![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
446 Cards in this Set
- Front
- Back
|
How does an upper motor neuron lesion affect bladder function?
|
Detrusor hyperreflexia, short contractions, external sphincter relaxation is slow. Leads to urge incontinence, slow flow.
|
|
|
How does a lower motor neuron lesion affect bladder function?
|
Acontractile bladder, poor bladder sensation.
|
|
|
What week does gastrulation occur?
|
Week 3
|
|
|
What week does neurulation occur?
|
Week 3 and 4
|
|
|
Name the derivatives of the embryonic structure, hypoblast.
|
• Endoderm of yolk sac
• Extra-embryonic mesoderm |
|
|
What event completes the end of neurulation?
|
When closure of the anterior pore occurs. This happens at the end of week 4.
|
|
|
First arch syndrome
|
• Insufficient NCC migration into 1st arch.
• Congenital abnormalities of eyes, ears, mandible, palate. |
|
|
Facial stigmata of fetal alcohol spectrum disorder
|
Short palpebral fissures.
Poorly formed philtrum. Thin upper lip. |
|
|
When do the neuropores close?
|
• Anterior neuropore: 23 days
• Posterior neuropore: 25 days (2 days after anterior neuropore closes) |
|
|
At week 6, what are the zones that the spinal cord is divided into?
|
• Alar plate
- Dorsal horn - sensory • Basal plate - Ventral horn - motor • Marginal zone - Presumptive white matter |
|
|
Where are temporal and spatial summation most important for generating an action potential?
|
On the post-synaptic membrane of an alpha-motor neurons dendrite.
|
|
|
The perineurium is continuous with which layer of the meninges?
|
Arachnoid
|
|
|
How to determine the prognosis of a complete cord injury?
|
It is poor prognosis, unless some recovery is seen within 24 hours.
|
|
|
What is hematomyelia?
|
Hemorrhage into the gray matter, with disruption of axons in white matter.
|
|
|
What are causes of Brown Séquard Syndrome?
|
• Penetrating cord injuries
• Stab • Gun shot wound (GSW) • Extrinsic cord lesions • Tumor • Disc • Intrinsic cord lesions • Tumor (e.g. schwannoma) • Blunt spinal cord trauma |
|
|
Which tract of the spinal cord do descending inhibitory neurons run?
|
Lateral corticospinal tract.
If you damage this tract, then the patient will experience UMN symptoms, such as weakness, spasticity, increased reflexes, Babinski reflex, clonus. |
|
|
What are causes of complete cord injury?
|
Trauma.
Cord compression by tumor. Abscess. |
|
|
What are causes of central cord syndrome?
|
Trauma (especially with underlying narrow spinal canal).
Intramedullary tumor. Syringomyelia. |
|
|
What are causes of anterior spinal artery infarct?
|
Thrombosis.
Embolism (air in the bends). Surgery on descending aorta. |
|
|
What are causes of subacute combined degeneration?
|
B12 deficiency.
|
|
|
What are causes of acute cauda equina syndrome?
|
Lumbar spine fracture or subluxation.
Epidural metastatic tumor. Hematoma. Abscess. |
|
|
Where do descending pain modulatory pathways originate from?
|
Periaqueductal gray in the brainstem.
|
|
|
Areas of synapses and crossovers of the spinothalamic tract.
|
Dorsal horn on ipsilateral side. Secondary neuron crosses over to contralateral side via anterior white commissure.
VPL of thalamus, contralateral side. |
|
|
Areas of synapses and crossovers of posterior column-medial lemniscus tract.
|
Nucleus gracilis/cuneatus in caudal medulla on ipsilateral side.
Secondary neuron crosses over as internal arcuate fibre in the caudal medulla. VPL of thalamus, contralateral side. |
|
|
Areas of synapses in the dorsal spinocerebellar tract.
|
Travel up fasciculus gracilis to L3, where it primary neuron synapses with Clarke's nucleus.
Secondary neuron synapses with cerebellum on ipsilateral side. |
|
|
Areas of synapses in the cuneocerebellar tract.
|
Travel up fasciculus cuneatus.
Synapse in accessory cuneate nucleus in rostral medulla. Secondary neuron synapses with cerebellum on ipsilateral side. |
|
|
Which tracts need to remain open for orgasm to occur?
|
Lateral corticospinal tract
Spinothalamic tract |
|
|
Traveling rostrally in the spinal cord, at what level does the fasciculus cuneatus appear?
|
T6 and up.
|
|
|
Name opioid receptor antagonists.
|
Naltrexone.
Naloxone. |
|
|
What is the denticulate ligament and filum terminale made of?
|
Pia and glial cells.
|
|
|
Complications of bacterial meningitis
|
• Cerebral edema
• Hydrocephalus • Abscess formation • Infarcts |
|
|
Which nerve root would tend to be affected with a paracentral or subarticular herniation at L4-L5?
|
The traversing L5 root.
|
|
|
Which nerve root would tend to be affected with a foraminal herniation at L4-5?
|
L4 nerve root, as it enters the foramen, just under the pedicle.
|
|
|
The middle meningeal artery is a branch of...
It passes through the ... to reach the inside of the skull. |
The maxillary artery, which is a branch of the external carotid artery.
Passes through the foramen spinosum. |
|
|
The middle cerebral artery is a branch of ...
|
The internal carotid artery.
|
|
|
How much CSF is produced per day, on average?
What is the total normal volume of CSF in an adult at any time? |
500 cc is produced per day.
150 cc is the normal amount that is circulating at any time. |
|
|
Where does the CSF exit from the ventricles?
|
In the fourth ventricle, via the 2 lateral foramen of Luschka, and midline foramen of Magendie.
|
|
|
What are the spaces formed by the meninges and skull called?
|
1. Epidural space (between skull and dura)
2. Subdural space (between dura and arachnoid) 3. Subarachnoid space (between arachnoid and pia) The epidural and subdural spaces are potential spaces. I.e. they don't exist unless there is a pathology, such as a hemorrhage. |
|
|
What is the location of the third ventricle?
|
Within the thalamus and hypothalamus.
|
|
|
What is the location of the fourth ventricle?
|
Within the pons, medulla, and cerebellum.
|
|
|
What space are the cranial venous sinuses in?
|
They are between the endosteal layer of dura, and the meningeal layer of dura.
|
|
|
The cranial venous sinuses all eventually drain into the ... vein.
|
Internal jugular vein, via the sigmoid sinuses.
|
|
|
Post-ganglionic sympathetic nerves are derived from...
|
Neural crest
|
|
|
Basal ganglia nuclei
|
• Caudate
• Putamen • Globus pallidus |
|
|
Purpose of inferior and superior colliculi
|
• Inferior colliculus (paired colliculi)
• Auditory center • Inferior brachium - fibres from each inferior colliculus to thalamus (medial geniculate body or nucleus) • Superior colliculus • Center for visual reflexes • Superior brachium - fibres from visual pathways and visual area of cortex to each superior colliculus. |
|
|
What spinal level does the conus medullaris usually end at?
|
L1 or L2 vertebral body
|
|
|
Other names for "tract"
|
Fasciculus, funiculus, column, lemniscus, peduncle, brachium, stria
|
|
|
What level of the brain/spinal cord do you find the nucleus cuneatus and gracilis?
|
Caudal medulla.
|
|
|
What level of the brain/spinal cord do you find the periaqueductal gray?
|
Midbrain.
|
|
|
What level of the brain/spinal cord do you find the red nucleus?
|
Midbrain.
|
|
|
What is the exit foramen for CN III?
|
Superior orbital fissure
|
|
|
What is the exit foramen for CN IV?
|
Superior orbital fissure
|
|
|
What is the exit foramen for CN V1 (ophthalmic)?
|
Superior orbital fissure
|
|
|
What is the exit foramen for CN V2 (maxillary)?
|
Foramen rotundum
|
|
|
What is the exit foramen for CN V3 (mandibular)?
|
Foramen ovale
|
|
|
What is the exit foramen for CN VI?
|
Superior orbital fissure
|
|
|
What is the exit foramen for CN VII
|
Internal auditory meatus
|
|
|
What is the exit foramen for CN VIII
|
Internal auditory meatus
|
|
|
What is the exit foramen for CN XI
|
Jugular foramen
|
|
|
What is the exit foramen for CN XII
|
Hypoglossal canal
|
|
|
What is the exit foramen for CN IX?
|
Jugular foramen
|
|
|
What is the exit foramen for CN X?
|
Jugular foramen
|
|
|
Derivatives of the 1st pharyngeal arch cartilage.
|
- 2 of the middle ear ossicle
- Mandible primordium |
|
|
Derivatives of the 2nd pharyngeal arch cartilage.
|
- One of the middle ear ossicles
- Part of hyoid bone |
|
|
Derivatives of the 3rd pharyngeal arch cartilage.
|
- Part of hyoid bone
|
|
|
Derivatives of the 4th and 6th pharyngeal arch cartilage.
|
- Fuse to form the thyroid and cricoid cartilages
|
|
|
What is the embryonic derivative of epiglottis?
|
Mesenchyme of the 3rd and 4th pharyngeal arches
|
|
|
Muscle derivatives and innervation of the pharyngeal 1st arch muscles.
|
• Muscles of mastication
□ Temporalis □ Masseter □ Medial and lateral pterygoid • Mylohyoid • Anterior belly of digastric • Tensor veli palatini Nerve: V3 |
|
|
Muscle derivatives and innervation of the pharyngeal 2nd arch muscles.
|
• Muscles of facial expression
• Posterior belly of digastric • Stylohyoid • Stapedius • Platysma • Nerve: CN VII, facial nerve. |
|
|
Muscle derivatives and innervation of the pharyngeal 3rd arch muscles.
|
• Stylopharygeus
• Nerve: CN IX, glossopharyngeal |
|
|
Muscle derivatives and innervation of the pharyngeal 4th arch muscles.
|
• Cricothyroid
• Nerve: CN X, superior laryngeal branch of vagus nerve |
|
|
Muscle derivatives and innervation of the pharyngeal 6th arch muscles.
|
• Other intrinsic laryngeal muscles
• Nerve CN X, recurrent laryngeal branch of vagus nerve |
|
|
Muscle derivatives and innervation of the caudal pharyngeal arch muscles.
|
• Remaining palatine muscles and constrictors
• Precise sources uncertain • Nerve: cranial accessory via branches of vagus nerve |
|
|
Muscle derivatives and innervation of the occipital somites.
|
• Extrinsic and intrinsic tongue muscles (except palatoglossus)
• Nerve: CN XII, hypoglossal |
|
|
Derivatives of the 1st pharyngeal pouch.
|
• Tympanic membrane
• Tympanic cavity • Auditory tube |
|
|
Derivatives of the 2nd pharyngeal pouch.
|
• Endodermal lining of 2nd pouch forms surface epithelium and lining of palatine tonsil crypt
• Mesenchyme around crypt differentiates into lymphoid nodules |
|
|
Derivatives of the 3rd pharyngeal pouch.
|
• Inferior parathyroid glands
• Thymus |
|
|
Derivatives of the 4th pharyngeal pouch.
|
• Superior parathyroid glands
• Ultimopharyngeal body (gives rise to parafollicular cells) - these cells originate from NCC that migrate from pharyngeal arches into 4th pair of pharyngeal pouches |
|
|
What nerves and arteries traverse the cavernous sinus?
|
Laterally: III, IV, V1, V2
Mediall: VI, internal carotid artery |
|
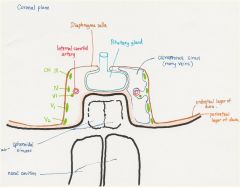
What section is this?
