![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
describe the projection of the visual field onto the retina. (i.e. how is it orientated?)
|
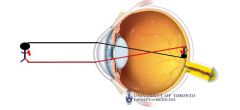
The visual field is projected onto the retina upside down and laterally inverted
|
|
|
The fovea is always on which side (nasal or temporal) of the optic nerve head?
|
The fovea is always temporal (lateral) to the optic nerve head
|
|
|
Why is the fovea ideally suited for focused vision?
1. (3) 2. 3. |
1. Anatomy
- avascular; has only photoreceptors and glial cells, axons of other ganglion cells divert around the fovea 2. Mostly cones (specialized for visual acuity and color vision) 3. 1:1 ratio of ganglion cells to cones |
|
|
What's the difference between rods & cons in terms of basal lighting, types of photopigment and vision produced?
|
Rods:
- dim light - express only rhodopsin - produce monochromatic vision Cones: - bright light - 3 types each sensitive to different areas of the visible spectrum - produce acute, color vision |
|
|
Why is the resolution power so much higher in the fovea?
|
The resolution power of the fovea is so high b/c there is a 1:1 photoreceptor to ganglion cell ratio. This makes for a very small receptive field. The ratio gets ++ larger as you move into the periphery = lower resolution.
|
|
|
What are Drusen? Where are they found and what are they a sign of?
|
Drusen are tiny yellow or white accumulations of extracellular material that build up in Bruch's membrane of the eye. They are a sign of Macular Degeneration
|
|
|
What type of pathology can the vitrous cause?
|
When the vitrous condenses it can tug on the retina and can create a tear. If this happens the vitrous can then get behind the retina and detatch it. This kills the photoreceptors b/c they need BOTH choroid & RPE circulation (they are in a watershed area between the two!)
|
|
|
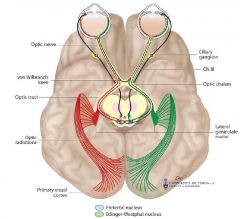
Signals from the retina are sent to what 3 areas of the brain?
|
1. Suprachiasmatic nucleus of the hypothalamus (for biological clock)
2. Lateral geniculate nucleus in the thalamus (relays information to the 1 visual cortex) 3. Pretectal region of the midbrain (anterior to sup colliculus) Pretectal & Edinger Westphal nucleus ** drives pupillary reflex** |
|
|
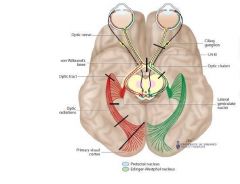
What is meyer's loop? The loop contains information from what visual field?
|
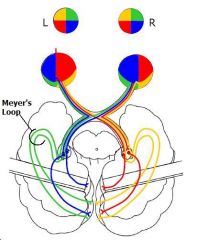
Meyer's loop = a system of fibers from the lateral geniculate body of the thalamus that loop anteriorly through the sublenticular part of the internal capsule en route to the 1 visual cortex. Carries info from top of visual field, to bottom of retina.
|
|
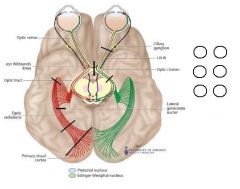
What would be the visual field defect for the first 3 lesions shown here?
|
|
|
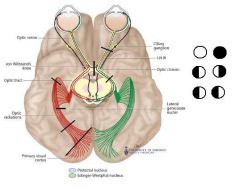
What would be the visual field defect for the following 4 lesions?
|
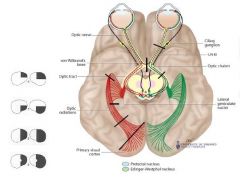
|
|
|
Where is the lesion if the visual field defect respects the:
- horizontal axis - vertical axis |
If the visual field defect respects the horizontal line, there is probably a retina/optic nerve lesion (in one or both eyes)
If the defect respects the vertical axis, there is probably a neurological lesion often in both eyes |
|
|
When and why would you get macular sparing?
|
When there is a lesion affecting the primary visual cortex you usually get macular sparing. This is b/c the macular fibers get dual blood supply from the PCA & MCA.
|
|
|
What are 4 causes of an optic chiasm lesion?
|
1. Pituitary adenoma
2. Suprasellar meningioma 3. Craniopharyngioma 4. Aneurysm of the internal carotid |
|
|
What is a junctional scotoma? What type of lesion would cause this and how?
|
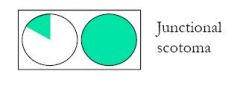
This is caused by an anterior chiasmal lesion that affects the fibers that are looping up at the chiasm. Nasal retinal fibers always decussate and may first loop into the contralateral optic nerve at the chiasm
|
|
|
Where is the primary visual cortex?
