![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
What are 2 subdivisions of GERD? |
1. Nonerosive reflux disease: sx without erosions on endoscopy 2. Erosive reflux disease: sx with erosions on endoscopy |
|
|
What are 3 typical symptoms of GERD? |
Heartburn (pyrosis), regurgitaton, acidic taste in mouth |
|
|
What are 7 atypical symptoms of GERD? |
Chronic cough, asthma-like symptoms, recurrent sore throat, laryngitis/hoarseness, dental enamel loss, noncardiac chest pain, sinusitis/PNA/bronchitis, otitis media |
|
|
What are 7 alarm symptoms of GERD? |
Dysphagia, odynophagia, bleeding, weight loss, choking, chest pain, epigastric mass: warrant immediate referral for invasive testing |
|
|
What are 5 aggravating factors of GERD? |
Recumbency (gravity), increased intra-abdominal pressure, reduced gastric motility, decreased LES tone, direct mucosal irritation |
|
|
What are 4 long-term complications of GERD? |
esophageal erosion, strictures/obstruction, Barret, reduction in QOL |
|
|
How can you make a presumptive diagnosis of GERD? |
Typical symptoms of heartburn and regurgitation (empiric PPI therapy recommended if patient has typical symptoms (strong/mod)) Screening for H. Pylori is NOT recommended Noncardiac chest pain that is suspected of having been caused by GERD need diagnostic eval before starting therapy |
|
|
When should endoscopy be performed in patients with GERD? |
Upper endo is NOT required is typical symptoms are present Recommended for alarm symptoms and in screening patients at high risk of complications Repeat endos not needed for Barrets if no new symptoms |
|
|
When should manometry be performed in patients with GERD? |
For preoperative evaluation but has no role in GERD diagnosis (strong/low) |
|
|
When should Am pH testing be performed in GERD? |
Esophageal reflux monitoring indicated B4 considering endoscopic/surgical therapy in nonerosive reflux disease as part of the eval of patients refractory to PPI therapy and in situations where GERD is in question Am reflux monitoring is the only test than can assess reflux sx association Am reflux monitoring NOT required in presence of short-or long-segment Barrett esophagus to establish GERD diagnosis |
|
|
Evidence for non-pharm management in GERD |
AGA guidelines cite insufficient evidence for lifestyle modifications for all patients (advocate use in target pops) -Dietary mod if assoc with food or drink -Weight loss if overweight/recent weight gain -Reduce/DC nicotine use (affects LES) -Elevate HOB/avoid meals 2-3 hours before bedtime if nocturnal symptoms -Avoid tight-fitting clothing (dec. IAb pressure) |
|
|
Foods that lower LES pressure |
Alcohol, caffeine, chocolate, citrus juice, garlic, onions, peppermint, spearmint |
|
|
Direct irritation |
Spicy foods, tomato juice, coffee |
|
|
Medications that reduce LES pressure, delay gastric emptying, direct irritation |
a-adrenergic antagonists, anticholinergics, BZD, CCB, estrogen, nitrates, opiates, TCA, theophylline, NSAID, ASA |
|
|
Initial GERD treatment (depends on severity, freq, duration of sx) |
Step down: start with maximal therapy (therapeutic PPI dose): OK for documented esophageal erosion +: rapid sx relief, avoidance of over-investigation -: potential over-tx, higher cost, increased AE Step-up: start with lower-dose OTC +: avoid over-tx, lower initial cost -: potential under-tx, partial sx relief, long sx contol |
|
|
AGA GERD Tx Guidelines |
Erosive esophaitis treated with 8 week course of PPI (no major product diff) -maint PPI is return of sx or complications -bedtime H2RA can be used in AM PPI and nightime sx but tachyphylaxis develops -Further testing before metoclopramide/baclofen |
|
|
AGA GERD Dosing Guidelines |
Traditional PPIs given 30-60 mins before meals -Newer PPIs offer dosing flexibility in relation to meals -Initiate PPI once daily before AM meal -BID PPI is partial response to Qday PPI and/or nighttime sx -BID is partial response to Qday or switch to another PPI |
|
|
Antacids for GERD MOA |
-Neutralize acid and raise IGastric pH leads to deactivation of pepsinogen/inc. LES pressure -Rapid onset but short duration (frequent dosing) -Ca, Al, Mag |
|
|
Alginic acid |
-Gaviscon -Forms viscous layer on top of gastric contents to act as barrier to reflux (variable added efficacy) |
|
|