Where are the following tracts: -posterior column-medial lemniscus -spinothalamic tract -corticospinal tract -medial longitudinal fasciculus |

Caudal medulla
|
|
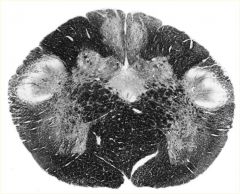
What section is this?
Where are the following tracts: -posterior column-medial lemniscus -spinothalamic tract -corticospinal tract -medial longitudinal fasciculus |

Midbrain
|
|

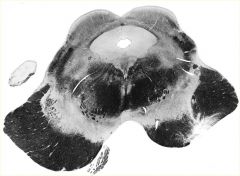
What section is this?
Where are the following tracts: -posterior column-medial lemniscus -spinothalamic tract -corticospinal tract -medial longitudinal fasciculus |

Pons
|
|
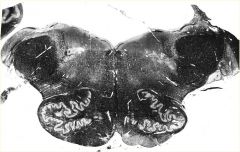
What section is this?
Where are the following tracts: -posterior column-medial lemniscus -spinothalamic tract -corticospinal tract -medial longitudinal fasciculus |
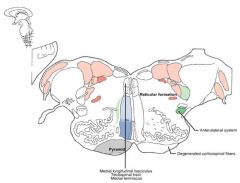
Rostral medulla
|
|
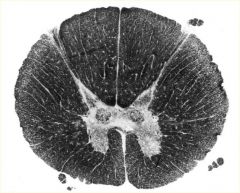
What section is this?
Where are the following tracts: -posterior column-medial lemniscus -spinothalamic tract -corticospinal tract -medial longitudinal fasciculus |
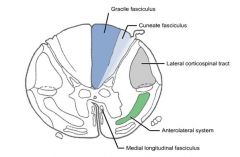
Spine (T4)
|
|
|
What are the semicircular organs of the inner ear responsible for detecting?
|
Angular acceleration (aka head rotation)
|
|
|
What are the otoliths (utricle and saccule) of the inner ear responsible for detecting?
|
Sense body orientation and linear motion.
Utricle detects horizontal plane. Saccule detects vertical plane. |
|
|
The labyrinth fluids in the inner ear are called perilymph and endolymph. Which one has similar composition to ECF, and which one has similar composition to ICF?
|
Perilymph is similar to ECF
• Low [K+] = 10 mM • High [Na+] = 140 mM Endolymph is similar to ICF • High [K+] = 144 mM • Low [Na+] = 5 mM |
|
|
What are the names of the hair cell cilia on the vestibular sensory epithelium?
|
Stereocilia
60-100 / hair cell Kinocilium 1 / hair cell |
|
|
What neurotransmitter do vestibular hair cells release?
|
Glutamate. This excites afferents of CN VIII (vestibulocochlear)
|
|
|
How does excitation/inhibition of a vestibular hair cell work?
|
Excitation/depolarization
• Deflection towards kinocilium ◊ Opens stretch sensitive K+ channels on cilia ◊ Depolarization opens Ca2+ channels at base ◊ Increased NT (glutamate) release ◊ Increased firing of vestibular afferents to CNS Inhibition/Hyperpolarization • Deflection aware from kinocilium ◊ Close K+ channels on cilia ◊ Hyperpolarization = inhibition of hair cells ◊ Decreased NT release ◊ Decreased afferent firing to CNS |
|
|
In the ampulla of the semicircular organs of the inner ear, what is the sensory vestibular epithelium called?
And the acellular gel-like substance? |
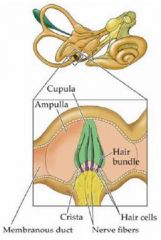
Crista
Cupula |
|
|
What is otoconia?
|
Calcium carbonate crystals that sit on top of the otolithic membrane.
The pressure of otoconia deflects hair cell cilium. |
|
|
At what levels do you find the vestibular nuclei?
What do each of the four vestibular nuclei do? |
Pons and rostral medulla.
• Lateral vestibular nucleus (Deiter's nucleus) • Innervates gravity-opposing muscles of limbs to maintain posture • Medial vestibular nucleus • Reflex adjustments of neck and trunk muscles to restore head position after disturbance • Superior and medial vestibular nuclei • Eye movements • Vestibulo-ocular reflex (VOR) • Inferior vestibular nucleus • Integrates multi-sensory input, and cerebellum to regulate VOR gain |
|
|
In caloric testing of induced nystagmus, which direction does the fast saccadic phase move if you introduce cold water? warm water?
|
COWS
Cold water - opposite side. Warm water - same side. |
|
|
What is the cause of benign paroxysmal positional vertigo?
Is it bilateral, or unilateral? |
Displaced otoconia lodged in semicircular canals.
Unilateral |
|
|
What is the cause of Meniere's disease?
Is it bilateral, or unilateral? |
Increased endolymph in inner ear.
Origins not well understood. Unilateral or bilateral. Diagnostic criteria: - 2 spontaneous episodes of rotational vertigo lasting at least 20 minutes - Sensorineural hearing loss - Tinnitus |
|
|
What is the cause of vestibular neuritis?
Is it bilateral, or unilateral? |
Viral infection of vestibulo-cochlear nerve.
Usually unilateral. |
|
|
What is the cause of perilymph fistula?
|
Breach in the oval and/or round window of the cochlea.
|
|
|
What are some drugs that cause ototoxicity?
|
Aminoglycosides, such as gentamicin and streptomicin.
|
|
|
What causes mal de debarquement?
|
Failure of CNS plasticity to respond to prolonged movement. Normal people adjust quickly when the movement stops. In some people, they have lost the ability to adjust.
E.g. getting off boat after a long ride. They feel like stuff is still moving. |
|
|
Which of the vestibulospinal tracts are ipsilateral, and which ones are not?
|
Lateral VS tract - ipsilateral
Medial VS tract - bilateral, more dense on ipsilateral side Superior/medial (VOR) - bilateral contralateral Inferior VS tract - ipsilateral |
|
|
Which nuclei does corticobulbar tract terminate on?
How do the cortical fibers travel - ipsilateral, bilateral, contralateral? |
a. Nucleus ambiguus IX, X, XI [cranial root]
- Receives bilateral innervation b. Motor nucleus of V - Receives bilateral innervation c. Spinal accessory nucleus XI - Receives ipsilateral projections for sternomastoid - Mostly contralateral projections for trapezius d. Hypoglossal nucleus XII - Receives bilateral projections, but crossed to genioglossus. e. Facial motor nucleus VII - Bilateral innervation to rostral part of nucleus (upper facial muscles) - Contralateral innervation to caudal part of nucleus (lower facial muscles) |
|
|
What can you say about spatial and temporal resolution for magnocellular and parvocellular retinal ganglion cells?
|
Magnocellular
- Low spatial, high temporal resolution Parvocellular - High spatial, low temporal resolution |
|
|
Why is the optic nerve considered a part of the CNS, and not a peripheral nerve?
|
It is myelinated by oligodendrocytes.
|
|
|
Which hemifields does the right optic tract represent?
|
It contains information from the left hemifield of each eye.
|
|
|
What is the three neuron relay for vision?
|
1. Bipolar cells
2. Retinal ganglion cells - projects through optic nerves, chiasm, tracts. Terminates on lateral geniculate nucleus of posterior thalamus. 3. LGN of posterior thalamus projects via optic radiations to striate nucleus. |
|
|
What are the divisions of the extra-striate cortex?
|
a. Dorsal (occipito-parietal)
- The "where" stream - Concerned with motion processing, depth perception, visuospatial data for attention, eye and hand movements b. Ventral (occipito-temporal) - The "what" stream - Concerned with colour processing, object recognition (e.g. words and faces) |
|
|
Does shining light on a photoreceptor decrease or increase the amount of NT released?
|
It hyperpolarizes the photoreceptor, and therefore decreases the amount of NT released.
|
|
|
In lesions to the cavernous sinus, the first cranial nerve to be affected is...
|
CN VI
|
|
|
Does a positive Romberg sign indicate problem with the dorsal column or the cerebellum?
|
Dorsal column.
A person with a cerebellar lesion will show sway regardless of whether the eyes are open or closed. |
|
|
Which cortex controls saccadic eye movements, and which controls pursuit?
|
Parieto-occipital cortex (visual association cortex) controls pursuit movements.
Frontal cortex (frontal eye field) controls saccadic movements to the opposite side of the body. |
|
|
What does a lesion in the motor association area cause?
|
Apraxia
|
|
|
What does a lesion in the sensory association area cause, if in the dominant hemisphere?
What about in the non-dominant hemisphere? |
If lesion in the dominant hemisphere -> tactile agnosia, astereognosis
If lesion in the non-dominant hemisphere -> hemispatial neglect |
|
|
What does a lesion in the primary visual area on the right hemisphere cause?
|
Homonymous hemianopsia on the left field of vision.
|
|
|
What does a lesion in the right frontal eye field cause?
|
Deficit in gaze to the left.
Eyes will deviate to the right (the side of the lesion), due to unopposed action of the extraocular muscles. |
|
|
What does a lesion in the primary auditory area cause?
|
Subtle decrease in hearing. Subtle because each ear is represented bilaterally.
|
|
|
What does a lesion in the auditory association area cause?
|
Word deafness - hearing is fine, but can't understand the words.
|
|
|
What does a lesion of the arcuate fasciculus cause?
|
The arcuate fascilculus connects Broca's and Wernicke's areas.
The lesion will cause conduction aphasia, where paraphasic errors are common (semantic, neologisms, literal). |
|
|
What does a lesion in the language areas of the non-dominant hemisphere cause?
|
Aprosodia
- disturbance in rhythm, intonation and melody of language. |
|
|
What are the most common causes of intraparenchymal hemorrhages?
|
1. Hypertension
2. Amyloid angiopathy (common in Down's syndrome) |
|
|
What are common areas in the cranial vasculature that are most susceptible to aneurysms?
|
Anterior communicating artery - 30%
Posterior communicating artery - 25% Middle cerebral artery - 20% Carotid bifurcation - 8% Basilar bifurcation - 7% |
|
|
Why are cerebral arteries more susceptible to aneurysms than peripheral arteries?
|
Thinner intima/media
Lacks external elastica Medial defects |
|
|
Symptoms of subarachnoid hemorrhage.
|
• Sudden, severe headache - worst h/a in life
• Nausea • Photophobia • Loss or altered level of consciousness • Focal neurological deficits • Sudden death |
|
|
What cerebrovascular diseases are indicated by focal localizing neurological signs? Absence of focal localizing neurological signs?
|
Intraparenchymal hemorrhage.
