![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
313 Cards in this Set
- Front
- Back

|
|
|
|
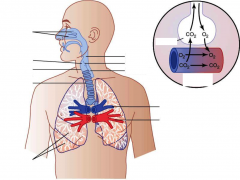
Respiratory process:
moving air into and out of the lungs |
Pulmonary ventilation
|
|
|
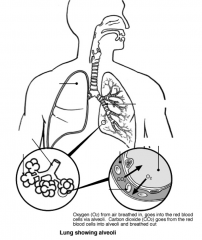
Respiratory process:
gas exchange between the lungs and blood |
External respiration
|
|
|
Respiratory process:
transport of oxygen and carbon dioxide between the lungs and tissues |
Transport
|
|
|
Respiratory process:
gas exchange between systemic blood vessels and tissues |
Internal respiration
|
|
|
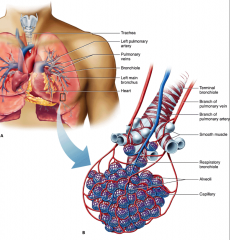
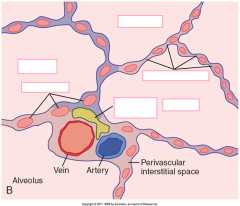
Pulmonary Blood Flow:
- From aorta, 2% of cardiac output - Bronchial veins drain into pulmonary veins - Do not take part in gas exchange "physiological shunt" |
Bronchial arteries
|
|
|
Pulmonary Blood Flow:
- Bring deoxygenated blood from right ventricle |
Pulmonary arteries
|
|
|
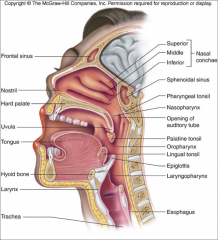
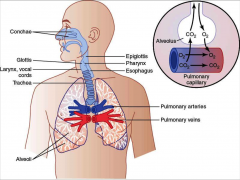
Functions as HME
|
Nose
|
|
|
Provides 100% humidification and warming of inspired air
|
nose
|
|
|
Filtration level of nasal hairs
|
Up to 6 micrometer particles
|
|
|
What can occur while inserting nasal tubes
|
bleeding due to increased vascularity
|
|
|
common effect of tracheostomy insertion
|
lung crusting and infection
|
|
|
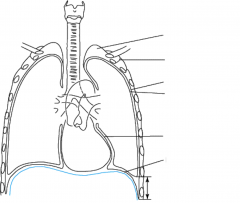
Lung has _______ right lobes, ________ left lobes
|
3 right
2 left |
|
|
negative pressure in the lungs pleural space
|
-5 cm H2O
|
|
|
If air introduced into pleural space, what occurs
|
negative pressure in lung removed, lung collapses (pneumothorax)
|
|
|
Disease that destroys elasticity of lung tissues
|
Emphysema
|
|
|
Causes decreased inward recoil, leading to barrel shaped chest
|
Emphysema
|
|
|
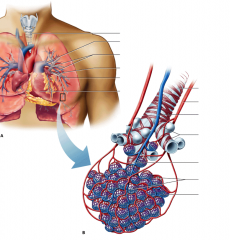
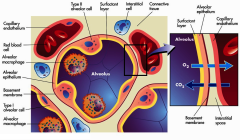
Alveolar capillary flow is from the ___________ end to the _____________ end
|
venous to arterial end
|
|
|
Excess PEEP can cause what to capillary flow?
|
Causes a choke point which can block capillary flow preventing External respiration. (no gas exchange)
|
|
|
Approx. distance between RBC and aveoli
|
0.3 - 0.7 = ~ 0.6 micrometers
|
|
|
What produces surfactant?
|
Type 2 alveolar cell
|
|
|
Total surface area of alveoli
|
~ 70 m^2
|
|
|
Six components of membrane
|
- alveolar fluid lining (contain surfactant)
- alveolar epithelium - epithelial basement membrane - interstitial space - capillary basement membrane - capillary endothelial membrane |
|
|
Reduction of what indicates disrupted alveolar capillary surface?
|
Diffusion Capacity of lung for Carbonmonoxide (DLCO)
|
|
|
True / False:
DLCO is abnormal in emphysema and interstitial fibrosis with destruction of lung parenchyma |
True
|
|
|
If breathing 500 cc
________ stays in conducting zone ________ reaches respiratory zone (alveolar sacs) |
150 stays in conductive zone
350 reaches respiratory zone (alveoliar sacs) |
|
|
Gas that stays in the conducting zone during respiration is called
|
Waste (in dead space)
|
|
|
Respiratory Tree:
Consists of nose, pharynx, trachea, bronchi, bronchioles, and terminal bronchioles. Cartilage is present only in the trachea and bronchi. Brings air in and out. Warms, humidifies, filter air. Anatomic dead space. Walls of conducting airways contain smooth muscle |
Conductive Zone
|
|
|
Respiratory Tree:
Consists of respiratory bronchioles, alveolar duct, and alveoli (300 millions in each lung). Participate in gas exchange |
Respiratory Zone
|
|
|
Warming and moistening the air is also known as
|
Airconditioning
|
|
|
~ number of alveoli in each lung
|
300 million (total of 600 million in both)
|
|
|
Name for cilia lining trachea
|
Pseudo stratified columnar cilia
|
|
|
mucous secreting cells in trachea that have sacs
|
Goblet cell
|
|
|
Combined action of cilia and goblet cells in trachea
|
Mucociliary clearance
|
|
|
Called "house keepers" of respiratory epithelium
|
Cilia
|
|
|
What causes cough when smoker quits smoking
|
Cilia "waking up"
|
|
|
Why more foreign bodies to right lung?
|
Right bronchiole wider and more in-line with trachea
|
|
|
Often missed diagnosis when patient presents with wheezing
|
foreign body aspiration (asthma usually assumed)
|
|
|
Describe sequence of events during Inspiration (6)
|
1) Inspiratory muscles contract (diaphragm descends; rib cage rises)
2) Thoracic cavity volume increases 3) Lungs are stretched; intrapulmonary volume increases 4) Intrapulmonary pressure drops (to -1 cm H2O) 5) Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure) |