Efficacy of antacids for GERD |
1st line for intermittent (less than twice weekly) symptoms or as breakthrough for those on PPI/histamine therapy -not appropriate for healing established erosions |
|
|
Antacids Adverse reactions |
Constipation (Al); diarrhea (Mag); accumulation of al/mag in renal disease with repeat dosing |
|
|
Antacids DDI |
Chelation: FQ, TC Reduced resorption b/c of pH increase: ketoconazole, itraconazole, iron, atazanavir, delviridne, indinavir, nelfinavir Increased absorption leading to potential tox: raltegravir, saquinavir |
|
|
H2RA MOA GERD |
Reversibly inhibit H2RA on parietal cell All available as Rx and OTC Generics available for all |
|
|
Available H2RA products |
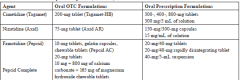
|
|
|
Available H2RA products |
|
|
|
Uses for GERD H2RA |
-On demand therapy for intermittent mild-mod GERD sx -Preventive dosing before meals or exercise -Higher Rx doses for more severe sx or maintenance dosing -Prolonged use associated with tolerance/reduced efficacy (tachyphylaxis) -Less efficacious than PPI for erosive esophagitis |
|
|
AE of H2RA |
Most are well-tolerated -HA, dizzy, fatigue, somnolence, confuson -Caution elderly/renal -Cimetidine with gynecomastia if long use |
|
|
H2RA DDI |
Absorption of drug dependent on lower gastric pH: ketocon, itracon, PPIs, -cimetidine: inhibits CYP450 -Warfarin, theophylline may be affected -Cimetidine competes with meds and creatinine for tubular secretion in kidney |
|
|
PPI MOA |
irreversibly inhibit final step in gastric acid secretion, more acid suppression and longer DOA than H2RA -most effective for short/long-term management of GERD and erosive dx -more effective before meals: give evening dose before evening meal instead of bedtime |
|
|
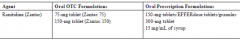
PPI products |

|
|
|
Adverse reactions PPI |
HA, dizzy, nausea, diarrhea, constipation Long-term: sig increases in endocrine neoplasia of sx Vit B12 deficiency -recommended in 2013 AGA guidelines: switch off in AE |
|
|
Risk of Fx PPI managment |
-Should not affect decision unless risk factors for hip fx -Patients with OP can remain on PPI -Limit dose/duration -Ensure adequate Ca and Vit D -BMD screening if at risk of low bone mass -Weight bearing exercise |
|
|
Hypomag PPI risk |
Re-eval if neeed Limit dose/duration Baseline testing if on diuretic/dg -Supplement |
|
|
C diff PPI management |
Re-eval if needed Limit dose/duration -Eval for C diff if PPI and diarrhea not improving |
|
|
CAP PPI management |
Short-term use can increase risk; long-term risk not eval -assess for vaccine status |
|
|
PPI DDI |
-Inhibition of CYP450: omeprazole inhibits met of substrates through 2C19 -clopidogrel (use pantoprazole): 2013 AGA state NOT sig clinically -high-dose IV MTX: risk of MTX toxcity (Avoid PPI, switch to ranitidine if needed); avoid PPI dose 2 days before or after MTX admin -pH-dependent absorption: ketoconazole, Protease inhibitors |
|
|
GERD promotility agents |
-DO NOT use without eval -Options: baclofen, prokinetics --> work through cholinergic mechanism to faciliate increased gastric emptying |
|
|
Metoclopramide GERD |
Dopamine antagonist Several times a day dosing AE: dizzy, fatigue, drowsy, EPS, hyperprolactinemia -GERD and gastroparesis |
|
|
Bethanechol GERD |
Cholinergic agonist; many AE (diarrhea, blurred vision, abdom cramping) possible inc gastric acid production |
|
|
Cisapride GERD |
Restrcted use Cardiac arrhytmias, TDP if used with CYP3A4 inhibitors |
|
|
Major causes of duodenal ulcers |
H Pylori NSAIDs Low dose ASA Uncommon: Zollinger-Ellison syndrome, high Ca, granulomatous diseases, neoplasia, infections (CMV, herpes, TB), ectopic pancreatic tissue |
|
|
S/S of duodenal ulcer |
Epigastric pain (maybe worse as night), pain is 1-3 hours after a meal; may be relieved by eating Pain may be episodic Assoc sx: HB, belching, bloated, nausea, anorexa |
|
|
Causes of
Gastric ulcer |
NSAIDS, H Pylori Uncommon: CD, infections |
|
|
Clinical S/S of Gastric ulcer |
Epigastric pain---worse with eating; associated symptoms include heartburn, belching, bloated, nausea, anorexia |
|
|
Complications of PUD (3) |
Bleeding Gastric outlet obstruction Perforation |
|
|
Patients at risk of NSAID-induced GI toxicity |

|
|
|
Which NSAIDs are less intrinsically toxic to GI than naproxen (which is moderate risk) |