Absence of focal localizing neurological signs indicates subarachnoid or intraventricular hemorrhage. |
|
|
How are subarachnoid hemorrhages graded?
|
Hunt and Hess Scale
• Grade 1: asymptomatic or mild h/a • Grade 2: severe h/a, meningismus (triad of nuchal rigidity, photophobia, and headache) • Grade 3: drowsy, confused, mild deficit • Grade 4: stuporous, severe deficits • Grade 5: deep coma, moribund (near death) |
|
|
How do you tell a lumbar puncture actually has RBCs in the CSF, rather than just from a traumatic tap?
|
> 100,000 RBCs in the CSF (by sheer number)
Presence of xanthochromia also supports an SAH, rather than a traumatic tap. |
|
|
What is amaurosis fugax?
|
"Fleeting darkness"
Transient monocular vision loss. Due to temporary reduction in retinal artery, ophthalmic artery or ciliary artery blood flow. Usually caused by emboli from atherosclerotic carotid artery. |
|
|
Where is the primary auditory area?
|
Superior surface of superior temporal gyrus (also called Heschl's gyrus)
|
|
|
Where is the auditory association area?
|
Superior temporal gyrus, area posterior to primary auditory gyrus in lateral sulcus.
|
|
|
Where is the secondary taste area?
|
Orbital cortex of frontal lobe and amygdala.
|
|
|
Name all of the long association fibres
|
Superior longitudinal fascilculus
- aka arcuate fasciculus - connects frontal, parietal and temporal lobes Inferior occipitofrontal fasciculus - connects frontal, temporal, and occipital lobes Superior occipitofrontal fasciculus - connects frontal, parietal, and occipital lobes Cingulum - connects areas of limbic cortex with each other. |
|
|
What does the anterior commissure connect?
|
Two anterior temporal lobes, and olfactory bulbs.
|
|
|
What does the posterior commissure connect?
|
The two pretectal nuclei
|
|
|
What fibers are contained in the anterior limb of the internal capsule?
|
Corticopontine fibers
Thalamocortical fibers from DM, anterior nucleus |
|
|
What fibers are contained in the posterior limb of the internal capsule?
|
Corticopontine, and other corticofugal fibers
Thalamocortical fibers from VP, VL, VA Corticospinal fibers |
|
|
What fibers are contained in the genu of the internal capsule?
|
Corticobulbar fibers
|
|
|
What function does the medial geniculate nucleus of the thalamus play?
|
Relays hearing information
|
|
|
What function does the lateral geniculate nucleus of the thalamus play?
|
Relays visual information
|
|
|
Which thalamic nuclei relay motor information?
|
Ventral lateral
Ventral anterior |
|
|
What does the pulvinar nuclei of the thalamus connect to?
|
Sensory association areas.
|
|
|
What does the dorsomedial nuclei of the thalamus connect to?
|
Frontal association cortex.
|
|
|
What are the intralaminar nuclei?
What do they project to? |
Centromedian and parafascicular nuclei.
Receives input from ascending reticular activating system (ARAS), and has diffuse projections to the cortex. |
|
|
What are the key anatomical structures for episodic memory?
|
◊ Medial temporal lobes
► Hippocampus ► Parahippocampus ◊ Anterior thalamic nucleus ◊ Mamillary body ◊ Fornix ◊ Prefrontal cortex |
|
|
What are the key anatomical structures for procedural memory?
|
◊ Basal ganglia
◊ Cerebellum ◊ Supplementary motor areas |
|
|
What are the key anatomical structures for semantic memory?
|
Inferolateral temporal lobes
|
|
|
What are the key anatomical structures for working memory?
|
◊ Phonological: prefrontal cortex, Broca's area, Wernicke's area
◊ Spatial: prefrontal cortex, visual association areas |
|
|
What kind of problem causes paraphasia?
|
Wernicke's aphasia
Transcortical aphasia |
|
|
Are the following affected with Wernicke's aphasia?
- speech - auditory comprehension - repetition - reading - writing - vision |
- speech - fluent, but paraphasic
- auditory comprehension - impaired - repetition - impaired - reading - impaired - writing - well formed, with paragraphic errors. - vision - right upper quadrantanopsia |
|
|
What are the three types of apraxia?
|
Limb kinetic
□ Loss of fine motor control or dexterity Ideomotor apraxia □ Failure to perform skilled/learned motor sequences on command, or to imitation. Ideational apraxia □ Difficulty in performing a sequence of steps to complete a task □ Loss of knowledge to select tools/objects |
|
|
Where are the formulae for complex movements (praxicons) stored?
|
Wernicke's area.
|
|
|
What is aphemia?
|
Also known as pure word mutism.
Looks like Broca's aphasia, except there is more dysarthria, and writing is preserved. |
|
|
Name the two types of visual agnosia, and their localization.
|
Apperceptive
- Seen most often after anoxic damage - Location □ Occipitotemporal > inferior parietal lesions Associative - Location □ Bilateral occipito-temporal damage. □ Left peri-striate involvement common. |
|
|
Localization of prosopagnosia
|
Right or bilateral medial occipitotemporal cortex
- lingual, fusiform and parahippocampal cortex Caused by right PCA territory infarct |
|
|
In the mental status exam, what functions are you testing for non-language, dominant parietal lobe function?
Is there a name for the constellation of symptoms that a lesion in this lobe would cause? |
Gerstmann syndrome
Location: dominant lobe, angular gyrus Acalculia Right/left confusion Finger agnosia Agraphia |
|
|
Localization of alexia without agraphia.
|
Dominant PCA territory infarct
- infarction of left visual cortex, and splenium of corpus callosum Patient will also have right hemianopia. Information about left hemifield will reach right occipital cortex, but can't cross to language hemisphere because of involvement of corpus callosum. |
|
|
What is the Meyer Overton rule?
|
An inhaled anesthetic's MAC (minimal alveolar concentration) inversely correlates with its lipid solubility.
E.g. N2O has a high MAC of 105%, which means that it is not very soluble in lipid |
|
|
What are the physiological end points of general anesthesia?
|
Hypnosis (loss of consciousness)
Analgesia Amnesia Immobility Inhibition of autonomic and sensory reflexes Muscle relaxation |
|
|
What are the determinants of the rate of uptake of an inhaled anesthetic?
|
1. Its solubility in the blood
2. Partial pressure difference between alveoli and pulmonary venous blood 3. Alveolar ventilation |
|
|
MOA and adverse effects of phenytoin
|
Block voltage-dependent Na+ channels at high firing frequencies
Adverse effects: hirsuitism, gingival hypertrophy, and teratogenic |
|
|
MOA and major side effects of carbamazepine
|
Block voltage-dependent Na+ channels at high firing frequencies
Side effects: aplastic anemia, SJS, hepatitis, SIADH |
|
|
MOA of barbiturates
|
Prolong GABA-mediated Cl- channel openings
Some blockade of voltage-dependent Na+ channels |
|
|
MOA of benzodiazepines
|
Increase frequency of GABA-mediated Cl- channel openings
|
|
|
MOA and adverse effects of valproic acid.
|
May enhance GABA transmission in specific circuits
Blocks voltage-dependent Na+ channels Adverse effects □ Not used in women of child-bearing age, because it is teratogenic -risk of spina bifida. □ Hair loss □ Weight gain |
|
|
What is the cause of these pupil signs?
- Small to midrange, equal, reactive - Pinpoint pupils - Unilateral dilated pupil - Bilateral dilated non-reactive pupils - Bilateral midrange non-reactive pupils - Bilateral dilated reactive |
Small to midrange, equal, reactive
- Most likely toxic/metabolic cause Pinpoint pupils - Either pontine infarct, or opiate overdose Unilateral dilated pupil - Supratentorial mass lesion until excluded Bilateral dilated non-reactive pupils - Bilateral structural midbrain, or severe metabolic Bilateral midrange non-reactive pupils - Severe metabolic, or perhaps barbiturate overdose Bilateral dilated reactive - Mild/moderate toxic/metabolic or structural |
|
|
Interpret these oculovestibular reflex findings, after injecting cold water into one ear:
• If fast movement is to opposite side in both eyes • If both eyes have slow deviation to cold water, but there is no nystagmus • If only ipsilateral eye deviates to cold water • No eye movement |
• If fast movement is to opposite side in both eyes
§ Patient not comatose. § Brainstem and cerebral cortex are intact. • If both eyes have slow deviation to cold water, but there is no nystagmus § Brainstem and MLF are intact • If only ipsilateral eye deviates to cold water § Lesion in MLF • No eye movement § Brainstem dysfunction § Structural or toxic/metabolic |
|
|
Interpret the following oculocephalic reflex findings:
• Eyes continue to look up to ceiling, and gradually return to original mid-gaze position. • Eyes turn with the head (remain midgaze) |
• Eyes should continue to look up to ceiling, and gradually return to original mid-gaze position.
- This is intact Doll's eyes response - Intact brainstem • If eyes turn with the head, this is absent doll's eyes response - Indicates either a dysfunctioning brainstem, or a pseudocoma |
|
|
How is pain further classified under "adaptive" and "maladaptive"?
|
Adaptive - in response to noxcious stimulus
i. nociceptive ii. inflammatory Maladaptive - uncoupled from noxious stimulus or healing tissue i. Neuropathic ii. Functional (abnormal operation of nervous system. e.g. fibromyalgia) |
|
|
What is the mechanisms involved in:
- peripheral sensitization to pain? - central sensitization to pain? |
Peripheral sensitization
i. Post-translational processing ii. Altered transcription/translation Central sensitization i. Acute phase - Post-translational processing - removal of Mg2+ block of NMDA receptors ii. Persistent phase - Altered transcription/translation - Disinhibition - Structural reorganization (sprouting of Aβ fibers) |
|
|
What is the pain "gate theory"?
|
It states that the transmission of pain from the peripheral nerve through the spinal cord can be modulated by:
1. Other afferent neurons 2. Controls emanating from the brain |
|
|
What is neuropathic pain?
|
Pain initiated or caused by a primary lesion or dysfunction in the nervous system.
|
|
|
What is causalgia?
|
Syndrome of sustained burning pain, allodynia, and hyperpathia after traumatic nerve lesion.
Often combined with vasomotor and sudomotor dysfunction, and later trophic changes. |
|
|
What are the first and second-line agents for chronic neuropathic pain?
|
First-line:
- TCAs - Anticonvulsants (gabapentin, pregabalin, carbamazepine) Second-line - SSNRI (venlafaxine) - Topical lidocaine |
|
|
Name the secondary amine TCAs and the tertiary amine TCAs.
What are the main differences between secondary and tertiary TCAs? |
Secondary amines
• Nortriptyline • Desipramine Tertiary amines • Amitriptyline • Imipramine Secondary amines are better tolerated, so use secondary amines on elderly patients. Secondary amines preferentially inhibit reuptake of NE, whereas tertiary amines preferentially inhibit reuptake of 5HT |
|
|
What are the most significant side effects of TCAs?
|
Anticholinergic effect
α-adrenergic blockade - postural hypotension Conduction delay and myocardial depression |
|
|
What is the MOA of gabapentin and pregabalin?
|
□ Does not act via GABA receptors
□ Binds to α₂δ-1 subunits of presynaptic voltage-gated Ca2+ channels □ Reduces release of glutamate, NE, substance P, and CGRP |
|
|
What is the MOA of tramadol?
