![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
What does Bordetella Pertuisis need to survive?
|
Requires human respiratory tract (ciliated) - humans are the only carriers
or special agar (Nicotinamide & other stuff) to grow Gram (-) coccobacilli |
|
|
How does Bordetella grow?
|
Slowly (3-5d) in specialized medium
|
|
|
How is the diagnosis of bordetella pertusis made?
|
Diagnosis is made clinically and confirmed by the slow growing culture. (gram - coccobacilli)
Rapid DFA & serology can confirm clinical suspicion. Absolute lymphocytosis above 40K can aid in confirmation |
|
|
What are the adherence factors(4) & Toxins(4) of Bordetella Pertusis
|
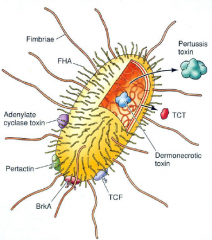
Adherence Factors (4) [PPPF]
Pilli=fimbrae Pertactin FHA (filamentous hemeagluttin) Pertusis Toxin - acts both as a toxin & an attachment factor Toxins (4) [PEAT] Tracheal Cytotoxin (TCT) (Dermonecrotic toxin) - destroys ciliary escalator ACT - activated by host CaM to raise cAMP & inhibits phagocytic cells Endotoxin (LPS) PT (see above) - inhibits Gi activation |
|
|
How does pertusis toxin work?
|
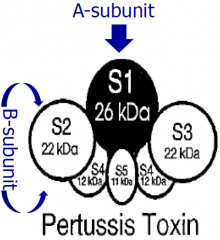
An AB toxin
S2-S5 act as B portion for uptake S1 is the A part - ADPR Inhibits the Gi function (increase in cAMP) |
|
|
Clinical signs of PT in blood?
|
Absolute lymphocytosis (40K)
Hypoglycemia |
|
|
What does Adenylate Cyclase Toxin (ACT) do?
|
[PAHCO]
[A]CT is a bacterial cyclase which is activated by host calmodulin to convert ATP->cAMP Some [h]emolysis activity. This **inhibits [p]hagocyte cells**, [c]hemotaxis, cell signaling & leads to 2y bacterial infections. Blocks formation of [o]xidative burst chemicals (PMN) |
|
|
What is and what does Tracheal CytoToxin (TCT) do? How does it compare to Endotoxin?
|
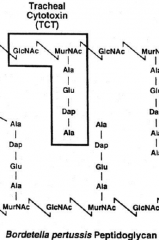
TCT - secreted fragemnted portions peptidoglycan layer of BP.
TCT - causes cytotoxicity of ciliated tracheal cells. This destroys the mucociliary escalator which takes 12wks to regrow. |
|
|
Where do you catch Whooping Cough? What is the infectivity rate? What is the reason for the recent resurgence?
|
1. Strict human pathogen. Some partially immunized adults carry but DO NOT have symptoms. They spread the pathogen
2. 80-100% infectivity rate to exposed. 3. Recent resurgence do to fear of vaccines |
|
|
Which Bordetella Pertussis Ag have antibodies(4)?
|
Ab form against FHA, PT, Pilli, Pertectin [FPPP]
?CMI is not stimulated possible reason requires boosters? |
|
|
Bordetella Pertussis
|
infection localized to UR tract & remains superficial binding to cilia. It does NOT directly invade.
Toxins rather than the bacteria will have systemic effects. |
|
|
What are the stages and Clinical symptoms of Bordetella Pertusis disease?
|

Overlapping phases
Catarrhal (1-2wks) - rhinorrhea, nonspecific malaise & fever this is when it is most communicable (flu like) Paroxysmal (2-4wks) - Cough 50x/day, coughing followed by whooping and occasional vomiting. Marker LYMPPHOCYTOSIS (>40k) Convalescent (3-4wks) - Cough decreases severity & frequency |
|
|
Can you treat whooping cough?
|
No, once the cough has started all therapy is supportive or to decrease spread to others.
Treat with erythromycin or clarithromycin. |
|
|
How does bordetella pertussis enter and cause diseases in humans? What does it secrete?
|
It is airborne, binds to ciliated respiratory epithelium via pertectin (PRN) + PT + FHA. This immobilizes the cilia. -> does NOT invade rather it superficially secretes
ACT - which causes hemolysis & disables PMNs PT - paralyzes PMN/macrophage, may stimulate insulin secretion, CAUSES lymphocytosis (>40K) TCT - Kills ciliated cells causing the persistent cough |
|
|
How can pertussis be prevented? How was the vaccine improved?
|
Vaccine is available that always uses purified Petussis Toxoid & FHA and some use Pernectin and Pilli. (Acellular)
The old vaccine used whole cells which had serious SE similar to GN shock |
|
|
What makes mycoplasma unique? What are it's growth requirements?