|
|
Describe sequence of events during Expiration (5)
|
1) Inspiratory muscles relax (diaphragm rises; rib cage descends due to recoil of costal costal cartilages)
2) Thoracic cavity volume decreases 3) Elastic lungs recoil passively; intrapulmonary volume decreases 4) Intrapulmonary pressure rises (to +1 cm H2O) 5) Air (gases) flows out of lungs down its pressure gradient until intrapulmonary pressure is 0 |
|
|
Inspiratory Muscle
- Most important muscle for inspiration - Acts like a piston; when it contracts, the abdominal contents are pushed downward, the rib are lifted upward and outward, increasing the volume of thoracic cavity |
Diaphragm
|
|
|
What nerve innervates the diaphragm
|
Phrenic nerve
|
|
|
At what area does the phrenic nerve arise?
|
C3, C4, C5
* C3,4,5 keeps the diaphragm alive |
|
|
Where can pain from the diaphragm be referred to?
|
Shoulder
|
|
|
Which muscles are not used for inspiration during normal quiet breathing?
|
External intercostals
scalene sternomastoids |
|
|
Inspiration is an ____________________ process
|
active process
|
|
|
Expiration is normally a _________________ process
|
Passive process
|
|
|
What are the expiratory muscles? (4)
|
- rectus abdominis
- internal / external oblique - transversus abdominis - internal intercostal |
|
|
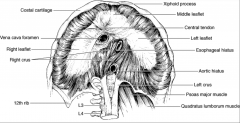
Structure perforating the diaphragm
At T8 |
IVC
|
|
|
Structure perforating the diaphragm
At T10 |
esophagus, vagus
|
|
|
Structure perforating the diaphragm
At T12 |
aorta, thoracic duct and azygous vein
|
|
|
most important muscle of inspiration
|
diaphragm
|
|
|
Diaphragm accounts for ~ _______% of TV during normal quiet respiration
|
75%
|
|
|
Factors that ___________ Dead Space
a. Pulmonary vascular diseases b. Pulmonary Embolism c. COPD d. ARDS e. Pulmonary fibrosis f. Shock g. Old age h. Positive pressure ventilation |
Increase Dead Space
|
|
|
Factors that ____________ Dead Space
a. Artificial airways (due to narrow diameter) |
Decrease Dead Space
|
|
|
Formula for Dead Space:
|
Vd = Vt x PaCO2 - PeCO2 / PaCO2
Vd = physiological dead space Vt = Tidal Volume PaCO2 = PCO2 of arterial blood PECO2 = PCO2 of expired air |
|
|
The volume of conducting airways where no gas exchange occur
|
Anatomical dead space (normally 150, 2 ml/kg)
|
|
|
volume of air that enters non-perfused or poorly perfused alveoli. Normally = zero
|
Alveolar dead space
|
|
|
volume of lung that does not participate in gas exchange
|
Physiological dead space
|
|
|
Is approximately equal to the anatomical dead space in normal lung
|
Physiological dead space
|
|
|
May be greater than the anatomical dead space in lung disease, in which there are V/Q inequalities (shunting or alveolar collapse)
|
Physiological Dead Space
|
|
|
Sum of all exhaled gas volume in 1 minute
|
Minute ventilation
|
|
|
equation for minute ventilation
|
MV = TV x RR = 5 L/min
|
|
|
Volume of inspired gases actually taking part in gas exchange in 1 minute
|
Alveolar ventilation
|
|
|
________ indicates alveolar ventilation
|
PCO2
|
|
|
Equation for alveolar ventilation
|
alveolar ventilation = (tidal volume-dead space) x breaths/min
|
|
|
Pleural pressure is negative in pleural space because lung recoils ______________ and chest wall recoils ____________
|
lungs recoil inward
chest wall recoils outward |
|
|
At FRC the inward and outward forces are
|
equal
|
|
|
Alveolar pressure is normally ______
|
0 cm H2O
|
|
|
Alveolar pressure ________ in inspiration and
________ in expiration |
decreases in inspiration
increases in expiration |
|
|
Transpulmonary Pressure =
|
alveolar P - Pleural P
|
|
|
First breath of neonates generates transpulmonary pressure of _______ to _______ cm H2O
|
40 - 80 cm H2O
|
|
|
Resting Pleural Pressure:
|
-5 cm H2O
|
|
|
Inspiration Pleural Pressure:
|
-8 cm H2O
|
|
|
Resting Alveolar Pressure:
|
0 cm H2O
|
|
|
Inspiration Alveolar Pressure:
|
-1 cm H2O
|
|
|
Expiration Alveolar Pressure:
|
+1 cm H2O
|
|
|
What is used to measure pleural pressure?
|
Balloon catheter in the esophagus
|
|
|
Lung volume is the _________
|
FRC
|
|
|
What happens to the pressure gradient between the atmospheric and alveoli during inspiration?
|
Air flows into the lungs until the pressure gradient dissipates
|
|
|
During inspiration pleural pressure becomes _______________
|
more negative than at rest
(-5 to -8 cm H2O) |
|
|
At peak of inspiration, lung volume is FRC plus one _____
|
FRC plus one TV
|
|
|
Alveolar pressure becomes __________ during normal (passive) expiration
|
more positive during expiration
