![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
17 Cards in this Set
- Front
- Back
|
Cytokines related to bone formation |
-Osteoblast 에서 RANKL, MCSF 분비 (osteoclast 촉진) -OPG 는 osteoclast 억제 |
|
|
Parathyroid Hormone (PTH) |
-Dominant regulator of PTH is plasma Ca. -Vit D inhibits PTH expression. -PTH is not directly regulated by phosphate level.
--> Main action is to increase plasma Ca. |
|
|
Physiological Action of PTH |
Kidney: -increase Ca reabsorption -reduce phosphate reabsorption -stimulate vit D production
Bone: -short term: promote Ca movement into the extracellular luid -long term: stimulates osteoblasts to produce RANKL.
Indirect action: Increase Ca and phosphate absorption in the intestine (results from increased vit. D).
결국 최종 효과는 Ca 양 증가, Phosphate 일정. |
|
|
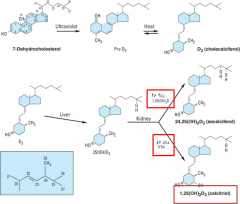
Vitamin D |
Principal regulator of Ca: increases Ca absorption from the intestine.
-Vit D itself is inactive. Requires 1, 25 hydroxylation. -24 hydroxylation makes it inactive. -PTH stimulates 1α-hydroxylase and increase 1,25-dihydroxy D. -Phosphate inhibits 1α-hydroxylase and hypophosphatemia stimulates the 1α-hydroxylase activity.
|
|
|
Vit D production regulation |
|
|
|
Synthesis of Vit. D |
-D3 가 Liver 로 와서 25번에 hydroxylation 이 된다. 신장에서 추가로 1번에 hydroxylation 이 되면 active form 이 된다. -Vit D 가 많거나 Ca, 인이 많다면 feedback 으로 1aH 의 효과가 작아지고 24H activity가 증가하면서 vit D 활성이 줄어든다. |
|
|
Physiological Action of Vit D |
**Mechanism of action: The main action is to stimulate Ca2+ absorption from the intestine
-In intestine: By binding to vitamin D receptor (VDR), it modify gene expression Ca binding proteins and channels, etc. -In kidney: a. Ca reabsorption in distal tubules b. P reabsorption in proximal tubules c. In bone, using VDR in osteoblasts, it produces proteins to activate osteoclasts to resorb Ca2+ in bone d. Inadequate supply of vitamin D leads to rickets (bone deformation) -Vitamin D-dependent rickets type I – defects in 1α hydroxylase -Vitamin D-dependent rickets type II – defects in VDR
*VDR deficiency-induced rickets can be restored by Ca supplementation; Effect of calcitriol on bone is secondary to increased Ca |
|
|
Calcitonin |
*Hypocalcemic hormone (opposite of PTH) -Synthesized and secreted by the parafollicular cells of the thyroid gland -Major stimulus of secretion is a plasma Ca rise -The most potent peptide inhibitor of osteoclast-mediated bone resorption
*Mech of action -Direct inhibition of osteoclastic bone resorption -In kidney, calcitonin inhibit Ca and P reabsorption
-Removal of parafollicular cells does not cause hypercalcemia -Chronic excess of calcitonin does not produce hypocalcemia: PTH and Vitamin D3 dominate the Ca regulation
|
|
|
Ca lv 항상성 유지 |
Ca 이 떨어지면 PTH 가 작용을 하고 Ca 이 높으면 thyroid 에서 calcitonin이 나와서 Ca level 을 낮춘다. 이렇게 항상성이 유지되고 있다 . |
|
|
Glucocorticoid |
-Antagonize vitamin D-stimulated intestinal calcium transport -Stimulate renal calcium excretion -Bone resorption -Suppress osteoblast function and increase osteoclast function by RANKL production -Secondary to the rise of PTH by reduced Ca uptake |
|
|
Estrogen |
-Directly affect osteoblast/clast ER to enhance bone formation -Suppress the bone-resorbing action of PTH -Estrogen administration leads to increase vitamin D in blood secondarily by decreased Ca and P and increased PTH -Clinically useful in the treatment or prevention of postmenopausal osteoporosis
|
|
|
Biphosphonates |
–Analogs of pyrophosphate –Chelating divalent cation (Ca) –A strong affinity for bone (Targets Ca to bone remodeling sites)
–Mechanism of action: a. Suppress osteoclast function by: –Osteoclast apoptosis: 1st generation »Metabolized to nonhydrolyzable ATP analog –Inhibition of cholesterol biosynthesis: aminobisphosphonates (2nd)
–Toxicity: •Esophageal and Gastric irritation = oral form of bisphosphonates –Circumvented by infusion of zoledronate: markedly reduces the frequency of administration |
|
|
Different Generation of Biphosphonates |
2nd generation = aminobiphosphonates 3rd generation = 10X more potent; Zoledronate
Indications: -Osteoporosis -Paget's Disease -Hypercalcemia -Cancer |
|
|
Non-Hormonal eg) Calcimimetics (=cinacalcet) |
-mimics the stimulatory effect of Ca to inhibit PTH secretion by activating Ca-sensing R. -toxicity: hypocalcemia -clinical use: secondary hyperparathyroidism in chronic kidney disease.
|
|
|
Osteoporosis |
-80 % genetic, 20 % environmental
Primary Osteoporosis = Post-menopausal Secondary Osteoporosis = Systemic illness (Paget's disease), glucocorticoids |
|
|
Therapeutic agents for osteoporosis |
#1. Inhibitor of Bone Resorption *Bisphosphonates -Prevention and treatment -Most effective -2nd, 3rd generation *Estrogen -Prevention -Heart disease and breast cancer – short term use *Raloxifene (SERM) -Estrogen partial agonist, inactive in uterus, anti-estrogen in breast prevention and treatment -Reduced side effect but worsen vasomotor symptom *Thiazides -lower dose than in anti-hypertensive -useful in hypercalciuria *Calcium *Vitamin D and analogs -increase Ca absorption -reduce parathyroid function *Calcitonin -Treatment less effective than BPP, hPTH *Denosumab -RANKL inhibitor -Comparable to the potent bisphosphonates #2. Stimulator of bone formation-PTH: its intermittent use increases bone density.-Adverse Effect: incidence of bone tumor (osteosarcoma) cf) Combination Therapy: The use of both anti-resorptive and anabolic agents is less effective than monotherapy alone. Combination therapy is reserved for a fracture during therapy with a single drug. |
|
|
Hypercalcemia |
Life threatening: central nervous system depression
*Causes -Primary hyperparathyroidism (high PTH) – most common -Ingestion of large quantities of Ca in hyperthyroid patients -Milk-alkali syndrome
*Treatments -Loop diuretics – Ca excretion with volume reduction -Corticosteroids – increase Ca excretion, decrease Ca absorption -Calcitonin – decrease bone resorption -Bisphosphonates – very effective, inhibit osteoclasts activity
|