Uses? Side effects? |
Synthetic opioid
• Weak μ-agonist activity • Inhibits serotonin and NE reuptake • Peripheral local anesthetic properties Uses • Postherpetic neuralgia • Diabetic neuropathy • Polyneuropathies • Post-amputation pain Adverse events • Reduced seizure threshold |
|
|
What are the uses of calcium channel α₂δ-1 ligands?
|
In chronic neuropathic pain
-Diabetic neuropathy -Postherpetic neuralgia -MS -Cancer-related neuropathic pain |
|
|
What are the uses for topical capsaicin?
|
- Diabetic neuropathy
- Postherpetic neuralgia |
|
|
Uses of cannabinoids for chronic pain.
|
A buccal spray is used for neuropathic pain from MS.
|
|
|
What are the four tracts in the anterolateral system?
|
Neospinothalamic
- from spinal cord to VPL thalamus Paleospinothalamic - from spinal cord to DM thalamus and intranuclear nuclei Spinomesencephalic - from spinal cord to PAG Spinoreticular - from spinal cord to reticular formation, which then projects to intralaminar nuclei, and then diffusely to cerebral cortex |
|
|
Which of the anterolateral tracts mediate...
a) sensory, discriminative component, sharp pain? b) Affective, motivational component and dull aching pain? c) Modulation of pain? |
a) Neospinothalamic
b) Paleospinothalamic, spinoreticular c) Spinoreticular, spinomesencephalic |
|
|
What is the diagnostic criteria of a migraine without aura?
|
At least 5 attacks that fulfill:
2 of the following: - unilateral location - throbbing quality - worse with exercise - moderate to severe intensity 1 of the following: - nausea or vomiting - phonophobia and photophobia |
|
|
What are the qualities of a tension-type headache?
|
Non-throbbing quality
Bilateral Mild to moderate intensity No aggravation with activity No nausea or vomiting No photophobia or phonophobia (or only 1 present) |
|
|
What are the characteristics of a cluster headache?
|
Severe unilateral orbital pain
Short duration (often just for a few minutes) Nocturnal episodes Can have up to 8 attacks per day, with clusters of attacks that can go for 7 days to 12 months. Restlessness - patients want to bang head Associated symptoms include - conjunctival injection - autonomic outflow (tearing, rhinorrhea) - rarely, ptosis and miosis |
|
|
What is the treatment of choice for paroxysmal headaches?
|
Indomethicin
|
|
|
What is the first line treatment for trigeminal neuralgia?
|
Carbamazepine
|
|
|
Pharmacological management of migraines (mild, moderate, and severe attacks)
Migraine preventative agents. |
Mild attacks
• ASA or NSAIDs Moderate attacks • Triptan • Combination analgesics / opioid Severe attacks • Triptan • Opioid for rescue Preventative agents • Beta blockers (nadolol) • TCA (amitriptyline) • Ca2+ channel blockers (flunarizine) • Serotonergic agents • GABA-minergic agents • Botulinum neurotoxin A |
|
|
Cluster headache treatment
- Acute therapy - Preventative therapy |
Acute therapy
• DHE intranasal / subcutaneous • Sumatriptan intranasal / subcutaneous • Oxygen inhalation (7 L / min) Preventative therapy • Verapamil • Prednisone • Topiramate • Methysergide • Lithium • Divalproex |
|
|
What happens if mammillary bodies are damaged?
|
Korsakoff's psychosis
- loss of memory - intelligence is intact |
|
|
Klüver-Bucy syndrome
|
Bilateral damage to amygdala
- Changes in aggression, emotional expression. - Complete lesion → docility, fearlessness - Partial lesion → bursts of aggression - Visual agnosia - Hypersexuality - Inappropriate attention to sensory stimuli |
|
|
There are three types of fibers in the brain: those that connect areas within the same hemisphere, those that connect area from one hemisphere to area in other hemisphere, and those that go in and out of the cortex. What are the these types of fibers each called?
|
Association fibers
Commissural fibers Projection fibers |
|
|
Which neurons are more able to regenerate - peripheral neurons or central neurons?
|
Peripheral neurons, because they can create growth cones, which follow Schwann cell tubes back to their original targets.
|
|
|
What is ephaptic transmission?
|
One naked axon causing firing of adjacent axon.
Often occurs due to demyelination, which allows ions to leak and affect adjacent neurons. |
|
|
Definition of dysesthesia vs paresthesia.
|
Dysesthesia = abnormal sensation of stimulus
Paresthesia = burning, prickling, tingling with no stimulus |
|
|
In electromyography, what is an F-wave? What does a prolonged F-wave indicate?
|
When a nerve is stimulated distally, it has orthodromic and antidromic AP. The antidromic AP travels up motor neuron into spinal cord, where a small portion of motor neurons will backfire, and travel back down nerves to the muscle. This causes the F-wave. A prolonged F-wave can reveal proximal nerve damage.
|
|
|
What are the antibodies directed at in myasthenia gravis?
|
Acetylcholine receptors
(Anti-AChR antibodies) |
|
|
What is a Ruffini's corpuscle?
|
A type of nerve receptor that is sensitive to skin stretch, sense of position and movement.
|
|
|
What is synesthesia?
|
Phenomenon where stimulation of one sensory mode leads to experiences in another sensory mode.
E.g. grapheme - numbers and letters are associated with different colours |
|
|
What do Merkel receptors sense?
|
Vibrations at low frequencies
|
|
|
What are the 4 attributes of a sensory stimulus?
|
1. Modality
2. Intensity 3. Duration 4. Location |
|
|
Properties of the sensory system that enable two-point discrimination
|
1. Receptor density
2. Size of the receptive fields |
|
|
What is a reliable post-natal test for FASD?
|
Test the fetus' hair or meconium for FAEE (fetal acid ethyl esters)
|
|
|
What pathogens often precede the development of Guillain Barre Syndrome?
|
Campylobacter jejuni
Less commonly: HIV, CMV, EBV |
|
|
What is a characteristic finding on lumbar puncture of a patient with GBS?
|
Elevated CSF protein, with normal WBC count.
This is believed to be caused by increased permeability of blood-nerve-barrier. |
|
|
What are the treatment options for Guillain Barre Syndrome?
|
Choose one or the other:
1) IVIG 2) Plasmapheresis (plasma exchange to get rid of the auto-antibodies) |
|
|
What happens to vitals in GBS?
|
They have dysautonomia: tachycardia, hypertension, tachypnea due to respiratory muscle weakness, arrhythmia.
|
|
|
Sympathetic post-ganglionic neurons are derived from...
|
Neural crest cells
|
|
|
What is the clinical course of Guillain Barre Syndrome if left untreated?
|
2 weeks of progression
Followed by 2-4 weeks of plateau Recovery starts in 60% of patients by week 4 of onset 80% of patients will fully recover or have only minor deficits 10% will have prolonged course with incomplete recovery 5% will die even with intensive treatment Treatment with IVIg or plasmaphoresis speeds up recovery |
|
|
What is a Renshaw cell?
|
A type of inhibitory neuron:
i. Located at lateral horn ii. Has recurrent inhibition loop • Innervated by motor neurons to give recurrent inhibition of these same motor neurons. This regulates motor neuron firing rates. |
|
|
How does tetanospasmin cause muscle spasms?
|
1. Tetanospasmin is taken up by α-motor neuron terminals, and transported retrograde to Renshaw cell.
2. In Renshaw cell, it cleaves proteins needed for release of glycine. Glycine is the neurotransmitter that Renshaw cells use to inhibit α-motor neurons 3. Since glycine release is prevented, there is no inhibition of the α-motor neurons. |
|
|
How does strychnine poisoning cause muscle spasms?
|
It is a glycine receptor antagonist. Glycine is the NT that Renshaw cells use to inhibit α-motor neurons.
|
|
|
What is the function of the reticulospinal tract?
|
• Automatic posture and gait-related movements
• Influence voluntary movement and muscle tone • Autonomic functions and pain impulses |
|
|
What is the Bing reflex?
|
A sign of UMN lesion:
- Get extension rather than flexion of ankle if dorsum of toe or foot is pricked with pin. |
|
|
What causes the clasp knife reflex?
|
It occurs with an UMN lesion.
Mechanism: □ In a normal situation where the triceps muscle is contracting (and thus feeling tension), the GTO inhibits the motor neuron to triceps, to prevent it from getting over-stretched and damaged. □ In the case of a clasp knife reflex, it is getting stretched because the examiner is trying to flex the elbow against the increased tone caused by the UMN lesion, and thus the GTO suddenly causes relaxation of the tricep muscle. |
|
|
What is the MOA of baclofen?
|
Activates presynaptic GABA(B) receptors, which causes hyperpolarization and decreases release of glutamate.
|
|
|
What is the MOA of diazepam?
|
Increases frequency of opening of GABA(A) receptors, which enhances post-synaptic inhibition, via hyperpolarization of postsynaptic membrane.
|
|
|
What is gliosis?
|
Proliferation of astrocytes in the CNS that eventually leads to scarring
|
|
|
What are the different opioid receptors, their prototype agonists, and actions?
|
Mu1 (μ1), Morphine, Supraspinal analgesia
Mu2 (μ2), Morphine, Respiratory depression Delta (δ), Enkephalins, Spinal analgesia Kappa (κ), Dynorphin A, Spinal analgesia and sedation NOP (ORL1), Nociceptin/orphanin FQ, Not yet fully understood |
|
|
What is the MOA of opioids?
|
1. Postsynaptic hyperpolarization by opening K+ channels
2. Presynaptic closing of Ca2+ channels, which prevents release of excitatory NTs 3. Activation of inhibitor enkephalin interneurons 4. Activation of descending inhibitory pathways |
|
|
Name 3 synthetic opioids
|
Meperidine (Demerol)
Fentanyl Methadone |
|
|
Which class of opioids does mepiridine and fentanyl fall under?
Which class of opioids does morphine, hydromorphone, and codeine fall under? |
Phenylpiperidines
- mepiridine - fentanyl Phenanthrenes - morphine - hydromorphone - codeine |
|
|
What receptors does an opioid receptor agonist-antagonist work on?
|
Agonist at kappa receptors, antagonist at mu receptors.
|
|
|
What is the relative potencies of morphine, fentanyl, codeine, and hydromorphone?
|
Most potent: fentanyl (100X potency of morphine)
next: hydromorphone next: morphine last: codeine |
|
|
Describe the metabolism of morphine and mepiridine
|
Morphine
- liver metabolizes into active metabolites - morphine-6-glucuronide - causes respiratory depression - morphine-3-glucuronide - causes seizures - metabolites are excreted by kidney. Therefore, must dose adjust for patients with renal failure. Can alternatively give them fentanyl. Mepiridine - metabolized by liver into normepiridine, which can cause seizures - also contrainidicated in renal failure |
|
|
What is remifentanil used for?
|
It is an opioid, used for continuous IV infusion in anesthesia. It is good for this, because it is rapidly metabolized by esterases.
|
|
|
What are some peripheral effects of opioids?
|
• Constipation
• Urinary retention • Constriction of sphincter of Oddi □ Biliary colic • Histamine release • Bradycardia • Hypotension □ Due to vasodilation |
|
|
How does opioid treat acute pulmonary edema?
|
Morphine causes pulmonary vasodilation
|
|
|
What is the clinical triad of opioid overdose?