|
Does not stain. It has a trilaminar membrane with Sterols from the host/environment. It acts parasitic
Smallest self replicating bacteria that requires Special mycobacteria agar to slowly grow. |
|
|
How is mycoplasma pneumoniae spread? and to whom?
|
Only reservoir is humans. It is spread by few as 100 droplets, generally causing symptoms in 5-15yo's in close quarters (prisons, military)
|
|
|
How does mycoplasma pneumoniae enter the body?
|
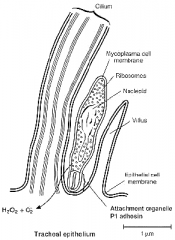
Binds to the cilia of bronchial epithelium. It then attaches at the base of the cilia using P1 tip attaching adhesion. This blocks the cilia function. This leads to desquamation and inflammation.
|
|
|
How does mycoplasma pneumoniae present in a patient?
|
atypical "walking" Pneumonia
2-4days of fever, HA & malaise. Physical exam will show patchy/unilateral pneumonia. Prior to respiratory symptoms of cough & mild tracheobronchitis. |
|
|
How is mycoplasma pneumoniae diagnosed? What is the culture appearance?
|
Gram stain of sputum show no organisms, or cells lacking cell wall. It requires special media cultures "fried egg appearance"
Serological tests are best, w/ a 4fold rise in the titer |
|
|
How is mycoplasma pneumoniae treated? Here does it persist?
|
No cell wall targeted drugs can be used. Erythromycin & tetracycline may shorten the duration but the bug may persist longer in the nasopharnyx.
|
|
|
How are bordetella pertusis and mycoplasma pneumoniae similar? Different?
|
Both bind to cilia in the trachea and move from there. Are spread by droplets.
Myco pneu produces no toxins Bord Pertus produces many toxins |
|
|
How does bordetella pertussis and mycoplasma pneumoniae immunity compare?
|
mycoplasma pneumoniae - host CMI may cause damage, the humoral immune response is induced. IgM, IgA and 2wks later IgG are formed. (may xreact-autoimmune w/ RBCs, brain, heart leading to anemia & systemic sx (arthritis))
Bordetella Pertussis - possibly uses CMI, IgG forms but will wane w/ time. 2nd infection will be more mild |
|
|
What are the mycoplasma that cause STDs? How are they spread? How are they differentiated from each other?
|
Ureaplasm urealyticum & Mycoplasma Hominis
spread through sexual contact. Ureaplasm urealyticum is identified by the production of urea. |
|
|
Describe the different manifestations of both unique mycoplasms in males? females?
|
1. men - urethritis, dysuria, urgency, & urethral discharge (Nongonococcal urethritis)
2. female - often asx but may have Salpingitis (Nongonococcal Salpingitis) |
|
|
What is the most common complication of Mycoplasma Pneumoniae?
|
CNS in about 25% of the cases
|
|
|
Is Xray alone enough to diagnose Mycoplasma Pnuemoniae? If not, what would be required?
|
No, though lower lobe Xray would be consistent with the disease. Xrays will show patchy/unilateral pneumonia.
Serology would confirm diagnosis. Stains are of little help with absence of a cell wall. |
|
|
What are the CXR findings in mycoplasma pneumoniae?
|
It often looks worse then the symptoms would suggest. Xrays will show patchy/unilateral pneumonia.
|
|
|
Is there a vaccine for mycoplasma pneumoniae?
|
No
|
|
|
What is hemagglutination?
|

Hemeagluttination is a specific form of agluttination of RBCs. Agluttination describes clumping.
It is used to diagnose mycoplasma pneumoniae. ???????????? |
|
|
Describe the mycoplasma pneumoniae bacteriology?
|
[CPRBC]
No [c]ell wall, marked [p]leomorphism, [r]esistant to [b]eta lactams, No gram stain. Have [c]holesterol in trilaminar membrane |
|
|
What are the common causes of atypical pneumoniae?
|
[MLCV]
mycoplasma legionella chlamydia viruses |
|
|
What are the different symptoms for atypical pneumoniae compared to classical pneumoniae?
|
????????????????
|
|
|
What population is most at risk for Whooping Cough?
|
Neonates, often mom's immunity has waned and does not transfer to the neonate. Vaccinations are given starting @ 2mo.
This is a dangerous window |
|
|
What are the major sequelae from whooping cough in neonates?
|
Life threatening in children w/ heart or lung problems. Otherwise neurological sequelae from hypoxia
|
|
|
How does TCT compare to Endotoxin?
|
Endotoxin is lipid A which is a part of the outer membrane in GN cells. TCT is from the peptidoglycan layer that is just deep to the outer membrane.
|