compressed by elastic forces of the lung. Pressure gradient reversed |
|
|
During normal (passive) expiration, intrapleural pressure _________
|
returns to its resting value
|
|
|
During forced expiration, intrapleural pressure ___________
|
intrapleural pressure becomes positive
|
|
|
This positive intrapleural pressure during forced expiration makes expiration _______________
|
more difficult because it compresses the airways
|
|
|
Why are COPD patients instructed to breath with "pursed lips"?
|
Airway resistance is increased in COPD, breathing slowly through pursed lips to expire slowly prevents airway collapse that may occur with forced expiration
|
|
|
During expiration lung volume ___________
|
lung volume returns to FRC
|
|
|
As elasticity increases, compliance ________________
|
decreases
|
|
|
As Elasticity decreases, compliance ________________
|
increases
|
|
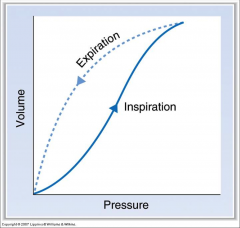
The lung has the most compliance _____________
|
at the middle region after inspiration already started
|
|
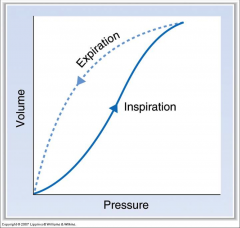
The lung has the lowest compliance _________________
|
At the beginning and end of inspiration
|
|
|
Shows "distensibility" of lungs and chest wall
|
Lung compliance
|
|
|
True or False:
Compliance is opposite to stiffness |
True
|
|
|
Lung compliance is the slope of the _____ _____ curve
|
Pressure - Volume Curve
|
|
|
Change in volume of lung for each unit change in pressure (transpulmonary pressure)
|
Compliance
(ex: 200 mL/cm H2O) |
|
|
True or False:
Compliance of lung-chest wall system is less than that of the lungs alone or chest wall alone ( the slop is flatter) |
True
|
|
|
At FRC the collapsing force of the lungs and expanding force are ___________________
|
equal and opposite (equilibrium)
|
|
|
Steel has very high _________________
|
elasticity
|
|
|
In patient with ________________ lung compliance increased and the tendency of the lung to collapse is decreased
|
Emphysema
|
|
|
In patient with ___________________ the tendency of lungs to collapse is less than the tendency of the chest wall to expand
|
emphysema
|
|
|
In patient with ________________ the lung-chest wall system seeks a new, higher FRC so that the two opposing forces can be balanced
|
emphysema (results in barrel-shaped chest)
|
|
|
In patient with ________________ lung compliance is decreased and the tendency of lungs to collapse is increased
|
fibrosis
|
|
|
In patient with __________________ the tendency of the lungs to collapse is greater than the tendency of the chest wall to expand
|
fibrosis
|
|
|
Causes of _______________ Lung Compliance
High expanding pressures Increased Pulmonary venous pressure Fibrosis (deposition of collagen) Lack of surfactant |
Decreased Lung Compliance
|
|
|
Causes of ________________ Lung Compliance
Emphysema (destruction of elastic fibers) Old Age |
Increased Lung Compliance
|
|
|
Equation for alveoli pressure relating to radius and surface tension
|
P = 2T/r (Laplace's Law)
|
|
|
____________________ results from the attractive forces between molecules of liquid lining the alveoli
|
Surface Tension of alveoli
|
|
|
In absence of ______________ small alveoli have tendency to collapse
|
surfactant
|
|
|
Surfactant is secreted by ____________________
|
Type 2 alveolar cells
|
|
|
Surfactant is composed of _________________ (3)
|
- phospholipid
- proteins - Ca++ |
|
|
Disrupts intermolecular forces between the molecules of liquid-act like "detergent"
|
Surfactant
|
|
|
Reduction in surface tension by surfactant does what to compliance
|
increases compliance
|
|
|
Lecithin / Sphingomyelin (L/S) ration of what in amniotic fluid indicates fetal lung maturation?
|
L/S ratio > 2:1
|
|
|
Surfactant synthesis starts at _________ wks gestation
|
24 wk gestation
|
|
|
Occurs in premature infants because of lack of surfactant. The infant shows atelectasis (lung collapse), difficulty reinflatting the lungs( as a result of decreased compliance) and hypoxemia because of V/Q
� |
Neonatal respiratory distress syndrome
|
|
|
Treatment for Neonatal resp. distress syndrome?
|
maternal steroid before birth (speeds up surfactant formation in babies, also artificial surfactant to infants by inhalation)
|
|
|
causes granular "ground glass" appearance of lung parenchyma, correlating to moderate to severe retractions and oxygen dependence in premature infants
|
resp. distress syndrome RDS
|
|
|
Airflow equation
|
Q = delta P / R
Q = airflow deltaP = pressure gradient R = airway resistance |
|
|
Resistance to flow equation
|
R = 8nl / pie r^4
|
|