Where is the visual association area? |
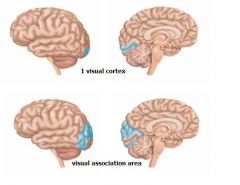
Primary: the area surrounding the calcarine fissure.
Association: Surrounds the primary visual area and occupies the occipital lobe. (the right hemisphere views the left visual field and vice-versa) ** the fovea is represented int he cortex surrounding the posterior 1/2 of the calcarine fissure |
|
|
How are signals transduced from photoreceptor to the ganglion cell? (i.e. what is each cell's response)
|
When light hits the p-receptor it closes it's channels and becomes herperpolarized, this decreases it's NT release are stimulates the bipolar cell to depolarize --> if enough graded responses this will trigger an AP in the ganglion cell.
|
|
|
What are the 4 steps in the visual transduction cascade, beginning with light striking rhodopsin?
|
1. After light hits it, rhodopsin splits and transducin is activated
2. Transducin activates phosphodiesterase 3. PDE destroys cGMP and this closes ion channels 4. Once channels close, cations can no longer enter and the cell becomes hyperpolarized 5 |
|
|
Which type of photoreceptor is specialized for night vision? In what general molecular way to rods and cones differ?
|
Rods came (genetically) from cones and are specialized for night vision. The components of both the activation and the shut-off pathways differ between rods and cones.
|
|
|
What is the only photosensitive molecule in the eye? What happens when it is struck by light?
|
Rhodopsin in the only photosensitive molecule in the eye. When light hits it, the helices will shift outwards allowing the G-protein to bind and be activated.
|
|
|
What are 4 functions of the RPE?
|
1. Phagocytoze disks
2. regenerate photopigments 3. metabolic support for the photoreceptors 4. absorb excess light |
|
|
Why do photoreceptors have 2 blood supplies? What are these?
|
The photoreceptors are supplied by the RPE and by retinal capillaries. They get dual blood supply because have the highest metabolic rate of any cell in the body.
|
|
|
How can the fovea survive even though it is avascular?
|
It has a lot less layers of cells!
|
|
|
What is the natural history of wet macular degeneration?
|
Macula will develop Drusen (yellow or white accumulations of extracellular material that build up in Bruch's membrane, below the RPE). This prompts the growth of abnormal blood vessels that grow through the membrane and can leak and bleed causing a lifting of the RPE = retinal death
|
|
|
What stimulates neovascularization in the retina and why is this a bad thing?
|
Diseases of retinal circulation cause occlusion and ischemia - hypoxic retina will release VEG-F which stimulates new vessels to grow. Problematic b/c these new vessels do not grow into the retina, they grow in to the vitreous and attach to the collagen scaffolding. This creates AP traction and can cause retinal detatchment (vessels have Felastic tissue that can tug on retina)
|
|
|
What are the 2 components of the blood retinal barrier?
What happens when retinal capillaries are occluded? |
The RPE and the retinal vessels that are covered by pericytes.
When retinal capillaries are occluded, ischemia results and this causes neovascularization and if untreated results in retinal detachment. |
|
|
What is a cataract?
|
Any clouding of the eye's crystalline lens. It is NOT cancer, caused by straining or a cause of irreversible blindness!
|
|
|
What are the symptoms of cataracts? (name 4 or 5)
|
1. Frequent script changes
2. Colors dulled or yellowish 3. Halos around lights at night 4. blurred vision 5. Glare |
|
|
What are the 6 causes/contributing factors to cataracts?
|
1. aging
2. family history 3. diabetes 4. Ocular trauma/surgery 5. steroids 6. UV light |
|
|
What is the one and only way to prevent cataracts?
What is the effect of a cataract on a person's vision? |
Protection from excessive sunlight! Antioxidants and vitamins are NOT protective!
Thickening of of the lens makes it stronger and more myopic -- person becomes near-sighted |
|
|
What is the ONLY proven treatment for cataracts!?!
When is a person eligible for this treatment? |
SURGERY!