What is the treatment? |
1. Coma
2. Miosis 3. Respiratory depression Treat with 100% O2 and iv Naloxone |
|
|
What is a potential drug interaction that must be cautioned with mepiridine?
|
Mepiridine with MAO inhibitors will cause hyperpyrexic coma (loss of consciousness with increased body temperature)
|
|
|
What are the structures that suspends the cord in the dura/arachnoid tube called?
|
Denticulate ligament - thickening of pia and glial elements
|
|
|
What levels does Clarke's nucleus extend through?
|
C8 to L3
|
|
|
What innervates the following:
Pain and temperature of the bladder fundus? Pain and temperature of the bladder neck? Sensation of fullness of bladder? Detrusor muscle? Internal urethral sphincter? External urethral sphincter? Pontine micturition center? |
Pain and temperature of the bladder fundus - sympathetic T12,L1
Pain and temperature of the bladder neck - parasympathetic S2-4 Sensation of fullness of bladder - parasympathetic S2-4. When moderately full, it is through SThTract. When very full, it is via dorsal column. Detrusor muscle - parasympathetic S2-4 → hypogastric plexus → synapse in vesical plexus → detrusor muscle Internal urethral sphincter - sympathetic T11-L2 (lumbar splanchnic → inferior mesenteric ganglioni → internal urethral sphincter) External urethral sphincter - S2-4 pudendal nerve via Onuf nucleus Pontine micturition center - PAG and superior frontal gyrus on medial surface |
|
|
Describe the sacral reflex pathway of bladder voiding
|
Occurs in infants, and people with spinal cord injury.
1. Stretch receptors in bladder wall are activated 2. Stretch receptors transmit via afferent fibres to sacral cord 3. Efferent parasympathetic nerve cell bodies are activated 4. Ach release by parasympathetics cause contraction of detrusor muscle 5. In infants, there is no control over external sphincter 6. In adults, the external sphincter is under somatic control through pudendal nerve |
|
|
Name the branches of the:
- vertebral arteries - basilar artery - internal carotid arteries |
Vertebral arteries
- PICA - anterior and 2 posterior spinal arteries Basilar artery - AICA - Superior cerebellar arteries - Pontine arteries Internal carotid arteries - ACA - MCA |
|
|
What proportion of the spinal cord does the anterior spinal artery and the 2 posterior spinal arteries supply?
|
ASA - anterior 2/3 of spinal cord
PSA - posterior 1/3 of spinal cord |
|
|
What are coronal arteries?
|
They are anastomosing arteries between anterior spinal artery and posterior spinal arteries.
|
|
|
What are radicular arteries?
|
Branches of cervical, intercostal, lumbar and sacral arteries that anastomose with coronal arteries, ASA and PSAs.
Supplies lower parts of the spinal cord (from lower cervical portion downwards). |
|
|
Where does the artery of Adamkiewicz arise from? What does it supply?
|
• Present at ~T12, arises from a branch of the aorta, and connects to the anterior spinal artery.
• Provides major supply for lumbosacral spinal cord. |
|
|
Describe the efferent pathways that mediate penile erection. Which spinal levels do the nerves arise? What kind of nerves are they (sympathetic or parasympathetic)?
|
Sympathetic fibers T10-L3
- psychogenic erection - if there is a SCI at sacral level, then reflexogenic pathway won't work, but psychogenic erections are still possible. Parasympathetic fibers S2-4 - reflex erection - if there is SCI above T9, then psychogenic reflex pathway won't work, but can still have reflexogenic erections. |
|
|
What is the MOA of erectile dysfunction drugs such as viagra, cialis and levitra?
|
PDE-5 (phosphodiesterase) inhibitors. PDE-5 usually converts cGMP into guanosine monophosphate. By increasing the amount of cGMP, which relaxes smooth muscle, which facilitates blood flow into the erectile tissue.
|
|
|
What are the two stages of ejaculation? Which levels of the spinal cord mediate each stage?
|
Stage 1: seminal emission
- sympathetic T10-12 - seminal fluid formation - sympathetic L1-2 - close internal urethral sphincter to prevent retrograde ejaculation Stage 2: expulsion - parasympathetic S2-4 - contractions of seminal vesicles, prostate, urethra - somatic S2-4 - contractions of bulbospongiosus, ischiocavernosus, levator ani |
|
|
What happens to ejaculation in men with complete lesion above T10? below T10?
|
Note that ejaculation requires intact T10-S4 segments.
Above T10 - still possible to trigger ejaculation reflex through vibrostimulation Below T10 - disturbs the lumbosacral reflex. Ejaculation still possible with more intense form of stimulation - electroejaculation (stimulation of efferent nerves through rectum) |
|
|
Bulbocavernosus reflex - significance of positive/negative result in the setting of SCI.
|
Positive - level of injury is above lumbar level
Negative - sacral injury |
|
|
Testicular squeeze test - significance of positive/negative result in the setting of SCI.
|
Positive (painful) - SCI must be below T9
Negative (not painful) - SCI must be T9 or above |
|
|
Pinprick test on genitalia - significance of positive/negative result in the setting of SCI.
|
Positive (painful) - incomplete SCI - spinothalamic tract was spared
Negative (not painful) - sacral SCI, or spinothalamic tract affected, or sacral dermatome affected. |
|
|
Test anal tone - significance of positive/negative result in the setting of SCI.
|
Positive - T10-S4 is open and communicating, so SCI is above T10
Negative - lesion is between T10-S4. May explain ejaculation disorder. |
|
|
With SCI above level of T6, can get autonomic dysreflexia with certain stimuli below the level of the SCI. Describe what happens.
|
Bradycardia
Above the level of the lesion: □ Spontaneous hypertensive crisis □ Sweating □ Headache Below the level of the lesion: □ Vasoconstriction □ Piloerection The main mechanism is increased adrenergic receptor sensitivity below level of lesion, and inability of compensatory parasympathetic signals from brain to reach level below SCI. |
|
|
What is the significance of a negative pinprick to genitalia and no voluntary anal contraction?
|
No genital orgasm possible.
|
|
|
Which area of the spinal cord is most susceptible to anterior spinal artery infarct? Why?
|
Mid-thoracic T4-8, because there is often only one small radicular vessel that supplies that anterior spinal artery at this level.
|
|
|
What are the neurological manifestations of subacute combined degeneration?
|
Demyelination of posterior columns and lateral columns (corticospinal tract and spinocerebellar tract).
Affects legs > arms Starts with loss of vibration and proprioception. Weakness/paralysis follows. |
|
|
Which tract must be intact for genital orgasms to occur?
|
Lateral corticospinal tract
|
|
|
What is the name of the vestibular sensory epithelia of the semicircular canals? otoliths?
|
Semicircular canals - cristae
Utricle/saccule - maculae |
|
|
What is the acellular gelatinous mass within the ampulla of the semicircular canals called?
|
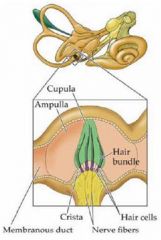
Cupula
|
|
|
What is the acellular gelatinous mass in the otoliths called?
|
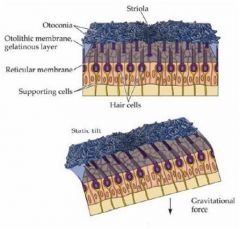
Otolithic membrane
|
|
|
What is synonymous with the medial vestibulospinal tract?
|
Descending MLF
|
|
|
Does the facial motor nucleus (VII) receive bilateral, unilateral, or contralateral projections from the corticobulbar tract?
|
It is special.
It receives bilateral projections for the rostral part. It receives contralateral projections for the caudal part. The significance is that a UMN lesion will affect the lower face on the contralateral side, but not the upper face. But a LMN lesion will affect both the upper and lower face on the ipsilateral side. |
|
|
Locate the oculomotor, trochlear and abducens nuclei.
|
|
|
|
Draw out the different pathways for the three types of conjugate eye movements.
|

|
|
|
Please draw how the cranial nerve nuclei develop in 7 columns
|

|
|
|
What artery supplies the eye?
|
The opthalmic artery, which is a branch of the internal carotid.
Ophthalmic artery splits into: - posterior ciliary artery (choroid, outer retina and optic disc) - central retinal artery (inner retina) |
|
|
Difference between rods and cones in terms of ...
- colour/greyscale - resolution - better during day or night |
Rods
- night - low resolution (spatial and temporal) - greyscale Cones - better during the day (bright light) - high resolution (temporal and spatial) - colour |
|
|
What would a transection at the following sites cause, in terms of visual field loss?
- optic nerve - optic chiasm - optic tract |
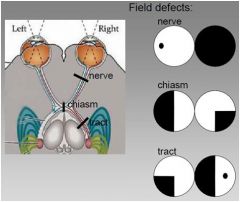
Optic nerve
- unilateral complete blindness Optic chiasm - bilateral hemianopsia Optic tract - homonymous hemianopsia |
|
|
What are the lower fibers of the optic radiations that loop around the inferior horn of lateral ventricle called?
|
Meyer's loop. They convey upper visual field info.
|
|
|
What are the two extra-striate pathways' functions?
|
Dorsal (occipito-parietal) stream:
- motion, depth, visuospatial, hand/eye movements Ventral (occipito-temporal) stream: - colour, recognition of words and faces |
|
|
What do you call the impaired recognition of faces?
|
Prosopagnosia
|
|
|
What is the pathway of control over dysconjugate gaze?
|
Visual association cortex → pretectum (convergence centre) → oculomotor nucleus for convergence, abducens nucleus for divergence
|
|
|
What changes would you see in the eyelids and pupils of a person with a third nerve palsy?
What is the most common cause of third nerve palsy? |
Ipsilateral ptosis and mydriasis.
Posterior communicating artery aneurysm, or internal carotid artery aneurysm, compressing CN III |
|
|
Which extraocular muscle receives innervation from the contralateral oculomotor nucleus?
|
Superior rectus.
|
|
|
What is the name of the condition when the MLF becomes demyelinated?
|
INO: internuclear ophthalmoplegia. Causes medial rectus to be weak.
|
|
|
Which meningeal layers are included in the term "leptomeninges"?
|
Pia and arachnoid mater.
|
|
|
What space does acute bacterial meningitis usually affect?
|
Subarachnoid space
|
|
|
Which organisms are the most frequent causes of acute bacterial meningitis?
|
Pneumococcus
Hemophilus influenzae Meningococcus |
|
|
What are the 3 forms of tertiary syphilis, and their presentations?
|
Tabes dorsalis - damage to posterior column and dorsal roots, and cranial nerves. Sensory ataxia and lancinating pains.
Meningovascular neurosyphilis - vasculitis with chronic meningitis. Headache, dizziness, personality changes, stroke. Paretic neurosyphilis - encephalitis, causing nerve destruction. Dementia. Less commonly - depression, mania, or psychosis |
|
|
What kinds of pathogens can cause meningoencephalitis?
|
Fungi (mucormycosis [vasculitis], and crytococcus [brain and meninges])
Syphilis Tuberculosis |
|
|
What is a prion disease caused by?
|
Abnormal isoform of the prion protein (PrP), which is a normal cell membrane protein in neurons.
- acquired mutations of PrP - familial causes - acquired by eating animals |
|
|
What is the name of the condition that causes the swinging flashlight test to be abnormal (eyes dilate when swung to the eye with the disease).
|
Optic neuritis, often caused by MS.
The pupil response is called Marcus-Gunn pupil. |
|
|
What is Argyll-Robertson pupil?
|
A pupil that can accommodate (constrict) to close vision, but does not react (constrict) to light.
Caused by syphilis. |
|
|
What are the variable disease patterns of multiple sclerosis?
|
- Relapsing remitting
- Secondary progressive - Primary progressive - Progressing relapsing |
|
|
What is the mean survival time from symptom onset of multiple sclerosis? What do they die of?
|
38 years from time of symptom onset.