|

|
|
|

|
|
|
|
|
|
|
|

|

|
|

|

|
|

|

|
|
|

|
|

|
|
|

|

|
|
|

|
|

|

|
|

|

|
|

|

|
|

|

|
|

|
|
|

|

|
|

|

|
|

|

|
|

|

|
|
|
Law describing the sum of the partial pressures of all gases in a mixture equals the total barometric pressure
|
Dalton's Law
|
|
|
reflects the amount of oxygen gas dissolved in the blood. It primarily measures the effectiveness of the lungs in pulling oxygen into the blood stream from the atmosphere.
� |
Partial Pressure of Oxygen
|
|
|
Following conditions associated with:
- increased oxygen levels in inhaled air - Polycythemia |
Elevated PO2 levels
|
|
|
Following conditions associated with:
- Decreased oxygen levels in the inhaled air - Anemia - Heart decompensation - Chronic obstructive pulmonary disease - Restrictive pulmonary disease - Hypoventilation |
Decreased PO2 levels
|
|
|
Number of iron-containing heme groups per hemoglobin?
|
4
|
|
|
Iron form which binds O2
|
ferrous (Fe++)
|
|
|
Normal adult hemoglobin structure
|
alpha2beta2
|
|
|
Following relate to what?
- Is the maximum amount of O2 that can be bound to Hb in blood at 100% saturation - Is depend on Hb conc. in blood - Limits the amount of O2 that can be carried in blood |
O2 binding capacity of blood
|
|
|
Following relate to what:
- Is the total amount of O2 in blood, including bound and dissolved O2 - Depends on the Hb concentration, PO2 and P50 of Hb |
O2 content of blood
|
|
|
Equation for oxygen content
|
O2 content = (O2 binding capacity x %Sat.) + Dissolved O2
%Sat = % of heme groups bound to O2 Dissolved O2 = unbound O2 in blood |
|
|
Normally 1g Hb can bind _________ ml O2
|
1.34 ml O2
normal Hb = 15g/dL |
|
|
Cyanosis results when deoxygenated Hb > _________ g/dL
|
5 g/dL
|
|
|
O2 binding capacity = _________ ml O2/dL
|
20.1 ml O2/dL
|
|
|
True or False:
O2 content of arterial blood decreases as Hb falls, but O2 saturation and arterial PO2 do not |
True
|
|
|
Oxygen delivery to tissue =
|
O2 delivery to tissue = cardiac output x O2 content of blood
|
|
|
Nitrites, benzocaine, metabolites of prilocaine can cause ________________
|
methemoglobinemia
|
|
|
Methemoglobin does not bind to O2 as readily, but has Increased affinity for ________
|
Increased affinity for CN-
|
|
|
Treatment for methemoglobinemia
|
IV methylene blue, converts ferric (Fe+++) to ferrous (Fe++) form
|
|
|
2 For Us
|
Ferrous (Fe++) is the good iron form
|
|
|
Following are causes of:
- Nitroprusside (releases CN ions) - Bitter almond oil - KCN - Wild cherry syrup |
Cyanide Poisoning
|
|
|
S/S of _____________:
- Tachycardia - Hypotension - Coma - Acidosis - Venous O2, rapid death |
Cyanide Poisoning
|
|
|
Treatment for cyanide poisoning
|
sodium nitrite and amyl nitrites to oxidize Hb to metHb (inducing methemoglobinemia) which binds to cyanide, allowing cytochrome oxidase enzyme to go free and function
|
|
|
_______________ binds to cyanide, forming thiocyanate, which is excreted by kidneys
|
thiosulfate
|
|
|
Oxygen carried in blood in two forms
1. Bound to Hb _______% in RBCs 2. Dissolve form ________% in plasma |
97% in RBC
3% in plasma |
|
|
Which form of O2 produces the partial pressure in blood?
|
Dissolved form in plasma
|
|
|
Hb combines rapidly and 'reversibly' to form with O2 to form ____________________
|
oxyhemoglobin
|
|
|
________________ is the driving force for the chemical reaction
Hb + O2 <-> HbO2 |
O2 tension
(increased PO2 increases affinity of Hb for O2) |
|
|
At PO2 of 40 mmHg, Hb is ______% saturated
|
75%
|
|
|
At PO2 of 25 mmHg, Hb is ______% saturated
|
50%
|
|
|
P50 is what
|
PO2 at 50% saturation
|
|
|
term describing change in affinity of Hb as each successive O2 molecule binds to a heme site
|
positive cooperativity
|
|
|
When the oxygen hemoglobin curve is LEFT shifted, the affinity of Hb is _______________
|
higher
|
|
|
When the oxygen hemoglobin curve is RIGHT shifted, the affinity of Hb is ________________
|
lower
|
|
|
Below PO2 of _________ free fall of saturation
|
60 mmHg
|
|
|
Conditions that shift curve to right (decrease affinity)
C A D E T |
Increased:
C O2 A cidity D PG - diphophoglycerate product of glycolysis E xercise T emperature |
|
|
Shift the curve to right, decreases the affinity of Hb for O2 and facilitating the unloading of O2 in the tissues
|