Only do surgery when the pt feels the lack of vision is interfering with his/her quality of life or ability to perform ADLs |
|
|
What is the path of the pupillary light reflex from the retina to the iris spincter?
|
Retina (CN II)--> pretectal Ncl --> Both Edinger-Wetphal nuclei --> Ciliary ganglion ---> (CN3) iris spincter
|
|
|
In the swinging flashlight test, what are the direct and consensual responses? What would a + (abnormal) test look like?
|
The pupil constricts in the illuminated eye = direct response and also in the non-illuminated eye = consensual. Swinging the light back & forth should = bilateral pupillary constriction. If there is unilateral or assymetric damage in retina/CN2 then will get paradoxical dilation when light shone in affected eye.
|
|
|
What 2 retinal diseases and 4 optic nerve diseases could cause an afferent pupillary defect?
|
Retinal disease:
- occlusion of central retinal artery or vein - detatchement Optic nerve diseases: - Optic neuritis - Optic N tumor - Trauma - Glaucoma (Anterior ischemic optic neuropathy) |
|
|
What 5 conditions will NEVER cause a relevant afferent pupillary defect?
|
1. Cataracts
2. Papilledema 3. Refractive error / corneal scar 4. Cortical blindness d/t stroke 5. Functional visual loss (i.e. faking it) ** Bilateral or symmetrical CN2 damage or retinal disease will NOT cause a RAPD!! |
|
|
20/20 is the gold standard of vision. What is the limit for driving? Legal blindness? Below this you can test for what 4 things?
|
20/50 - driving vision
20/200 - legal blindness 10/200 - test person at 10ft Counting fingers Detecting motion Light perception or no light perception |
|
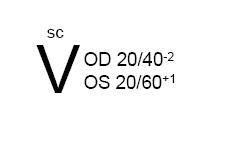
How would you interpret the following notation?
|
OD = right eye
OC = left eye SC = sine correction (uncorrected) (OU = both eyes) (CC = cum correctore, or with correction) |
|
|
Which 2 parts of the eye focus light? What type of light requires extra power to be focused on the retina?
|
Light is focused by the cornea (2/3) and lens (1/3).
Near light (divergent) are out of focus (presbyopia) and requires extra power to focus onto the retina (aka accomodation). Lens gets fatter! |
|
|
What (functionally) causes presbyopia? How is near & far vision affected? What is the treatment?
|
When lens provides insufficient accomodation for near things but distant vision is unaffected.
Tx: + readers (extra power) |
|
|
What (functionally) causes myopia? How is near and far vision affected? What is the treatment?
|
The eye is too long so distant light will be out of focus. (can also be that lens power is too high). Near-sight is unaffected but can't see distance ("nearsighted").
Tx: --ve lenses (divervent power) |
|
|
What (functionally) causes hyperopia? How is near and far vision affected? What is the treatment?
|
The eye is too short or the lens power is too low; have trouble seeing things in the distance. Young ppl's lenses can accomodate to supply the + but as they get older need glasses.
|
|
|
What (functionally) causes astigmatism? How is near and far vision affected? What is the treatment?
|
Astigmatism occurs when an image is focused to a line instead of a point. This is b/c the focusing system is ellipsoidal (like an egg).
Tx = glasses contacts laser etc |
|
|
What are 5 ways of checking the function of CN2? Which is the best and why?
|
1. Central visual acuity
2. RAPD * best b/c only objective measure 3. Color vision 4. Visual fields 5. Contrast sensitivity |
|
|
What (specifically) does papilledema mean?
What are the 4 signs of papilledema? |
Papilledema r= swelling of visible protion of CN2 secondary to increased ICP. ALL OTHER causes of swelling are NOT papilledema! Only say p-edema when you know swelling is due to increased ICP!
Signs: lost sharp borders, hyperemia/dilated veins, haemorrhages around nerve and no spontaneous venous pulsations (but there are only present in 80% of ppl - if you see them prob no inc ICP; if you can't see them not helpful!) |
|
|
What 4 things do you look for when examining of the eye?
|
1. Sharp borders
2. Pink nerve (yellow/pale = pathology) 3. Haemorrhages are always pathologic 4. Should see a "cup" (yellow hole in the middle |
|
|
What are the 2 main categories of imflammatory optic neuropathies?
|
Infectious: TB, syphilis, viral (HSV/HZV, etc), Fungi
Non-infectious: MS, sacroid, Wegner's |
|
|
What is the most common cause of optic nerve ischemia?
Symptoms? (most sensitive one?) Treatment? |
Giant cell Arteririts!
Occurs in pt's usually >70yrs Symptoms: Jaw claudications (painful chewing), headache, wt loss, fever, shoulder pain, fatigue. HIGHLY treatable! Give high dose steroid or else get bilateral visual loss!! |
|
|
What is are 2 toxic and 1 metabolic cause of optic N disease?
One or both eyes effected? |
Vitamin B12/folate deficiency, ethambutol or methanol toxicity,
Usually bilateral Slowly progressive Xtic visual field defect |