Die from respiratory disease or infection. |
|
|
Do multiple sclerosis plaques appear hyperintense or hypointense on MRI (T1/T2)?
|
T1 MRI: hypointense
T2 MRI: hyperintense |
|
|
What should be ordered in a diagnostic workup of suspected multiple sclerosis?
|
MRI
CSF analysis - WBC are high, protein is normal or high, IgG is high (often with oligoclonal banding) |
|
|
What are the disease modifying treatments for multiple sclerosis?
How about for acute attacks? |
Interferon
Glatiramer acetate - a mixture of proteins with similarities in composition to myelin, acting as a decoy. For acute attacks, use glucocorticoids. |
|
|
What is the location of a lesion that causes spatial hemineglect?
|
Usually the right sensory association area.
|
|
|
What is the location of a lesion that causes visual agnosia?
|
Visual association area
|
|
|
If there is damage to the frontal eye field on the right hemisphere, which way will the eyes deviate?
|
The eyes will deviate to the right.
This is due to unopposed contraction of extraocular muscles |
|
|
What percentage of right handed people are right-hemisphere dominant?
|
Only 15%.
70% are still left-hemisphere dominant. 15% have bilateral language representation. |
|
|
What is the deficit when the expressive language area is damaged?
|
Broca's aphasia
- nonfluent aphasia, difficulty producing language - telegraphic speech - agraphia - comprehension is intact, and person is aware of language problem |
|
|
What is the deficit when the receptive language area is damaged?
|
Wernicke's aphasia
- fluent aphasia, speech is fluent but non-sensical - Comprehension is impaired, and person is unaware of language problem |
|
|
What happens if the fibers connecting Wernicke's and Broca's area are damaged? What are these fibers called?
|
The fibers are called arcuate fasciculus.
Conduction aphasia - difficulty with speech repetition. Comprehension is intact. Fluent, but paraphasic speech. Patient will be aware of their mistakes, but have difficulty correcting them. |
|
|
Which nucleus of the thalamus does the frontal association cortex have connections with?
|
DM nucleus
|
|
|
What artery gives rise to the anterior choroidal artery? What does it supply?
|
Usually the internal carotid artery. Sometimes the MCA.
Supplies globus pallidus, putamen, thalamus, and posterior limb of internal capsule. |
|
|
What artery gives rise to the anterior lenticulostriate arteries? What do they supply?
|
Medial branches: ACA
Lateral branches: MCA Supplies basal ganglia and internal capsule. |
|
|
What does "striatum" refer to?
|
Caudate and putamen.
|
|
|
What vein does the great cerebral vein (of Galen) drain into?
|
Inferior saggital sinus, which then drains into straight sinus.
|
|
|
Is reading comprehension impaired in Broca's aphasia?
|
Yes, for syntax.
|
|
|
What are the primary features of the following syndromes of the frontal lobe:
- orbitofrontal syndrome - dorsolateral frontal syndrome - medial frontal syndrome |
Mnemonic: ODDEMA
- orbitofrontal syndrome: disinhibition - dorsolateral frontal syndrome: executive dysfunction - medial frontal syndrome: apathy |
|
|
Describe the areas that are involved in planning and executing a complex movement.
|
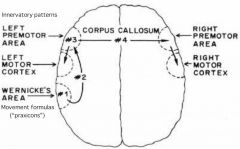
|
|
|
Difference between apperceptive and associative agnosia when the patient is told to copy a picture.
|
Apperceptive - they can't copy shapes.
Associative - they can copy shapes, but they can't recognize what it is. |
|
|
What is a common cause of prosopagnosia?
|
Because the facial recognition area is in the right occipitotemporal area, a right PCA territory infarct often is the cause of prosopagnosia.
|
|
|
In an acute stroke, will the eyes deviate towards or away from the site of the lesion?
|
Towards.
|
|
|
Which thalamic nuclei does the ascending reticular activating system project to?
|
Intralaminar nuclei, and reticular nuclei. These, in turn, project to all parts of the cortex.
|
|
|
What are these categories of reduced consciousness called:
i) A patient with severely altered consciousness, with inconsistent evidence of willful actions associated with consciousness ii) A patient with no evidence of awareness, does not respond meaningfully, but has some spontaneous movements and reflexes, lasting for > 3 months. iii) A patient who has no evidence of conscious sensations, reflexes, or movement. |
i) Minimally conscious state
ii) Permanently vegetative state (need to have the symptoms for 3 months to call it this) iii) Coma |
|
|
What is the MOA of inhaled anesthetics?
|
• Facilitation of inhibition
□ ↑GABA(A) receptor-mediated transmission □ ↑background (leak) K+ conductance (K+ leaks out of cells, hyperpolarizing cells) • Inhibition of excitation □ ↓glutamate receptor-mediated transmission □ ↓ACh receptor-mediated transmission |
|
|
What controls these properties of inhaled anesthetics?
- Onset - Toxicity - Potency |
Onset
- blood solubility. The more soluble (the higher the blood/gas partition coefficient), the longer it takes to induce anesthesia. Toxicity - solubility in blood. The more soluble in blood, the higher the rate of metabolism. The faster the metabolism, the greater the potential for toxicity. Potency - lipid solubility. The more lipid soluble, the greater the potency (and therefore the lower the MAC of the drug). |
|
|
Name 3 i.v. anesthetics
|
Thiopental
Propofol Ketamine |
|
|
What is the difference in MOA for thiopental, propofol and ketamine?
|
Thiopental - GABA(A) agonist
Propofol - GABA(A) agonist Ketamine - NMDA (a type of glutamate receptor) antagonist |
|
|
What is special about thiopental in contrast to the other i.v. anesthetic drugs?
|
-No analgesic properties
-Rapidly redistributed, so not good for maintenance of anesthesia. Only used for induction of hypnosis -Causes histamine release -Arterial occlusion is possible |
|
|
What is special about propofol in contrast to the other i.v. anesthetic drugs?
|
- No significant redistribution - can be infused for maintenance of anesthesia
- Rapid awakening (even faster than thiopental) - Pleasant dreams - Antiemetic properties - Pronounced hypotension - Injection pain - Potential for sepsis |
|
|
What is special about ketamine in contrast to the other i.v. anesthetic drugs?
|
- Dissociative anesthesia (catatonia, amnesia, analgesia)
- Little cardiorespiratory depression - Maintains airway reflexes - Different MOA - NMDA antagonist - Unpleasant dreams |
|
|
Equation to determine cerebral blood flow?
|
CBF = CPP / CVR
CPP is cerebral perfusion pressure CPP = MAP - ICP. This tells you that with increased ICP, there is less CBF. CVR is cerebral vascular resistance |
|
|
Equation to determine cerebral perfusion pressure?
|
CPP = MAP - ICP
|
|
|
What is Cushing response?
|
Hypertension, bradycardia, and erratic respiration, due to increased ICP
|
|
|
What is the lifetime risk of brain tumour?
|
1 in 200
|
|
|
What is the most common type of brain cancer? What is its 5 year survival rate?
|
Glioblastoma.
5 year survival of 3% only. |
|
|
What is the significance of the MGMT protein in glioblastoma?
|
MGMT is a DNA repair protein.
Patients with high MGMT gene level/activity are likely to have resistance against temozolomide (an alkylating agent). If MGMT levels are low due to gene promoter region methylation, they have good treatment outcome with temozolomide. |
|
|
What is the significance of LOH 1p gene in oligodendroglioma?
|
Associated with good response to chemotherapy.
|
|
|
What are the main categories of CNS tumours?
|
Glioma
- astrocytoma - oligodentroglioma - ependymoma Neuroma Meningioma |
|
|
What are the main categories of cranial and spinal nerve tumours?
|
Schwannoma
Neurofibroma Malignant peripheral nerve sheath tumour |
|
|
What kind of cancers are most likely to metastasize to the brain?
|
• Lung - 50%
• Breast - 15% • Skin (melanoma) - 10% • GI • GU - 5% |
|
|
What is the afferent and efferent pathway for the gag reflex, including the nuclei?
|
Brush posterior pharynx -> glossopharyngeal -> nucleus solitarius -> nucleus ambiguus -> vagus -> striated muscles of the pharynx
|
|
|
Which artery is most likely to be compressed by a transtentorial uncal herniation?
|
PCA
|
|
|
Which artery is most likely to be compressed by a subfalcine herniation?
|
ACA
|
|
|
Monoaminergic nuclei of the reticular formation, and what monoamine do they produce?
|
Ventral tegmental area - dopaminergic neurons
Raphe nucleus - serotonergic neurons Locus ceruleus - noradrenergic neurons |
|
|
What is status epilepticus?
|
The occurrence of a single unremitting seizure with a duration longer than 5 to 10 minutes or frequent clinical seizures without an interictal return to the baseline clinical state.
|
|
|
Which areas does the glossopharyngeal carry general somatic afferent (GSA) fibres from?
|
Posterior 1/3 of tongue
Tonsils Pharynx Inner surface of tympanic membrane Skin of external ear |
|
|
Which areas does the vagus nerve carry general somatic afferent (GSA) fibres from?
|
Pharynx
Larynx Outer surface of tympanic membrane Skin of external ear Posterior meninges Concha |
|
|
Which skeletal muscles does vagus nerve innervate?
|
Cricothyroid
Intrinsic laryngeal muscles Salpingopharyngeus Palatopharyngeus Sup, mid, inf constrictors Levator palatini Palatoglossus |
|
|
Name inhaled anesthetics, in order of highest rate of metabolism to lowest.
|
Methoxyflurane - hepato and nephrotoxicity
Halothane - hepato and nephrotoxicity Sevoflurane - low potential for toxicity Isoflurane - low potential for toxicity Desflurane - resistant to metabolism Nitrous oxide - ?toxicity of free radicals |
|
|
List the 3 factors that regulate cerebral vascular resistance.
|
Pressure autoregulation
PaO2 and PaCO2 Cerebral metabolism * Note that sympathetics and parasympathetics have no major role in regulating CVR. |
|
|
Name 4 epilepsy syndromes.
|
1. Benign childhood epilepsy with centrotemporal spikes
2. Juvenile myoclonic epilepsy of Jans 3. West syndrome 4. Lennox-Gastaut syndrome |
|
|
What are the major differences between gabapentin and pregabalin?
|
Pregabalin has more linear pharmacokinetics, which is better for renal/liver failure patients. It can also be used as an anxiolytic.
|
|
|
What does an area of the brain that has died from ischemia look like on CT scan?
|
It appears hypodense.
White matter looks like grey matter. |
|
|
Where do interneurons that are responsible for pain modulation reside?
|
In the substantia gelatinosa of dorsal horn, laminae II.
Receives descending input from PAG, and also from large diameter afferents conducting touch. |
|
|
MOA of triptans.
What are the adverse effects? |
Selective serotonin agonist in cranial arteries, causing vasoconstriction and reduction in inflammation.
Adverse effect: constricts coronary arteries, therefore contraindicated in patients with ischemic heart disease. |
|
|
MOA of dihydroergotamine
|
Non-specific serotonin agonist, causing peripheral and cerebral arteries to vasoconstrict
|
|
|
What is the difference between classic trigeminal neuralgia, and secondary trigeminal neuralgia?
|
Classic TN - caused by vascular compression on TN
Secondary TN - caused by structural lesions other than vascular compression |
|
|
What areas of the face are often affected by trigeminal neuralgia?
|
It is usually unilateral, but sometimes bilateral, but never on both sides simultaneously.