Bohr Effect
Ex: During exercise, the tissues produce more CO2, which decreases tissue pH (H+) and, through the Bohr effect, stimulates O2 delivery to the exercising muscle. |
|
|
Fetal hemoglobin HbF, shifts curve to the __________
|
left
|
|
|
affinity for Hb for CO is _______ x than O2
|
250x
|
|
|
Binding of CO to Hb _____________ the affinity of remaining sites for O2,
|
increases affinity -> causing shift of the curve to the left, decreases unloading in tissues (brain)
|
|
|
CO poisoning with have a ______________ PO2
|
normal PO2, no cyanosis
|
|
|
S/S of __________________:
- headache - vertigo - dyspnea - confusion - dilated pupil - convulsion and coma |
CO poisoning
|
|
|
Treatment for CO poisoning
|
100% O2 (will bump off CO from Hb)
|
|
|
major form of CO2 carried to lungs
|
HCO3-
|
|
|
2 small forms of CO2 carried to lungs
|
carbaminohemoglobin (Hb CO2)
Dissolved CO2 |
|
|
In RBC CO2 combines with H2O to form ___________
|
H2CO3
|
|
|
HCO3- leaves RBC in exchange for _______ and transported to lungs in the plasma
|
Cl- (chloride shift)
|
|
|
Effect describing:
Blood carries more CO2 when PO2 decreases Blood carries less CO2 when PO2 increases |
Haldane Effect
|
|
|
Interact with the medullary respiratory centers to smooth the respiratory pattern
|
Pontine respiratory centers
|
|
|
Contains rhythm generators whose output drives respiration
|
Ventral respiratory group (VRG)
|
|
|
Integrates peripheral sensory input and modifies rhythms generated by the VRG
|
Dorsal respiratory group (DRG)
|
|
|
Higher brain centers, voluntary control over breathing
|
Cerebral cortex
|
|
|
Respiratory centers
|
medulla and pons
|
|
|
breathing receptors of pain and emotional stimuli acting through the ___________________
|
hypothalamus
|
|
|
True or False:
H+ ions in blood are able to stimulate Brain Respiratory chemoreceptor |
FALSE
H+ in blood are not able to cross blood/brain barrier. CO2 must cross barrier to form H+ in CSF |
|
|
Normal healthy adult breaths via what stimulation
|
PCO2 drive
|
|
|
Sensory information is coordinated in ________________ to send signals to respiratory muscles
|
Brain Stem
(PCO2, lung stretch, irritants muscle spindles ,tendons and joints) |
|
|
Located in the reticular formation
|
Medullary Respiratory Center
|
|
|
Called the "pacemaker" of medullary respiratory center
|
Dorsal Respiratory Group
|
|
|
Component of medullary respiratory center:
- inspiratory control - receive inputs via vagus and glossopharyngeal nerve - output to diaphragm via phrenic nerve |
Dorsal Respiratory Group
|
|
|
Component of medullary respiratory center:
- expiratory control - efferent via internal intercostal nerve - work only during exercise, when expiration becomes an active process. |
Ventral Respiratory Group
|
|
|
DiVe
|
Dorsal (inspiratory)
Ventral (expiratory) |
|
|
Control of Breathing:
Located in pons Stimulates inspiration , producing deep and prolonged inspiratory gasp (apneusis) |
Apneustic Center
|
|
|
Control of Breathing:
- Located in upper pons - Inhibits respiration, and therefore, inspiratory volume and respiratory rate. Adjust rate and depth of respiration |
Pneumotaxic Center
|
|
|
Control of Breathing:
- voluntary breathing; hypoventilation or hyperventilation |
Cerebral cortex
|
|
|
Chemoreceptor control:
- Sensitive to pH of CSF decreases - Not sensitive to increase in H+ in blood |
Central Chemoreceptors in Medulla
|
|
|
True or False:
Acidosis and alkalosis does not effect central chemoreceptors |
True
|
|
|
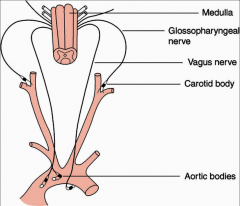
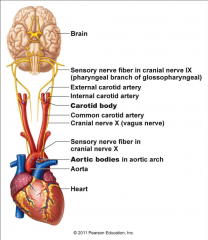
Chemoreceptor control:
- Sensitive to decreased PO2 - Sensitive to increased PCO2 - Sensitive to decreased pH (increased H+ concentration) |
Peripheral chemoreceptors in the carotid and aortic bodies
|
|
|
Receptors responsible for hypoxic drive to respiration
|
Peripheral chemoreceptors in carotid and aortic bodies
|
|
|
Control of Breathing:
- Afferent via vagus nerves - when these receptors are stimulated by distention of the lungs, they produce a reflex in breathing frequency |
Stretch receptors
(HERING-BREUER REFLEX) (located on bronchial walls) |
|
|
Control of Breathing:
- Engorgement of pulmonary capillaries in LVH, stimulates these receptors, which then cause rapid, shallow breathing dyspnea |