ibuprofen, diclofenac, nabumetone High risk: ketorolc, piroxicam |
|
|
What is the duration of NSAID use that contributes to risk of GI stuff |
higher risk in first 3 moths RA, CV disease can contribute to GI toxicity of NSAIDS H Pylori infection can confer risk of GI toxicity |
|
|
Diagnosis of PUD: H Pylori infection |
Symptom presentation Must treat if test --test with active ulcer disease, history of PUD, gastric mucosa-associated lymphoid tissue lymphoma --test and treat acceptable for patients with unevaluated dyspepsia who have no alarm symptoms and are younger than 55 |
|
|
Invasive endoscopic testing for H Pylori |
-Histology: Very sensitive and specific -Rapid urease test (CLO test): detects presense of NH3 in a sample generated by H Pylori urease activity (False negs if partially treated infection, GI bleeds, achlorhydria, use of PPIs/H2/bismuth in past month); stop anti-secretory agents I week before doing test -Culture: 100% specific though costly and time consuming |
|
|
Noninvasive serologic H pylori testing |
Detects IgG to H pylor in serum by ELISA: cannot distinguish between active infection and past exposure -Abodies persist long after eradcation Antibody testing not affected by antibiotics or PPIs |
|
|
Noninvasvie urea breath test |
Detects exhalation of radiolabeled CO2 after the ingestion of radiolabeled urea -97% sen 95% spec -diangosis and test for eradication -recent use of AB or PPIs may result in FN in up to 40% of patients -Stop antisecretory agents 2 week before testing or wait 4 weeks after treatment has ended |
|
|
Noninvasive stool antigen test |
Diagnosis and confirm eradication -FN with PPI/antibiotics -stop 2 weeks before or test 4 weeks after |
|
|
General Tx guidelines of H Pylori per ACG |
-PPI -2 antibiotics (clarithyromycin and amox or metro) -Duration on 7-14 days (preferred 14 days) -Follow up testing for eradication: history of ulcer complaints, gastric MALT, early gastric cancer, recurrence of sx |
|
|
Preferred H Pylori eradication confirmation |
UBTs Stool antigen tests -wait 4 weeks after treatment for both |
|
|
Quadruple based therapy for H Pylori |
Bismuth, metronidazole, TC and a PPI x 14 days if triple therapy fails or if patient has intolerance or allergy of triple drug therapy |
|
|
Pylera components |
Quadruple-based therapy -TC, bismuth, metronidazole in 1 capsule |
|
|
Sequential therapy for H Pylori |
PPI and amoxicillin are given for 5 days followed by PPI, clarithromycin, and tinidazole for additional 5 days -needs further validation in literature |
|
|
Salvage H Pylori therapy |
Bismuth-based quadruple therapy for 14 days or a LF based triple therapy for 10 days for patients who have not responsed to initial regimen |
|
|
Chart of H Pylori regimens |
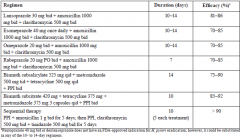
|
|
|
Primary prevention of NSAID-induced ulcers by ACG guidelines |
-Implement risk factor modification -TEST AND TREAT for H PYLORI is beginning long-term NSAID therapy -Determine level of GI related risk (low, med, high) -Also determine CV risk (high risk CV: patients who require low-dose ASA for cardiac event prevention) -Naproxen is onl NSAID that does not inc CV risk |
|
|
Prevention strategies for NSAID-related GI complications and CV risk |

|
|
|
Misoprostol dosing for NSAID risk |
Full dose of 800 mcg/day in divided doses; poorly tolerated due to NVD and cramping |
|
|
NSAID and antiplatelet concomitant use ACCF guidelines |
-Need for AP therapy evaluated first -If needed: assess for GI risk factors (including dyspepsia and GERD) -T/T for H Pylori in patients with history of nonbleeding ulcer and/or ulcer related complications (optimal to eradicate H Pylori before beginning long-term AP therapy) |
|
|
What are preferred gastroprotective agents for tx and prevention of ASA and NSAID GI injury? |
PPIs |
|
|
Who should receive gastroprotective therapy |
Patients with GI risk factors who require use of any NSAID (including OTC and COX2) in conjunction with cardiac-dose ASA GI risk factors who require preentive dose of ASA (do not use doses > 81 mg/day) |
|
|
PPIs should be prescribed for patients receviing |
concomitant ASA and anticoagulant therapy (UFH, LMWH, warfarin, NOACs, fondaparinux) |
|
|
Target INR for patients for whom warfarin is added to ASA and plaix |