Usually involves V₂ or V₃, but almost never V₁ |
|
|
What is the major complication of treating trigeminal neuralgia with surgery (rhizotomy, or thermocoagulation)?
|
Anesthesia dolorosa - persistent painful anesthesia in the denervated area.
|
|
|
What 4 functions do the hypothalamus and limbic system work together to maintain?
|
1. Endocrine secretion
2. Autonomic function 3. Homeostasis 4. Emotion and basic drives |
|
|
Which area of the hypothalamus...
- activates parasympathetic responses? - responds to ↑ temperature (heatloss center)? - is the feeding center? - stimulates sleep? |
Parasympathetic - anterior
Heat loss - anterior Feeding area - lateral Sleep inducing - anterior |
|
|
What is the medial forebrain bundle?
|
Dopaminergic connections between the ventral tegmental area (VTA) and the nucleus accumbens.
|
|
|
What are the neural substrates for addiction?
|
-medial forebrain bundle
-amygdala -hippocampus -hypothalamus -frontal and prefrontal cortex |
|
|
In psychiatry, what is the difference between temperament and character?
|
Temperament = genetically encoded behaviour
Character = acquired through environment |
|
|
What are the 5 main dimensions of personality?
|
1. Emotional stability
2. Extroversion 3. Openness 4. Agreeableness 5. Conscientiousness |
|
|
Name all of the personality disorders, and how they are organized.
|
Cluster A - odd or eccentric
-Paranoid -Schizoid -Schizotypal Cluster B - dramatic, irrational -Borderline -Antisocial -Histrionic -Narcissistic Cluster C - anxious, fearful -Dependent -Avoidant -OCPD |
|
|
Which psychiatric disorders has cognitive behavioural therapy NOT been useful for?
|
Panic attacks/agoraphobia, and generalized anxiety disorder.
|
|
|
What classes of drugs are used as first line treatment of anxiety disorders?
|
SSRIs
SNRIs Benzodiazepines |
|
|
How long do you generally need to treat mood disorder with SSRIs before they start to have an effect?
|
6 weeks before they start to work
|
|
|
What is BDNF?
|
BDNF (brain derived neurotropic factor)
- under stress, cortisol is released, and may suppress gene for BDNF - chronic hypercortisolemia may cause low BDNF, which leads to neuronal loss, and may cause mood disorders |
|
|
In depression, which NTs are involved in increased negative affect, and which are involved in decreased positive affect?
|
Increased negative affect: 5-HT, NE
Decreased positive affect: DA, NE |
|
|
What is a big concern with use of MAO inhibitors?
|
Tyramine reaction - can't metabolize tyramine, which gets converted into NE, and causes hypertension.
|
|
|
What is the name of a reversible monoamine oxidase inhibitor?
|
Moclobemide. It is safer than irrreversible MAOi's, which cause tyramine reaction, which can cause hypertensive crisis.
|
|
|
What are the side effects of TCAs?
|
H₁ antagonism
□ Sedation and weight gain M₁ antagonism □ Dry mouth □ Blurred vision □ Urinary retention □ Constipation α₁ antagonism □ Orthostatic hypotension □ Dizziness Voltage-gated Na+ channels □ Brain: seizures and coma □ Heart: arrhythmia, cardiac arrest, death |
|
|
Name the SSRIs, what they inhibit/activate, and which enzyme they are metabolized by.
|
FPFSCE
Fluoxetine - NRI, 5HT-2C agonist, 2D6, 3A4 Paroxetine - NRI, M1, 2D6 Fluvoxamine - opioid agonist, 3A4 Sertaline - opioid agonist, DRI Citalopram - 2D6 Escitalopram - the most clean of all the SSRIs |
|
|
Why can't SSRIs be stopped abruptly?
|
Will cause withdrawal symptoms, especially with paroxetine. Most significant symptom is flu-like symptom and sweating.
|
|
|
Why do DA levels increase with the use of SNRI?
|
There are few DA reuptake pumps in neurons of prefrontal cortex. NE reuptake pumps are responsible for uptake of both NE and DA in the PFC. So inhibition of those will increase DA.
|
|
|
Name an NDRI.
|
Buproprion
Ritalin (methylphenidate) |
|
|
Name an SARI (serotonin antagonist and reuptake inhibitor).
|
Trazodone - used for insomnia
• At low doses, it antagonizes 5HT2A, H₁, and α₁ receptors • High doses are required to inhibit 5HT reuptake transporters, which limits its usefulness as an antidepressant |
|
|
Name an NaSSA (noradrenergic and specific serotonergic antidepressant).
Which receptors does it antagonize? |
Mirtazapine
• α₂ antagonist at presynaptic terminal, which results in increased release of NE and serotonin • 5HT2A/5HT2C antagonists • 5HT2 antagonism • 5HT3 antagonism • H1 antagonism |
|
|
What drugs are used as second line agents for depression?
|
TCAs
Quetiapine Trazodone (which is a SARI) |
|
|
MOA of lithium.
|
□ Inhibition of inositol monophosphatase
□ Modulation of G proteins □ Reduction of protein kinase C activity, affecting genomic expression associated with neurotransmission |
|
|
List the mood disorders
|
1. Major depressive episodes
2. Manic episodes 3. Hypomanic episodes 4. Mixed mood episodes 5. Major depressive disorder 6. Dysthymic disorder 7. Bipolar I disorder 8. Bipolar II disorder 9. Cyclothymic disorder |
|
|
What is the DSM-IV criteria for major depressive disorder?
|
At least 5 of the SIGECAPSD symptoms for 2 weeks. One of them has to be depressed mood or lack of interest in things they normally enjoy.
|
|
|
Which drugs are used to treat bipolar?
|
Mood stabilizers
- lithium - valproic acid - carbamazepine - lamotrigine |
|
|
What is agoraphobia?
|
Fear of situations in which escape might be difficult or embarrassing if panic occurs.
Typically a result of panic disorder. |
|
|
List the anxiety disorders
|
Anxiety disorders
1. Generalized anxiety disorder 2. Panic disorder 3. OCD 4. Social phobia 5. Specific phobia 6. Post-traumatic stress disorder 7. Acute stress disorder |
|
|
How long do the symptoms of general anxiety disorder have to last before GAD can be diagnosed?
|
6 months
|
|
|
What classes of drugs are used to treat anxiety disorders?
|
SSRI, SNRI
Benzodiazepines |
|
|
What's the most prevalent anxiety disorder?
|
Social phobia
|
|
|
What elements should be covered in a suicide risk assessment?
|
SAD PERSONS
Sex (male) Age (< 19 or > 45) Depression Previous suicidal thoughts Ethanol Rational thought Social support Organized plan No spouse Sickness |
|
|
How does normal anxiety differ from that experienced in an anxiety disorder?
|
Duration, intensity, and impairment in functioning.
|
|
|
What are the symptoms of serotonin syndrome?
|
• Migraines
• Myoclonus • Diarrhea • Agitation and anxiety • Psychosis • Nausea • Dizziness • Disorientation • Shivering • Sweating • Increased BP • Hyperthermia • Seizures • Coma • Cardiovascular collapse • Permanent hyperthermic brain damage • Death |
|
|
What are the 3 major divisions of the cerebellar surface?
|
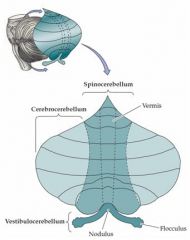
Cerebrocerebellum (aka neocerebellum)
• Posterior lobe • Topographical representation of the extremities, areas for eye movement and speech • Coordination of intricate and complex movements • Lesion causes dysmetria and dysdiadochokinesia Vestibulocerebellum (aka archicerebellum) • Flocculonodular lobe (and vermis) • Trunk control • Lesion causes truncal ataxia and nystagmus Spinocerebellum (aka paleocerebellum) • Vermis and anterior lobe • Synergistic movement of extremities • Lesion causes gait ataxia |
|
|
What are the negative and positive symptoms of schizophrenia?
|
Negative symptoms, mediated by too little DA in mesocortical pathway
- avolition - alogia - affect flattening Positive symptoms - mediated by too much DA in mesolimbic pathway - hallucinations - delusions - disorganized speech - catatonia |
|
|
What are extrapyramidal symptoms?
|
Caused by lack of DA action in the nigrostriatal pathway, people experience acute dystonic reaction, akathisia, pseudoparkinsonism, tardive dyskinesia.
|
|
|
What is the difference between low potency and high potency antipsychotics?
|
Low potency (chlorpromazine, clozapine, quetiapine) have tendency to cause sedation, weight gain, hypotension, and urinary retention, due to H₁, α₁, M₁ receptor antagonism.
High potency (risperidone, haloperidol, pimozide, perphenazine) have tendency to cause EPS. |
|
|
What is the difference between atypical and conventional antipsychotics?
|
In addition to the H₁, α₁, M₁ receptor antagonism, atypical antipsychotics also antagonize 5HT-2A receptors in the mesocortical, nigrostriatal, and tuberoinfundibular systems. Blocking 5HT-2A in DA neurons has the effect of increasing DA release. This reduces the NIDS, EPS, and hyperprolactinemia seen with conventional antipsychotics.
The draw back to atypicals is that they tend to cause more metabolic side effects (weight, DM, dyslipidemia). |
|
|
List the atypical antipsychotics.
|
• Paliperidone
• Risperidone • Olanzaprine • Ziprasidone • Aripiprazole • Clozapine • Quetiapine |
|
|
What can be used to treat the extrapyramidal symptoms caused by antipsychotics?
|
Anticholinergic agents
- benztropine - trihexphenidyl |
|
|
What is unique about clozapine compared to other antipsychotics?
|
It can cause agranulocytosis in 0.5-2% of cases, so cell counts need to be monitored in patients.
In addition, it has intrinsic anticholinergic action, so it has less EPS side effect. |
|
|
Which liver drug metabolizing enzyme does smoking affect, and in what way?
|
Induces 1A2
|
|
|
Which component of the substantia nigra contains the DA neurons?
|
Substantia nigra pars compacta
|
|
|
What are the names given to the groups of fibers that travel from the globus pallidus internal segment, to the thalamus?
|
Lenticular fasciculus - cuts through internal capsule, and passes dorsal to STN
Ansa lenticularis - loops ventrally under internal capsule The joining of these forms the thalamic fasciculus. |
|
|
Where does lesion occur in hemiballism?
|
Lesion in contralateral subthalamic nucleus, usually caused by a stroke.
|
|
|
Where is the lesion in Huntington's disease?
|
Autosomal dominant disorder, where there is degeneration of the striatum (caudate and putamen). Mostly affects the indirect pathway first, and then in later stages, affects both the indirect and direct pathways.
|
|
|
What are the four things that the basal ganglia is responsible for? What is the name of the circuits for each of these?
|
1. Motor circuit
2. Oculomotor circuit 3. Associative circuit - complex motor activity, newly learned movements 4. Limbic circuit - motor expression of emotion |
|
|
What is the name of the deep cerebellar nuclei, from lateral to medial?
|
Don't Eat Greasy Food
Dentate Emboliform Globose Fastigial |
|
|
What information is carried in corticopontine connections? What is the pathway?
|
They are part of the cerebrocerebellar system. Will project from frontal, parietal and temporal lobes, through medial and lateral 1/5 of crus cerebri, to ipsilateral pontine nuclei, cross in basal pons as transverse pontocerebellar fibers, and enter cerebellum via MCP.