J (juxtacapillary) receptors
|
|
|
Stimuli that increase breathing for which receptor:
decreased pH increased PCO2 |
Central Chemoreceptor (medulla)
|
|
|
Stimuli that increase breathing for which receptor:
decreased PO2 (<60 mmHg) increased PCO2 decreased pH |
Peripheral Chemoreceptor (carotid and aortic bodies)
|
|
|
Abnormal Respiratory Pattern:
- Hypersensitivity of resp center to CO2 - Period of waxing and waning of tidal volumes separated by periods of apnea - Drug overdose, CHF, hypoxia |
Cheyne-Stokes Respiration
|
|
|
The association of sleep apnea with extreme obesity is referred to as _______________________
|
Pickwickian Syndrome
(Obesity-hypoventilation syndrome) |
|
|
Clinical signs of what condition?
- Partial airway obstruction causes snoring - Hypoxia-- decreased PO2 - Rarely hypercapnia - Polycythemia - Poor sleep at night - Daytime sleepiness |
Pickwickian Syndrome
|
|
|
Treatment of Pickwickian Syndrome
|
Oropharyngeal appliances
Positive pressure nasal mask Surgery |
|
|
Area of the lung:
Lowest Blood flow |
Apex
|
|
|
Area of the lung:
Lower ventilation |
Apex
|
|
|
Area of the lung:
Higher V/Q |
Apex
|
|
|
Area of the lung:
Highest regional arterial PO2 |
Apex
|
|
|
Area of the lung:
Lower regional arterial PCO2 |
Apex
|
|
|
Area of the lung:
Highest Blood Flow |
Base
|
|
|
Area of the lung:
Higher Ventilation |
Base
|
|
|
Area of the lung:
Lower V/Q |
Base
|
|
|
Area of the lung:
Lowest regional arterial PO2 |
Base
|
|
|
Area of the lung:
Higher regional arterial PCO2 |
Base
|
|
|
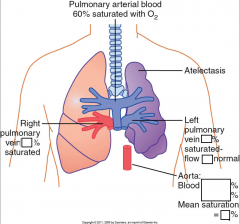
V/Q = ?
airway obstruction (shunt). |
V/Q = 0
|
|
|
V/Q = ?
blood flow obstruction |
infinity
|
|
|
In an airway obstruction (shunt), does 100% oxygen improve PO2?
|
No
|
|
|
In a blood flow obstruction, does 100% oxygen improve PO2?
|
Yes (assuming <100% dead space)
|
|
|
If the frequency , TV and CO are normal , the V/Q is approximately ___________
|
0.8
(Normal V = 4L/min and normal Q=5L/min) (apex > 1.0, base < 0.8) |
|
|
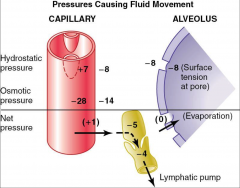
Outward Forces Causing Fluid movement:
Capillary pressure ________ mmHg Interstitial osmotic pressure __________ mmHg Negative interstitial pressure __________ mmHg |
Capillary pressure 7 mmHg
Interstitial osmotic pressure 14 mmHg Negative interstitial fluid pressure 8 mmHg |
|
|
Inward Forces Causing Fluid movement:
Plasma protein osmotic pressure ________ mmHg |
Plasma protein osmotic pressure 28 mmHg
|
|
|
Mean Filtration Pressure _________ mmHg
|
1 mmHg
|
|
|
pO2 of:
Dry Inspired Air |
160
|
|
|
pO2 of:
Humidified Tracheal Air |
150
(addition of H2O decreases PO2) |
|
|
pO2 of:
Alveolar Air |
100
(O2 has diffused from alveolar air into pulmonary capillary blood, decreasing the PO2 of alveolar air) |
|
|
pO2 of:
Arterial Blood |
100*
(Blood has equilibrated with alveolar air, is "arterialized") |
|
|
pO2 of:
Venous Blood |
40
(O2 has diffused from arterial blood into tissue, decreasing the PO2 of venous blood) |
|
|
PCO2 of:
Dry inspired air |
0
|
|
|
PCO2 of:
Humidified Tracheal Air |
0
|
|
|
PCO2 of:
Alveolar Air |
40
(CO2 has been added from pulmonary blood into alveolar air) |
|
|
PCO2 of:
Arterial Blood |
40
(Blood has equilibrated with alveolar air) |
|
|
PCO2 of:
Venous Blood |
46
(CO2 has diffused from the tissue into venous blood, increasing the PCO2 of venous blood) |
|
|
Lack of normal surfactant, as occurs in infants with respiratory distress syndrome, results in:
A. Increase lung compliance B. Stabilization of alveolar volume C. Increases retractive forces of the lungs D. Decrease filtration forces in the pulmonary capillaries |
C, increases retractive forces of the lungs
|
|
|
During inspiration, as the diaphragm contracts, the pressure in the interpleural space becomes
A. Equal to zero B. More positive C. More negative D. Equal to pressure in alveoli E. Equal to pressure in atmosphere |
C, more negative
|
|
|
The volume/amount of gas in the lungs at the end of a normal expiration is referred as
A. Residual Volume B. Expiratory reserve volume C. Functional residual capacity D. Inspiratory reserve volume E. Total lung capacity |
C, Functional Residual Capacity
|
|
|
The vital capacity is the sum of the
A. RV, TV,ERV B. RV,TV,IRV C. ERV,IRV,TV D. RV,ERV,IRV |
C, ERV, IRV, TV
|
|