2-2.5 |
|
|
What is superior to clopidogrel for recurrent ulcer bleeding |
ASA + PPI |
|
|
How long should elective endoscopy be deffered after DES |
1 year |
|
|
Treatment/secondary prevention of NSAID ulcer |
Risk factor modifcication Discontinue or lower dose if possible Test for H Pylori and treat if present |
|
|
Drug therapy for treatment/prevention of NSAID ulcer |
PPIs are DOC Misoprostol: as effective as PPIs for healing/preventon--multidoses and poorly tolerated H2RAs are inferior to PPIs and misoprostol |
|
|
Vimovo |
Esomeprazole + naproxen (375/20 or 500/20) |
|
|
Celecoxib for treatment/prevention of NSAID ulcer |
-High rate of ulcer recurrence/bleeding comparable with diclofenac + omeprazole combo -Limited by its recent assoc with CV effects -Uncertain if use of low dose ASA + celecoxib for 2ndary prevention of GI events -Combo of COX2 + PPI is not well studied (could be considered in high-risk pts if they required continued NSAID or ASA use) -Dose related response to toxicitiy |
|
|
Stepwise approach for CV patients needing NSAID |
-APAP, ASA, tramadol, or short-term nacs -Non-acetylated salicylates -Non COX-2-selective NSAIDs next -NSAIDs with some COX2 -COX-2 inhibitors laast --consider PPI -Monitor BP, renal fcn, edema, GI bleeding |
|
|
Lower risk NSAIDs for GI bleeding risk |
Ibuprofen, etodolac, diclofenac, celecoxib |
|
|
Taking ibuprofen and ASA together |
Ibuprofen taken 30 mins after or 8 hours before ASA to prevent interaction |
|
|
Causes of upper GI bleeding |
PUD (NSAID vs H Pylori) Esophagitis Erosive disease Esophageal varices MW tear Neoplasm Stress ulcers (crtically ill) |
|
|
S/S of upper GI beed |
Hematemeis "coffee-ground" Hematochezia NV Melena Shock (tachycardia, clammy skin) Hypotension Associated organ dysfunction (renal/hepatic/cardiac/cerebral hypoperfusion) |
|
|
Initial mangement of ulcer-related GI bleeding |
-Volume resuscitation and HD stabilize -1 or 2 large bore IV catheters -Crystalloid NS preferred (blood if hb <7 to maintain Hb 8-10) -endoscopy within 24 hours |
|
|
Clinical scoring scales for upper GI bleed |
Blatchford or Rockwall scores --> determines risk of early rebleeding and need for urgent vs nonurgent interventon |
|
|
Endoscopic therapy for upper GI bleed |
-12 to 24 hours of presentation -Combo of injection and coaptive therapy is most efficacious approach -Sclerotherapy -Thermal coaptive therapy (heater probe, laser coagulation) -Hemostatic clips |
|
|
PPI for upper GI bleed |
pre-endoscopic dose (80 mg IV bolus) followed by 8 mg/hr IV infusion -no mortality affect or rate of rebleeding -reduces lesion size and need for endoscopic therapy -CI is for 72 hours after endo therapy for pts with active bleed -Once Qday for patients with flat spot or clean based ulcer |
|
|
Should upper GI bleed be tested for H Pylori? |
Yes: and treat if positive results IF neg: restest No need for PPI after eradication |
|
|
Should oral PPI be used as secondary prevention? |
Possibly: if needed, single daily oral dose |
|
|
Should NSAIDs be D/C? |
Possibly: assess for NSAID and ASA use; PPI + COX2 recommended (unless CV risk) -Reinitiate ASA when CV risk > GI risk -Clopidogrel bleed rate > ASA |
|
|
What is long-term PPI therapy recommended for? |
Ulcers not associated with NSAIDs or H Pylori |
|
|
What are contributors to SRMD development? |
Hypoperfusion of GI tract Altered susceptibility to gastric acid Loss of defense mech: bicarb layer/PGI/cell renewal Alterations in gastric motility; affects drug absorption |
|
|
Pharm prevention for SRMD |
Not routinely recommended in non-ICU settings See risk factors for ICU |
|
|
Risk factors for initiating of SRMD prophylaxis |
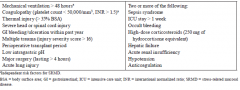
|
|
|
Preventive Tx Options for SRDM |
-Antacids:raise pH and prevent rebleeding (diarrhea, constipation, elyte problems) -Sucralfate: direct mucoal layer/mods pepsin/use fallen out of favor/binds drugs in GI tract (efficacy similar to H2RA) -H2RA: efficacy with prevention; high dose IV can be used for 1st line therapy (cimetidine only FDA approved--->thrombocytopenia, renal dyscn dose adjust |
|
|
PPI for SRMD |
Most commonly used; little data Similar to H2 in S/E Oral or IV used or NG Oral is equivalent to IV PPI for maintaining pH -IV PPI = high dose IV H2RA -Possible C diff associations? |

