptots and nosiceptors in the stomach signal to vomiting center in the medulla oblongata. Antiperistalsis and distension of duodenum precedes vomiting. Strong downward contraction of the diaphragm and abdominal muscles. Esophageal sphincter relaxes at the same time. Vomiting is also triggered by neural stimuli integrated in the chemoreceptor trigger zone near the fourth ventricle of the brain. |
|
|
area of frequent ulceration
|
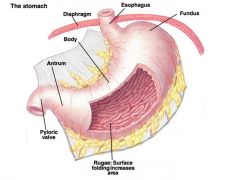
pyloric valve and area pointing to esophagus
|