|
|
|

|

|
|

|
|
|

|

|
|
|
Intravenous lactic acid increases ventilation. The receptor responsible for this effect are located in the_________
A. Medulla Oblongata B. Carotid bodies C. Aortic baroreceptor D. Lung parenchyma |
B. Carotid Bodies
|
|
|
Primary stimulus for carotid bodies is
A. H+ B. Low concentration of O2 C. High concentration of CO2 D. HCO3- |
B. Low concentration of O2
|
|
|
Indications for ___________________
- apnea, inadequate ventilation - severe hypoxemia despite O2 supplementation - airway protection - in coma |
Mechanical Ventilation
|
|
|
Precautions with what?
- pt with PO2 <= 55mmHg - Hypoxic drive suppression - oxygen toxicity - parenchymal damage |
Supplemental O2
|
|
|
Respiratory Responses to Exercise:
O2 consumption |
increased
|
|
|
Respiratory Responses to Exercise:
CO2 production |
increased
|
|
|
Respiratory Responses to Exercise:
Ventilation rate |
increased
|
|
|
Respiratory Responses to Exercise:
Arterial PO2 and PCO2 |
no change, B2 effect
|
|
|
Respiratory Responses to Exercise:
Arterial pH |
No change in moderate, ex decreased in strenuous
|
|
|
Respiratory Responses to Exercise:
Venous PCO2 |
increased
|
|
|
Respiratory Responses to Exercise:
Pulmonary blood flow |
increased
|
|
|
Respiratory Responses to Exercise:
V/Q ratio |
more evenly distributed
|
|
|
Respiratory Responses to Exercise:
Blood flow to skeletal muscle |
Increased, B2 effect, vasodilation
|
|
|
Respiratory Responses to Exercise:
HR, SV, CO |
Increased B1 effect
|
|
|
Adaptation to High Altitude:
Alveolar PO2 |
Decreased
|
|
|
Adaptation to High Altitude:
Arterial PO2 |
Decreased
|
|
|
Adaptation to High Altitude:
Ventilation rate |
Increased
|
|
|
Adaptation to High Altitude:
Arterial pH |
Increased (kidney resolves initial low pH)
|
|
|
Adaptation to High Altitude:
Hb concentration |
Increased
|
|
|
Adaptation to High Altitude:
2,3 DPG |
Increased (catabolic effect to right shift)
|
|
|
Adaptation to High Altitude:
Hb-O2 curve |
Shift to right, decreased affinity, increased P50
|
|
|
Adaptation to High Altitude:
Pulmonary vascular resistance |
Increased (Hypoxic Vasoconstriction)
|
|
|
During Forced Exhalation, the intrapleural space pressure increases from -8 to _________
|
+30
|
|
|
True or False:
Forced exhalation collapses airway and increases resistance |
True
|
|
|
Following are released by what during asthma episode:
- Heparin - Histamine - SRSA (slow reacting substance of anaphylaxis) - ECF (eiosinophilic chemotaxic factor) - Bradykinin |
Mast cells
|
|
|
Exposure to antigen -> formation of ______
|
IgE
|
|
|
40@40 = emergency
|
hyperventilation with high or even normal PCO2 is respiratory emergency
|
|
|
Reversible airway obstruction by contraction of smooth muscle of bronchioles
|
Asthma
|
|
|
Seen by airway wall thickening from inflammatory cell infiltration, airway edema, increased mucus secretion, subepithelial fibrosis and increased smooth muscle mass
Also may be loss in linkage between the airway wall and the surrounding tethering elements of the alveoli |
Airway remodeling
|
|
|
Symptoms of asthma:
|
- wheezing
- cough - dyspnea - chest discomfort |
|