Rate, rhythm and force of movement. Lesion causes dysmetria, dysdiadochokinesia. |
|
|
What is the purpose of the reticulospinal tract? Where in the spinal cord is it located?
|
Influences voluntary movement and tone. Located in the lateral and anterior white columns of the spinal cord.
|
|
|
What is the purpose of the rubrospinal tract? Where is it located?
|
Facilitates flexor activity, and inhibits extensor muscle activity.
Located in lateral white column of spinal cord, just lateral to corticospinal tract |
|
|
What are "climbing fibers"?
|
They are afferents arising from the olive, that project to contralateral cerebellum via inferior cerebellar peduncle.
|
|
|
What is the time period required for diagnosis of schizophrenia?
|
6 months of continuous signs, with at least 1 month of 2 or more characteristic symptoms (positive / negative symptoms)
|
|
|
What are the subtypes of schizophrenia?
|
1. Paranoid
2. Catatonic 3. Residual 4. Undifferentiated 5. Disorganized |
|
|
What is the main difference between schizophreniform disorder and schizophrenia?
|
In schizophreniform disorder, they have signs for at least one month, but less than 6 months
|
|
|
What is schizoaffective disorder?
|
They meet criteria for schizophrenia, and concurrently meet criteria for depressive episode (for 2 weeks), or manic or mixed episode (for 1 week)
They must also have presence of delusions or hallucinations for at least 2 weeks in the absence of mood symptoms. |
|
|
What is the time required to diagnose delusional disorder?
|
Non-bizarre delusions for at least 1 month.
|
|
|
What are the different types of delusions?
|
GPJEMS
1. Grandiose 2. Persecutory 3. Jealous 4. Erotomanic 5. Mixed - a combination of the different types 6. Somatic |
|
|
Symptoms and time required to diagnose brief psychotic disorder.
|
One of the positive symptoms (delusions, hallucinations, disorganized speech, disorganized behaviour) for > 1 day, but < 1 month.
|
|
|
Which drugs can induce psychosis?
|
• Marijuana
• Amphetamines • Cocaine • Hallucinogens |
|
|
Differences between Parkinson's tremor and essential tremor.
|
In Parkinson's:
- head tremor is uncommon - asymmetric - rigidity - writing is small, tremor not prominent - worse while walking - alcohol has no effect |
|
|
What is the treatment for Parkinson's disease?
|
Sinemet, which is levodopa and carbidopa.
Levodopa is metabolized into dopamine, which can cause nausea and vomiting outside of the BBB. Carbidopa effectively blocks the conversion of levodopa into DA, but carbidopa does not cross the BBB. This allows levodopa to cross the BBB and get metabolized, while minimizing emesis. |
|
|
Primary treatment for Huntington's disease.
|
Tetrabenazine
- DA depleting agent |
|
|
List the treatment for the following movement disorders:
Parkinson's disease Essential tremor Chorea Tics Ballism Dystonia |
Tremor
□ PD: levodopa, DA agonists □ Essential tremor: β blockers, anticonvulsants Chorea □ Tetrabenazine Tics □ Tetrabenazine Ballism □ Sedation □ Tetrabenazine Dystonia □ Anticholinergics □ Botox |
|
|
Indicate whether the following groups of cognitive functions would be impaired or unimpaired in delirium, amnestic syndrome, and dementia:
1. Attention 2. Recent memory 3. Frontal lobe function, calculation, language, visuospatial |
Delirium - all impaired
Amnestic syndrome - recent memory impaired Dementia - recent memory impaired, FCLV also impaired |
|
|
What are some key characteristics of delirium?
|
Reduced ability to focus, sustain or shift attention
Cognition decrease Fluctuation Sleep-wake reversal Sundowning |
|
|
Causes of delirium.
|
DIMSR
Drugs Infection Metabolic or Myocardia infarction Structural Retention (constipation, urinary) |
|
|
What genes can cause early-onset Alzheimer disease?
|
APP (amyloid precursor protein)
PSEN1 <- 78% of familial cases! PSEN2 The pathology of AD caused by these genes is ↑Aβ₄₂ protein. |
|
|
Who is eligible for genetic testing for familial Alzheimer disease?
|
• Can test 1st degree relatives of an affected individual with the mutation.
• First cousins of an affected individual if the common ancestors (parents who were siblings) died before the average age of onset of dementia. • Nieces or nephews of an affected individual whose parent (sibling of the affected individual) died before the average age of onset of dementia. |
|
|
Which gene confers a risk for developing Alzheimer disease?
|
ApoE gene
- promotes Aβ accumulation and senile plaque formation. - however, even with two E4 alleles, there is still only a very small risk of developing AD |
|
|
What does polysomnography measure?
|
EEG
EOG (electro-oculogram) EMG (submentalis) ECG |
|
|
What are some risk factors for obstructive sleep apnea?
|
Family history
Obesity Male Elderly Sedating medications Alcohol Smoking |
|
|
What sort of sleep disorder often occurs with Alzheimer disease?
|
Sleep apnea
|
|
|
What are some neuropathological findings in Alzheimer disease?
|
Senile plaques.
Neurofibrillary tangles. Dystrophic neurites (axons & dendrites). |
|
|
How does the Aβ42 protein get created in Alzheimer disease?
|
It is abnormal clipping of the Amyloid Precursor Protein (APP) by γ-secretase in conjunction with β-secretase.
|
|
|
Which chromosomal abnormality results in Alzheimer disease? Why?
|
Down Syndrome. The APP gene is on chromosome 21, so Down syndrome patients will have more amyloid precursor protein, and thus more Aβ42 protein
|
|
|
What chromosome is APP (amyloid precursor protein) on?
What chromosome is Tau protein on? |
APP: 21
Tau: 17 |
|
|
What are the available pharmacological treatment options for Alzheimer disease?
|
Cholinesterase inhibitors
- rivastigmine - galantamine (also increases presynaptic release of ACh) - donepezil NMDA receptor antagonists (uncompetitive) - memantine |
|
|
What are the 3 chambers of the cochlea? What does each contain (perilymph or endolymph)?
|
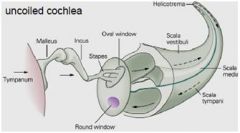
Scala vestibuli
• Contains perilymph Scala media • Contains endolymph Scala tympani • Contains perilymph |
|
|
What is the central bony core of the cochlea called?
|
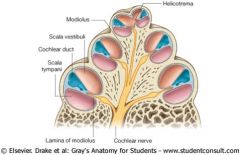
Modiolus
- Contains peripheral fibers and ganglion cells of auditory nerve |
|
|
What are the two types of spiral ganglion afferents of the auditory system?
|
Type 1 afferents
- 95% of the spiral ganglion - myelinated - synapses with inner hair cells Type 2 afferents - 5% - unmyelinated - synapse with outer hair cells |
|
|
Where do efferent fibers in the cochlear nerve originate from?
|
Superior olivary complex in the pons
- synapse on outer hair cells and afferent fibers of inner hair cells |
|
|
In the organ of Corti, do the stereocilia need to be deflected toward or away from the stria vascularis in order for depolarization to occur?
|
Toward stria vascularis
|
|
|
In the organ of Corti, what is the structure that sits on top of the sterocilia, and mechanically causes the sterocilia to bend called?
|
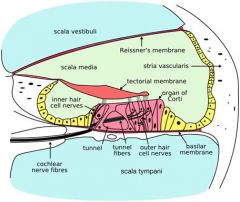
Tectorial membrane
|
|
|
Do low frequency sounds cause more of a deflection of sterocilia in organ of Corti at the base, or at the apex of the cochlea?
|
At the apex.
Conversely, high frequency sounds cause more deflection at the base. |
|
|
Where is the secondary auditory cortex?
|
Wernicke and Broca's areas.
|
|
|
What is the sequence of events in alcohol withdrawal?
|
1. Withdrawal symptoms
2. Seizures 3. Delirium tremens |
|
|
What is the average life expectancy after onset of Alzheimer disease?
|
8-10 years after onset.
|
|
|
What happens to the speech of the patient in delirium?
|
It becomes disorganized
|
|
|
Name the 5 layers of the cornea
|
Anterior epithelium
Bowman's membrane Substantia propria Descemet membrane Corneal endothelium |
|
|
Optic lens fiber proteins.
|
Crystallin
Filensin |
|
|
List the 10 layers of the retina, from inside to outside.
|
1. Internal limiting membrane
2. Nerve fiber layer 3. Ganglion cell layer 4. Inner plexiform layer 5. Inner nuclear layer 6. Outer plexiform layer 7. Outer nuclear layer 8. External limiting membrane 9. Outer segments of rods and cones 10. Retinal pigment epithelium |
|
|
What cells are contained in the inner nuclear layer of the retina?
|
Bipolar, amacrine, horizontal, Muller
|
|
|
What is the name of the visual pigment in rods? cones?
|
Rods - rhodopsin
Cones - iodopsin |
|
|
What is the area of highest visual acuity called on the retina?
|
It is the fovea centralis of the macula lutea. Has attenuated retinal layers, and contains many cones.
|
|
|
What is the difference between dry and wet forms of macular degeneration?
|
Dry macular degeneration - gradual accumulation of plaque underneath RPE, due to RPE degeneration.
Wet macular degeneration - growth of vessels from choroid into retina, causing bleeding and clotting. |
|
|
What are the 3 concentric layers of the eye?
|
From outermost to innermost:
1. Corneoscleral layer 2. Uvea (choroid, ciliary body, iris) 3. Retina |
|
|
What is the demarcation within the eyeball that separates the non-neural retina from the neural retina?
|
Ora serrata.
|
|
|
What is the fluid in the anterior and posterior chamber of the eyeball called?
What is the gel in the main ocular chamber called? |
Aqueous humor.
Vitreous body. |
|
|
What embryonic layer is each part of the eyeball derived from?
|
Ectoderm
□ Retina □ Lens □ Anterior epithelium of cornea Mesoderm □ Inner layer of cornea □ Choroid □ Sclera □ Ciliary body and iris |
|
|
What is the name of the sebaceous glands in the palpebral conjunctiva? What is their function?
|
Meibomian glands. They produce oily secretion that prevents rapid evaporation of tears.
|
|
|
Histological differences between a sympathetic ganglion and dorsal root ganglion.
|
Sympathetic ganglion
- eccentric nucleus - few satellite cells DRG - central nucleus - many satellite cells |
|
|
What is Parinaud syndrome?
|
1. Impaired vertical gaze
2. Large, irregular pupils 3. Eyelid abnormalities - lid retraction, or bilateral ptosis 4. Impaired convergence, sometimes convergence-retraction nystagmus Causes: pineal region tumors, hydrocephalus, compressing on dorsal midbrain and pretectal area. |
|
|
What is the effect of 5HT2A/5HT2C and 5HT3 antagonism?
|
5HT2A/5HT2C antagonists
• Weight gain • Anxiolytic • Antidepressant • Reduce sexual dysfunction • Sleep-restoring 5HT3 antagonism • Causes reduced nausea and GI upset |
|
|
Key signs/symptoms of Bell's palsy.
|
Left retroauricular pain.
Hyperacusis. LMN type facial weakness on one side. Painful, scratchy eye. |
|
|
What should be done to manage increased intracranial pressure?
|
• Head elevation
• Diuretics (such as mannitol) • Hyperventilation • Sedation/paralysis • Barbiturates • Surgery - CSF drainage - Evacuate the mass - Craniectomy |
|
|
What is the upper limit of a normal ICP in an adult?
|
15 mmHg
|