|
|
|

|

|
|

|

|
|
|
Destruction of alveolar walls and abnormal enlargement of air spaces distal to terminal bronchiole
|
Chronic Pulmonary Emphysema
|
|
|
Causes of _________________:
- SMOKING - chronic infection - chronic obstruction - decrease diffusion capacity -> CO2 retention - V/Q mismatch -> hypoxia and hypercapnia - Pulmonary hypertension -> RHF "cor pulmonale" |
Chronic Pulmonary Emphysema
|
|
|
With COPD, lung-hyperinflation and Cor Pulmonale, heart may be what shape?
|
teardrop-shaped
|
|
|
Pathogenesis of What:
Upon long-term exposure to cigarette smoke, inflammatory cells are recruited to the lung; they release proteinases in excess of inhibitors, and if repair is abnormal, this leads to airspace destruction and enlargement or emphysema. |
Emphysema
|
|
|
___________________:
have mild hypoxemia and because they maintain alveolar ventilation, normocapnia (normal PCO2) |
"Pink Puffers" (primarily emphysema)
|
|
|
__________________:
have severe hypoxemia with cyanosis and because they do not maintain alveolar ventilation, hypercapnia ( PCO2). The have right ventricular failure (right heart has to work harder against scarred lung) and systemic edema |
"Blue Bloaters" (primarily bronchitis)
|
|
|
Term for fibrotic lung condition:
- Rales - cough - infiltration and fatal fibrosis |
Bleomycin Lung
|
|
|
________________________
MCC: - pneumococci (G+ Diplococci in pairs) |
Pneumonia
|
|
|
Filling of alveoli with fluid and cellular debris
|
Consolidation
|
|
|
_______________________:
- droplet infection - obligate aerobes - commonly in lung apex |
Tuberculosis
|
|
|
______________________:
- Due to an inactivating mutation in the BMPR2 gene (normally functions to inhibit vascular smooth muscle proliferation) - Poor prognosis |
Primary Pulmonary Hypertension
|
|
|
________________________:
- Due to COPD (destruction of lung parenchyma) - Mitral stenosis ( resistance pressure) - Recurrent thromboemboli ( cross-sectional area of pulmonary vascular bed) - Autoimmune disease (e.g. systemic sclerosis ; inflammation intimal fibrosis medial hypertrophy ) - Left-to-right shunt ( shear stress endothelial injury ) - Sleep apnea or living at high altitude (hypoxic vasoconstriction) |
Secondary Pulmonary Hypertension
|
|
|
Progression of ____________________:
Severe respiratory distress cyanosis and RVH DEATH from decompensated cor pulmonale |
Secondary Pulmonary Hypertension
|
|
|
5 Causes of Hypoxia?
|
1. Decreased CO
2. Hypoxemia (decreased PaO2 -> decreased %Sat) 3. Anemia 4. CO poisoning 5. Cyanide poisoning |
|
|
Causes of ___________________:
- Salicylate toxicity - Sepsis - Excess mech. ventilation - hyperventilation (blowing off too much CO2) |
Respiratory Alkalosis
|
|
|
Symptoms of ____________________:
- Lightheadedness - Circumoral numbness - Paresthesias - Tetanus (ionized calcium --alkalosis--> bound form) |
Respiratory Alkalosis
|
|
|
Most PE's originate from _________
|
DVT in leg
|
|
|
Non-thrombotic pulmonary emboli (3)
|
- Septic-> endocarditis in IV drug abusers, infected catheters
- Fat (long bone fractures) - Amniotic fluid (during child birth) |
|
|
Pathological consequence of _____________________:
- increased pulmonary vascular resistance - increased pulmonary artery pressure - increased RV afterload |
PE
|
|
|
S/S of ______________________:
- Dyspnea - Pleuritic chest pain - SOB - Signs of RV overload (loud P2, RV heave) - Look for signs of DVT - Homan - warmth, swelling - 50% have no symptoms |
PE
|
|
|
ABG with __________________:
- Resp. alkalosis - Decreased PCO2 - pt hyperventilating - Hypoxemia - Increased O2 A-a gradient |
PE
|
|
|
Found with ________________:
- Pulmonary artery end diastolic pressure > pulmonary artery occlusive pressure |
PE
|
|
|
Gold standard for _________________:
Pulmonary angiography |
PE
|
|
|
PE Anticoagulation: (3)
|
1. Heparin (PTT) 1.5-2.5 x normal = 30 sec
2. Warfarin, coumadin (PT) (12 sec) 3. Thrombolytic therapy - streptokinase, tPA (high risk, only with life threatening PE) |
|

|

|
|

|

|
|
|

|
|
|
Asthma pathway
|
Exposure -> formation of IgE -> IgE attaches to mast cells -> re-exposure to the antigen -> Mast cells release
- Heparin - Histamine - ECF - SRSA - Bradykinin |

